

Hello,
Dr. Batman
Hello Doctor, Welcome!
Profile

Name: Batman
Email: batman@gotham.com
CARDIOLOGY
(Total Questions - 217)Q.1. A 66 year old man presents to the hospital with palpitations. An ECG taken shows atrial fibrillation. He has no history of any ischaemic heart diseases. His blood pressure is 110/70 mmHg, heart rate is 130 beats/minute and respiratory rate is 20 breaths/minute. He looks sweaty on examination. His chest is clear clinically on auscultation. What is the most appropriate management?
Correct Answer : A
Rate control medications such as metoprolol should be given first as he is hemodynamically stable. If rate control medications fail, then we could try rhythm control. Digoxin as part of rate control should not be used as first-line unless there is evidence of congestive heart failure. Remember, the most important part of management for atrial fibrillation is preventing strokes and controlling the patient’s symptoms. Converting patients back to sinus rhythm is not always the main goal.
The clinical presentation of atrial fibrillation can vary. Some patients are asymptomatic; others may have life-threatening complications (e.g. heart failure or angina). The management depends on the underlying cause and the presence of symptoms.
There are two wide categories for management:
1. Rhythm control (cardioversion)
2. Rate control
Rhythm Control : If the patient has signs of shock, syncope, acute cardiac failure, or ischaemia then perform electrical cardioversion under sedation. This is rarely necessary. There is also the option of chemically cardioverting with flecainide or amiodarone. If the patient has had symptoms for more than 48 hours, there is a risk of cardiac thromboembolism when cardioverted. So in these cases, rate control medications and low molecular weight heparin are better choices.
Rate control medications include beta blockers (metoprolol), rate-limiting calcium channel blockers (diltiazem or verapamil), and digoxin.
For rate control, beta-blockers or rate-limiting calcium channel blockers are the first choice. Digoxin 500 mcg is usually the choice of drug if the patient suffers from congestive heart failure.
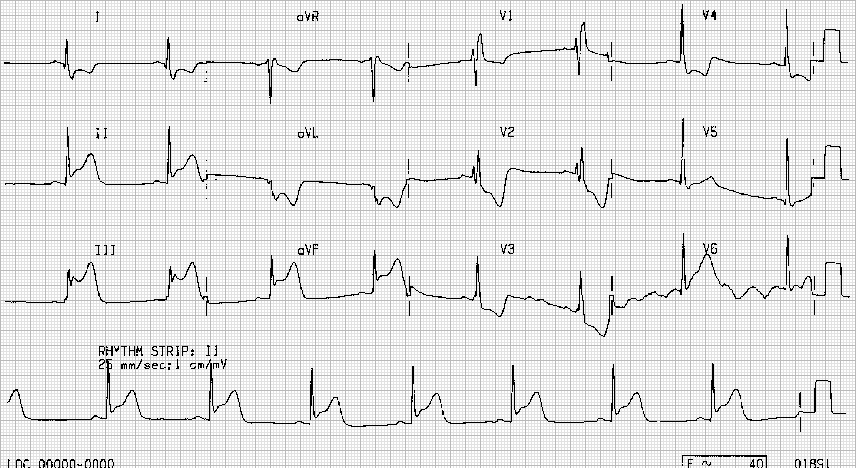
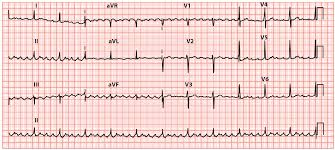
Q.2. A 55 year old man has sudden onset of central chest pain and shortness of breath 3 hours ago. He looks pale and sweaty. An ECG was done in the Emergency Department and is seen below. What is the most likely diagnosis based on this ECG?

Correct Answer : B
This could be potentially a case of a myocardial infarction. A new LBBB in the context of cardiac chest pain is traditionally considered part of the criteria for thrombolysis. It is extremely important to recognize an LBBB on an ECG.
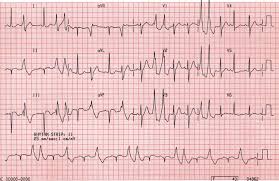
Q.3. Which of the following may cause the abnormalities of the QRS axis shown on this ECG?
Correct Answer : D
A common cause of left axis deviation is inferior myocardial infarction.
Remember, this question does not ask if this is an inferior myocardial infarction hence the ECG does not show the typical ST elevation in leads II, III, and aVF. This question is asking, what abnormalities could represent a left axis deviation of which inferior myocardial infarction is the only option.
Common causes of left axis deviation (LAD) : Left ventricular hypertrophy (LVH), Left anterior fascicular block (or hemiblock), Inferior myocardial infarction.
Less common causes of left axis deviation (LAD) : Obesity, Wolff Parkinson White syndrome.
Causes of right axis deviation : Right ventricular hypertrophy, Thin tall, Chronic lung disease, Pulmonary embolism, Left posterior hemiblock, Lateral myocardial infarction.
The lateral wall of the left ventricle is supplied by the left anterior descending. Infarction here would cause an axis deviation away from the site of infarction.
Q.4. A 60 year old man had a myocardial infarction 2 weeks ago. He now presents with dyspnoea and pleuritic chest pain. A pericardial friction rub was noticed on examination. ECG shows widespread ST elevation. A chest x-ray shows an enlarged, globular heart. His pulse rate is 95 beats/minute and his respiratory rate is 24 breaths/minute. What is the most likely cause of his symptoms?
Correct Answer : B
The widespread ST elevation and pericardial friction rub are seen in pericarditis. The chest X-ray showing an enlarged, globular heart points towards pericardial effusion.
Dressler’s syndrome would explain all the findings. Dressler’s syndrome tends to occur around 2-6 weeks following an MI.
The underlying pathophysiology is thought to be an autoimmune reaction against antigenic proteins formed as the myocardium recovers. It is characterized by a combination of fever, pleuritic pain, pericardial effusion, and a raised ESR. It is treated with NSAIDs.
Q.5. A 62 year old man has a routine ECG pre-operatively for an elective osteoarthritic knee replacement. He is in sinus rhythm, and the WRS complex is not prolonged. There is a gradual prolongation of the PR interval, followed by a dropped beat every 3 or 4 QRS complexes. The ECG machine is unable to calculate the PR interval. The patient does not complain of any palpitations. What is the most likely diagnosis?
Correct Answer : C
Mobitz type 1 block : Gradual prolongation of the PR interval followed by a dropped beat. 1st degree heart block is a prolongation of the PR interval (beyond 0.2 seconds). It is a benign condition that does not require additional follow-up or management. It is not usually associated with symptoms and does not progress to other forms of heart block. The PR interval is measured from the beginning of the P wave to the beginning of the QRS complex.
Mobitz type 2 and complete heart block require permanent pacemakers.
Q.6. A 68 year old woman is brought into the Emergency Department with palpitations and chest discomfort. She gives a history of left hemiparesis four days ago which has partially resolved after a few hours. She has a blood pressure of 160/95 mmHg, respiratory rate of 22 breaths/minute and a heart rate of 120 beats/minute. A CT scan of the head was organised which shows evidence of a small cortical infarct. An ECG taken in the Emergency Department shows absent P waves and an irregularly irregular rhythm with a variable ventricular rate. Metoprolol was given intravenously and she was discharged once asymptomatic. Which long term medications is she likely to benefit from?
Correct Answer : A
The patient has been diagnosed with atrial fibrillation. The symptoms of stroke were probably due to atrial fibrillation. The main goals in managing AF are rate/rhythm control and anticoagulation.
As she was already managed with metoprolol which is a rate-limiting medication, the next step is to count her CHA2DS2-VASc score to determine if she requires anticoagulation. In her case, she would have a CHA2DS2-VASc score of 4 (1 for hypertension, 1 for age, 1 for stroke history, and 1 for sex). Anticoagulation such as warfarin would be of benefit to reduce the risk of stroke for her. Aspirin is no longer used for stroke prevention.
ATRIAL FIBRILLATION AND ANTICOAGULATION :
Guidelines suggests using the CHA2DS2-VASc score to determine the most appropriate anticoagulation strategy for atrial fibrillation.
The CHA2DS2-VASc score is used to assess a patient’s stroke risk. Offer anticoagulation to all people with a CHA2DS2-VASc of 2 or above, and consider offering it to men with a CHA2DS2-VASc of 1.
Risk factor : C - Congestive heart failure, 1 H - Hypertension, 1 A2 - Age 75 years , 2 Age 65-74 years, 1 D Diabetes, 1 S2 Prior stroke or TIA 2 V Vascular disease (including ischaemic heart disease and peripheral arterial disease), 1 S Sex (female). It may be quicker to remember when to give warfarin according to the below scenarios instead of writing out and calculating the whole CHA2DS2-VASc score.
This only applies to simple exam scenarios.
• < 65 years old and no comorbidities - No warfarin
• 65 years old or at least one comorbidity - Warfarin
Another alternative to warfarin which has gained much popularity over the past decade is DOAC (Direct-Acting Oral Anticoagulants) such as apixaban, edoxaban, and rivaroxaban. These medications are also licensed for use in stroke prevention with non-valvular atrial fibrillation and a CHA2DS2-VASc score 2 (consider for men with CHA2DS2-VASc score 1).
The benefits of using DOAC compared to warfarin include :
• Reduces the risk of intracranial haemorrhage
• No INR monitoring
• Faster onset anticoagulation (2-4 hours)
The disadvantages of using DOAC compared to warfarin include:
• No specific antidote
• Essential to be compliant
Newer questions for the exam may contain DOAC as an option so do read up on them.
SECONDARY PREVENTION AFTER STROKE OR TIA :
Stroke: A syndrome of the sudden onset of focal neurological loss of presumed vascular origin lasting more than 24 hours.
Transient Ischaemic Attack: A syndrome of the sudden onset of focal neurological loss of presumed vascular origin lasting less than 24 hours.
Q.7. A 45 year old lady who was previously fit and well is admitted with breathlessness, palpitations and a history of two episodes of syncope over the past two days. Upon further questioning, she admits to having difficulty breathing when she sits upright. She finds great relief when she lies down flat on her couch. Upon examination, the tips of her fingers are noted to be blue and clubbing is noticed. Auscultation reveals a mid-diastolic rumble which changes when the patient changes position and a loud S1 at the cardiac apex. What is the most likely diagnosis?
Correct Answer : C
ATRIAL MYXOMA are benign tumours. Around three-quarters of atrial myxomas occur in the left atria and tend to grow on the wall (septum).
Sometimes small pieces of the tumour can break off and fall into the bloodstream. If this happens, they can block an artery elsewhere in the body such as the brain, which could cause a stroke, or in the lungs causing a pulmonary embolus. Around 10% of myxomas seem to be inherited (passed down through families). These are known as familial myxomas.
The symptoms occur due to obstruction of the mitral valve which results in syncope and heart failure.
Features :
• Symptoms of haemodynamic obstruction, embolization, or constitutional symptoms such as fever, malaise, tachycardia, and tachypnoea
• Symptoms and signs of ischaemia or infarction in the peripheries, due to embolization of adherent thrombus
• Atrial fibrillation
• Large myxomas may impair intracardiac blood flow, causing dyspnoea, syncope, or symptoms and signs of congestive cardiac failure.
• Echo: Pedunculated heterogeneous mass typically attached to the fossa ovalis region of the interatrial septum.
Q.8. A 75 year old man is found to be unresponsive. The ward doctor is called to the patient’s bedside. He is not breathing and has no detectable pulse. Which is the most appropriate next step?
Correct Answer : C
Start chest compressions.
Q.9. A 58 year old man with a history of type 1 diabetes mellitus and hypertension for 13 years develops sudden central chest pain and abdominal pain for 45 minutes. The pain radiates to his jaw. It started while he was driving and it was associated with cold sweating and dyspnoea. He describes the pain as a burning pain. What is the most likely diagnosis?
Correct Answer : B
This is clear that this is a myocardial infarction. Atypical presentations of myocardial infarction are common. They may present with abdominal pain in the question above. Atypical symptoms include abdominal discomfort or jaw pain. The remaining symptoms are quite characteristic of myocardial infarction.
• In pericarditis, the pain is aggravated by inspiration or lying flat and relieved by leaning forward. A pericardial rub may present and there may be a fever
• In pulmonary embolism, patients would present with dyspnoea and pleuritic chest pain.
The writers of the exam would also give other hints like having a history of immobilization or a long travel.
• In costochondritis, the pain is localized at the costochondral junction which is enhanced by motion, coughing, or sneezing. The writers would usually give a history of repeated minor chest injury or activities that one is unused to – perhaps decorating or moving furniture.
• In pneumothorax, the pain is not central but pleuritic and there are no signs that indicate that this is a pneumothorax in the given question The given picture of central chest pain for 45 minutes (more than 30 minutes), sweating, and dyspnoea with major risk factors of diabetes mellitus and hypertension suggest the diagnosis of myocardial infarction.
ACUTE MYOCARDIAL INFARCTION PRESENTATION :
Chest pain (central chest pain may not be the main symptom)
• Three-quarters of patients present with characteristic central or epigastric chest pain radiating to the arms, shoulders, neck, or jaw
• The pain is described as substernal pressure, squeezing, aching, burning, or even sharp pain
• Radiation to the left arm or neck is common
• Chest pain may be associated with sweating, nausea, vomiting, dyspnoea, fatigue and/or palpitations
• Shortness of breath
Atypical presentations are common and tend to be seen in women, older men, and people with diabetes. Atypical symptoms include abdominal discomfort or jaw pain. Elderly patients may even present with altered mental state.
ACUTE CHEST PAIN DIFFERENTIALS:
Ischaemic cardiac pain - Retrosternal “pressure”, tightness”, “constricting”, Radiates to shoulders, arms, neck, or jaw. Associated with diaphoresis, sweating, nausea, pallor.
Pericarditis - Atypical, retrosternal pain, Sometimes pleuritic, Positional (relieved on sitting forward).
Gastroesophageal reflux disease - Retrosternal “burning”, Associated with indigestion, Pain when supine, after consumption of food, alcohol, and NSAIDs, Relieved by antacids.
Aortic dissection - “Tearing” pain, sudden in onset. Radiates to back, Diaphoresis, hypotensive, tachycardic. Differences in blood pressures and/or pulses, Abnormal or absent peripheral pulses, New murmur (aortic regurgitation)
Pulmonary embolism - Acute respiratory distress, Diaphoresis, hypotensive, tachycardic, hypoxaemia, Pleural rub.
Pneumothorax - Pleuritic, sharp, positional, sudden in onset Associated with abrupt breathlessness, Diminished breath sounds, hyperresonance to percussion.
Pneumonia - Associated with cough, sputum, and fever.
Musculoskeletal - Sharp, positional, pleuritic aggravated by movement such as deep inspiration, coughing, twisting of neck or thoracic cage.
Q.10. A 65 year old man has chest pain. On initial assessment, he is noted to be pale. An ECG reveals no connection between P waves and QRS complexes with a rate of 42 beats/minute. What is the most likely diagnosis?
Correct Answer : C
First-degree heart block :
• PR interval > 0.2 seconds
Second-degree heart block: Mobitz type I AV block (Wenckeback block/phenomenon)
• Progressive prolongation of the PR interval until a dropped beat occurs Mobitz type II AV block
• PR interval is constant but the P wave is often not followed by a QRS complex (dropped beat)
Third degree (complete):
• P waves will occur regularly, usually at heart block: a rate of around 75 beats per minute but are completely unconnected to the rhythm of the QRS complexes.
Q.11. A 46 year old man was broguht into the A&E after being stabbed in the chest with a knife. His chest is bilaterally clear. He has muffled heart sounds and his neck veings look distended. His blood pressure is 84/40 mmHg and pulse is 110 bpm. What is the most appropriate investigation that can lead to a a diagnosis?
Correct Answer : D
This question points towards cardiac tamponade. His chest is bilaterally clear thus we can therefore exclude pneumothorax or pleural effusion. Muffled heart sounds, distended neck veins and hypotension are called Beck’s triad and it is a classical finding in cardiac tamponade. This is diagnosed with an echocardiogram.
These are the most common features that are asked in exams .
ACUTE PERICARDITIS:
Causes include -
• Viral infections (Coxsackie)
• Tuberculosis
• Uraemia
• Trauma
• Post-myocardial infarction, Dressler’s syndrome
• Connective tissue disease
Clinical Features - Central chest pain is worse on inspiration or lying flat and relieved by sitting forward (Pericardial friction rub)
ECG classically shows concave (saddle-shaped) ST-segment elevation, Troponin may be raised.
Treatment NSAIDS.
PERICARDIAL EFFUSION:
Clinical features - Dyspnoea, Raised JVP
CXR shows an enlarged, globular heart ECG shows low-voltage QRS complexes and alternating.
Treatment - Pericardiocentesis
CARDIAC TAMPONADE :
A life-threatening condition in which a pericardial effusion has developed so rapidly or has become so large that it compresses the heart.
Etiology : Usually penetrating or blunt chest trauma
Features :
• Dyspnoea
• Raised JVP – seen by having neck veins which are distended
• Tachycardia
• Hypotension
• Muffled heart sounds
• Pulsus paradoxus
Remember Beck’s triad: Muffled heart sounds, distended neck veins, and hypotension
Diagnosis - Echocardiography
Treatment - Pericardiocentesis.
Q.12. A 20 year old man comes to the Emergency Department complaining of palpitations that began when he woke up earlier today. The palpitations have been continuous and are still on going. He denies chest pain, shortness of breath or dizziness. His blood pressure is 120/80 beats per minute. He has a respiratory rate of 23 breaths/minute. He is completely conscious throughout. Below is his ECG taken in the Emergency Department.
Correct Answer : B
This ECG shows supraventricular tachycardia. Carotid massage should be attempted before giving IV adenosine.
SUPRAVENTRICULAR TACHYCARDIA : Paroxysmal supraventricular tachycardia is manifested as a regular rhythm at a rate between 130 and 220 beats/min. Acute management if hemodynamically stable, this should be done in the following sequence :
• 1st : Valsalva manoeuvre, carotid massage
• 2nd : Adenosine 6 mg rapid IV bolus (or verapamil – but verapamil is rarely used for SVT now unless the patient is asthmatic in which case verapamil is used instead of adenosine)
If adenosine is unsuccessful in converting to normal sinus rhythm then give another 12 mg IV adenosine.
If still unsuccessful give a further 12 mg IV adenosine.
• 3rd : Electrical Cardioversion
Acute management if hemodynamically unstable -
• Direct current (DC) cardioversion
Prevention of episodes:
• Beta-blockers
• Radio-frequency ablation.
Q.13. A 53 year old man with chronic heart failure, develops a red, swollen and acutely tender right large toe. He is subsequently diagnosed with gout and started on a new medication. A few days later his symptoms of gout have significantly improved however, he is now short of breath and complaining of orthopnea. What is the likely medication that he was started on?
Correct Answer : C
Non-steroidal anti-inflammatory drugs (NSAIDs) should be avoided in patients with chronic kidney disease, heart failure, or ischaemic heart disease. Selective COX-2 inhibitors should also be avoided in these patients. NSAIDs inhibit the synthesis of prostaglandins.
This in turn can lead to a reduction in sodium excretion, renal perfusion, and glomerular filtration rate. They can also reduce the effectiveness and increase the toxicity of ACE inhibitors and diuretics. This can result in an exacerbation of heart failure.
NSAIDs can cause the kidneys to retain more salt and water in the body which can increase your risk of heart failure.
They can also make some blood pressure-lowering medicines, such as ACE inhibitors and diuretics, less effective – and a rise in blood pressure is likely to worsen heart failure. It is also worth noting that thiazide diuretics increase the risk of gout due to reduced clearance of uric acid.
Q.14. A 50 year old smoker and heavy drinker presents with complaints of a racing heart. He has no chest pain. The palpitations usually occur when he drinks alcohol or after a meal. He has no significant past medical history. A 24 hours ECG is shown to be normal. What is the most appropriate action?
Correct Answer : A
A racing heart or palpitation is a common phenomenon in alcoholics which is not serious or harmful. So reassure the patient.
Q.15. A 50 year old man attends the Emergency Department with complaints of shortness of breath and palpitations which started 4 hours ago. He denies chest pain. He has a pulse of 142 beats/minute, a blood pressure of 110/80 mmHg and a respiratory rate of 20 breaths/minute. His past medical history includes hypertension, type 2 diabetes mellitus and angina. An ECG was performed which shows supraventricular tachycardia. Carotid sinus massage was attempted but he is still tachycardic. What is the most appropriate next management?
Correct Answer : C
The next step for management after trying carotid sinus massage would be intravenous adenosine. Verapamil is rarely used for SVT now unless the patient is asthmatic in which case verapamil is used instead of adenosine. The history of hypertension, type 2 diabetes mellitus, and angina have little or no significance in this question.
Q.16. A 74 year old man started having chest pain. He has a blood pressure of 70/50 mmHg. His level of consciousness is decreased. A radial pulse is felt. An ECG shows the following rhythm. What is the most appropriate management?
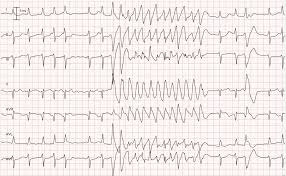
Correct Answer : A
For junior doctors, the ECG pattern between ventricular tachycardia and ventricular fibrillation can be hard to distinguish. But here as the patient is still conscious, it cannot be ventricular fibrillation as V. fib would present without a pulse and the patient would not be conscious. Thus, ventricular tachycardia is the answer here. Since the patient is haemodynamically unstable, cardioversion would be the answer.
VENTRICULAR TACHYCARDIA :
Ventricular tachycardia may impair cardiac output with consequent hypotension, collapse, and acute cardiac failure. This is due to extreme heart rates and lack of coordinated atrial contraction (loss of “atrial kick”).The rate of V. Tach is from about 100-250 bpm. P Waves may be present or absent. P waves are usually not seen if the rate is increased. If present, the P waves have no relation to the QRS complexes.
V. Tach can present in two ways:
1. With Pulse : Haemodynamically stable or Haemodynamically unstable e.g. hypotension, chest pain, cardiac failure, decreased consciousness level.
2. Without Pulse : Management depends on how the patient presents.
With Pulse & Haemodynamically stable : Antiarrhythmics e.g. amiodarone, lidocaine, procainamide ; Haemodynamically unstable e.g. hypotension, chest pain, cardiac failure, decreased consciousness level - Immediate electrical cardioversion is indicated.
Without Pulse - Immediate electrical cardioversion is indicated.
ECG ARRHYTHMIA CLINCHERS :
These clinchers help point you towards an answer but you still need to read the whole stem and look at the ECG before you decide. The exam can be tricky.
Atrial Fibrillation:
• Palpitations
• Fast heart rate
• Dyspnoea
Atrial Flutter :
• The patient in the stem will describe it as a “fluttering feeling in the chest”
Ventricular Fibrillation :
• Older adult with sudden collapse
• Not breathing
Ventricular Tachycardia :
• Regular and fast
• Stem will mention a period of ongoing lightheadedness, palpitations, and chest pain (rarely will they present with collapsed in exams)
Sinus Bradycardia : Lightheadedness, dizziness, hypotension, vertigo and syncope
Note - Slow heart rate is completely normal in young athletes.
Sinus Tachycardia :
• Physiological situations, such as exercise or situations of stress or anger
• History of infection
Heart Block :
• Stem will mention an older patient who has suffered a previous MI or who has ACS.
Type 1 AV Block: Lengthening of the PR interval
Type 2 AV Block Mobitz I: Progressive prolongation of PR interval until a P wave is dropped
Mobitz II: Randomly dropped P waves
Type 3 AV Block (Complete Heart Block): No P waves
Wolff-Parkinson White Syndrome : “Delta wave” on ECG.
Q.17. A 25 year old male presents to Accident & Emergency with the complaint of substernal sharp chest pain. The patient claims that the pain is much worse on inspiration. His pas medical history is insignificant however, he smokes 20 cigarettes daily and drinks 50 units of alcohol weekly. On examination, his chest is clinically clear and his abdominal examination was found to be normal. His vitals are noted as: Temperature 38 C Respiratory rate 18 breaths/minute Blood pressure 110/70 mmHg Oxygen saturation 97% What is the most likely diagnosis for this patient?
Correct Answer : B
This is simply a diagnosis of exclusion.
In pericarditis, the chest pain felt by patients is pleuritic and aggravated by inspiration, coughing, and a change to the upright position. The pain is relieved when the patient lies down – an important feature that was deliberately left out of the stem. The diagnosis of pericarditis involves the typical chest pain, pericardial friction rub on auscultation, and characteristic ECG changes this question stem only gives one part of a clue for diagnosis which is the pleuritic chest pain and a fever.
Remember, not all questions in exams are straightforward.
ACUTE PERICARDITIS :
• Chest pain is described as sharp, stabbing, central chest pain, with radiation to the shoulders and upper arm
• Chest pain may be pleuritic and is often relieved by sitting forwards
• Chest pain may be made by inspiration, cough, swallowing, or movement of the trunk
• Other symptoms include non-productive cough and dyspnoea
• Pericardial friction rub on auscultation
Clinically, the presence of a pericardial friction rub is pathognomic – often a rub can be heard even when a pericardial effusion is present.
Causes :
• Viral infections (Coxsackie)
• Tuberculosis
• Uraemia (causes ‘fibrinous’ pericarditis)
• Trauma
• Post-myocardial infarction, Dressler’s syndrome
• Connective tissue disease
Post-myocardial infarction is an extremely important cause to remember for the exam.
ECG changes : Widespread ‘saddle-shaped’ ST elevation (Saddle-shaped meaning concavity directed upwards) and PR segment depression.
Q.18. An 82 year old male was walking in his garden when he suddenly fell to the ground and was unconscious. He recovered completely within a few minutes however, he described feeling very hot and flushed after the episode. He remembers the events prior to the fall and confidently says he did not trip. He denies feeling sweaty or dizzy prior to the fall. What is the best investigation to diagnose his problem?
Correct Answer : D
Patients who have an unannounced loss of postural tone leading to a period of unconsciousness need to be investigated for three main causes which are:
• Irregular rhythms
• Low blood pressure or postural drop
• Seizures
The first two (irregular rhythms and low blood pressure or postural drop) are easy to investigate however seizures are a little bit more difficult and thus we would only suspect it if there was an eyewitness who saw the fit.
There is usually a period of post-ictal drowsiness or confusion if a seizure is to be considered. This stem mentions that he recovered completely within a few minutes which tells us that a seizure is unlikely. Cardiac syncopal events are the most likely here as they are usually abrupt in onset with rapid recovery with flushing. This is the reason that ECG is the answer here.
In many cases, it may be due to a vasovagal syncope which is a common response to an overwarm environment or a period of prolonged standing. It can also occur after a visual stimulus such as seeing blood on the floor. However, patients with vasovagal syncopes would normally feel dizzy and have ‘tunnel vision’ before the syncopal episode. This is not evident in this stem.
INVESTIGATIONS FOLLOWING SYNCOPE :
Things to do for patients who had a syncopal event and recovered
• Find witnesses – see if family members or friends have seen how the patient became unconscious or was there a seizure witnessed.
• Perform an ECG to look for arrhythmias
• Perform blood pressure supine and standing or sitting to look for a postural drop
• Check blood glucose to exclude hypoglycemia.
Q.19. A 42 year old man collapsed and died at home. The GP’s report states that he has type 2 diabetes and has a BMI of 35. What is the most likely cause of death?
Correct Answer : C
Although there are risk factors for myocardial infarction and pulmonary embolism, it is more likely a myocardial infarction that killed this man because in diabetics, myocardial infarction can be painless as the patient can develop autonomic neuropathy. We call this a “silent MI”. If one does not feel pain, he might not call for help. As this progresses, he collapses and dies.
Q.20. A 68 year old man is found collapsed at a shopping mall. An ECG reveals no connection between P waves and QRS complexes with a rate of 35 beats/minute. What is the most likely diagnosis?
Correct Answer : A
Please see Q-10 for heart block
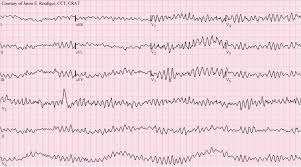
Q.21. A 72 year old man is found not breathing in the CCU with the following rhythm. His pulse cannot be felt. What is the most likely diagnosis?
Correct Answer : B
VENTRICULAR FIBRILLATION :
Ventricular Fibrillation means “sudden death”. The blood pressure drops immediately to zero and so does the cardiac output. Ventricular fibrillation (VF) is the most important shockable cardiac arrest rhythm. The ventricles suddenly attempt to contract at rates of up to 500 bpm. This rapid and irregular electricalactivity renders the ventricles unable to contract in a synchronized manner, resulting in immediate loss of cardiac output.
Unless advanced life support is rapidly instituted, this rhythm is invariably fatal. Prolonged ventricular fibrillation results in decreasing waveform amplitude, from initial coarse VF to fine VF and ultimately moving on to asystole due to progressive depletion of myocardial energy stores.
ECG Findings for V. Fib:
• Chaotic irregular deflections of varying amplitude
• No identifiable P waves, QRS complexes or T waves
• Rate 150 to 500 per minute
• There is no specific pattern to the discharge. There are different types of wavering baseline patterns.
Q.22. A 58 year old man with a past history of myocardial infarction and type 2 diabetes mellitus has a new diagnosis of hypertension. He is currently taking aspirin, atorvastatin and metformin. What is the most approprite medication to be added?
Correct Answer : A
This question is testing your management of hypertension with diabetes. Patients with type 2 diabetes mellitus have a considerably higher risk of cardiovascular morbidity and mortality, not to mention hypertension plays a major role in the development and progression of microvascular and macrovascular disease in people with diabetes.
Treatment in this group of patients is especially important. The management for a person with hypertension alone differs slightly when compared to the management of a patient with hypertension and diabetes. First-line antihypertensive drug treatment in a hypertensive patient with diabetes should be an ACE inhibitor unless the patient is Afro-Caribbean. Age here is irrelevant when the patient has diabetes.
Given the benefits of ACE inhibitors in terms of reno-protection and retinopathy, it is appropriate to recommend an ACE inhibitor as the first line for the treatment of hypertension in most adults with type 2 diabetes. This is partly due to the positive effect on glucose metabolism. For people of African or Caribbean family origin, an ACE inhibitor plus either a diuretic or a calcium channel blocker is the first line.
HYPERTENSION MANAGEMENT IN NONDIABETICS AND DIABETICS:
HYPERTENSION ALONE : First line :
• Age < 55 - ACE inhibitor
• Age > 55 or of black African or Caribbean origin - calcium channel blocker
HYPERTENSION & TYPE 2 DM: First line :
• Any age - ACE inhibitor
• Black African or Caribbean origin - ACE inhibitor plus either a diuretic or a calcium channel blocker.
Q.23. A 65 year old woman comes in to the Emergency Department complains of leg cramps and feeling weak. She takes bendroflumethiazide for hypertension. Her blood test show the following: Sodium 134 mmol/l Potassium 2.1 mmol/l Urea 4.1 mmol/l Creatinine 66 micromol/l Glucose 4.8 mmol/l What is the most likely ECG feature to be seen?
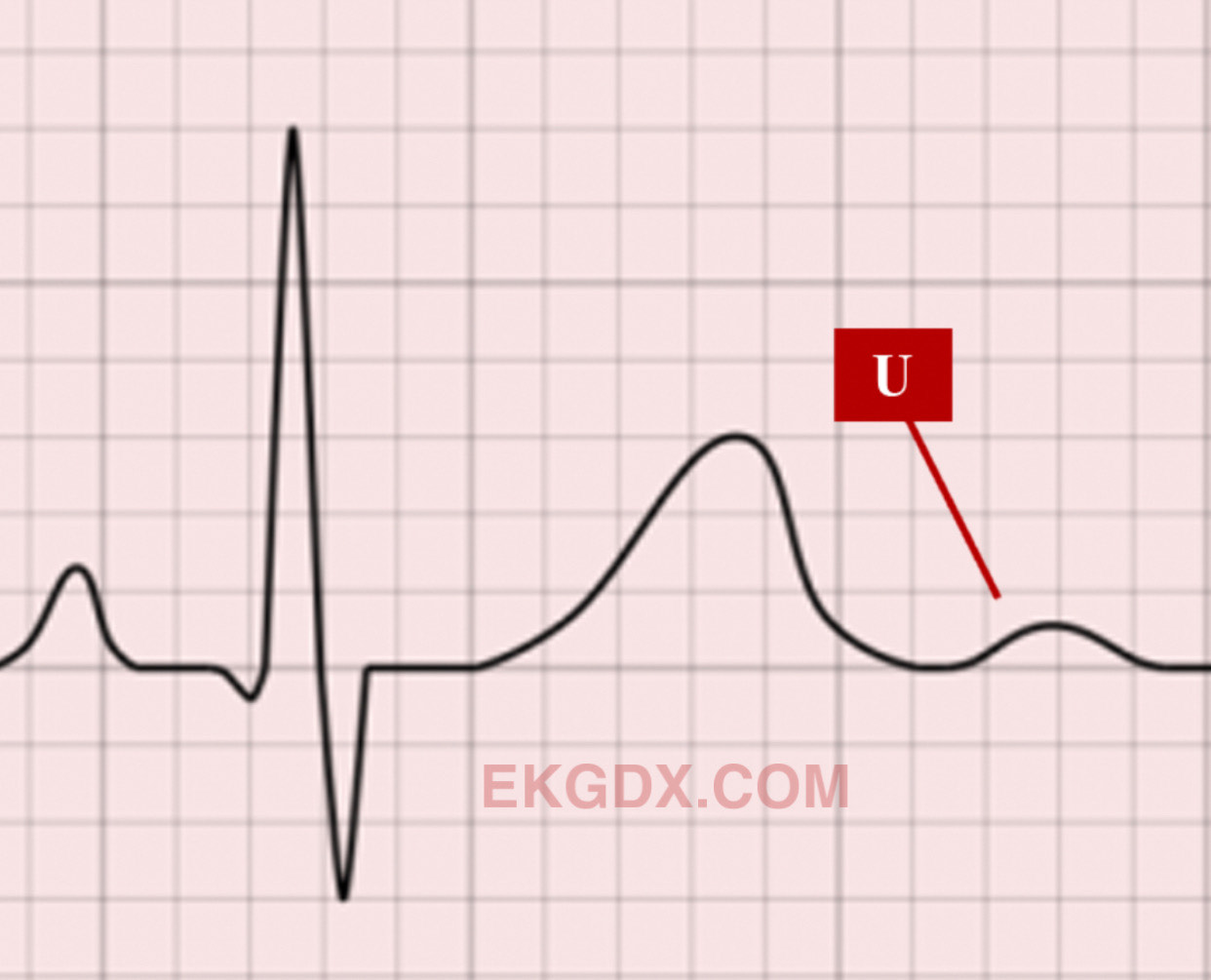
Correct Answer : B
Muscle weakness and cramping are features of low potassium. The potassium levels shown here are severely low. Low enough that management is likely going to be IV replacement in an area where there is cardiac monitoring. Thiazides such as bendroflumethiazide can increase potassium loss which results in hypokalemia. U waves are seen in hypokaleimia.
The other answers are less likely: J waves are usually observed in patients suffering from hypothermia.
Delta waves are seen in Wolff Parkinson's White syndrome. PR interval in hypokalemia is prolonged. QT interval remains the same in hypokalemia although Q-T interval may be falsely seen as prolonged in hypokalaemia. It is usually the U wave that is mistaken for the T wave. These are situations that may falsely suggest a prolonged Q-T interval. This is an example of a prominent U wave.
A low T wave followed by a prominent U wave produces a ‘camel-hump’ effect. As hypokalaemia progresses to be more severe, the T wave decreases in amplitude and is flattened or becomes inverted. The U wave becomes more prominent. This may falsely be seen as a prolongation of the Q-T interval.
ECG features of hypokalaemia :
• Prominent U-waves
• Small or absent T waves
• Prolonged PR interval
• ST depression
Mnemonic: HypUkalaemia – U waves.
Q.24. A 51 year old female presents with the complaint of increasing breathlessness and breathlessness on exertion. She has been having difficulty in sleeping lately and she says that she has to use three pillows to sleep at night. On examination, the patient is noted to have bilateral pedal oedema up to the level of her calf and widespread crepitations bilaterally on auscultation. Auscultation of the heart reveals a pansystolic murmur at the cardiac apex. An ECG was done which was significant for a broad P wave. She has no medical problems other than asthma, which was diagnosed when she was 7 years old, and that she had rheumatic fever when she was 14 years old. She does not drink alcohol or smoke. What is the most likely cardiac defect that this patient has?
Correct Answer : A
The patient has mitral regurgitation secondary to rheumatic fever. Some exam clinchers for mitral regurgitation:
• Previous disease that affects the mitral valve
• Signs and symptoms of pulmonary oedema will appear in the stem
• Panysystolic murmur at the cardiac apex is the murmur of mitral regurgitation
• Chest X-ray if given may show an enlarged left side of the heart.
MITRAL REGURGITATION :
Common scenarios in the exam are history of rheumatic fever.
• A few weeks after a myocardial infarction where the patient may be admitted for pulmonary oedema.
Clinical features of Left ventricular failure :
• Dyspnoea
• Orthopnoea
• Paroxysmal nocturnal dyspnoea
With severe and chronic mitral regurgitation, right-sided failure would eventually occur leading to:
• Oedema
• Ascites
Important clinical sign : Pansystolic apical murmur radiating to the axilla
ECG - signs of left ventricular hypertrophy and left atrial enlargement (e.g. broad P wave)
Chest X-ray - may show an enlarged left side of the heart
Diagnosis :
- Echocardiography.
Q.25. A 38 year old man presents to the emergency department feeling unwell and dizzy. He has a heart rate of around 35 beats/minute. What is the most appropriate first line treatment?
Correct Answer : C
Atropine is the first drug of choice for symptomatic bradycardia.
The dose in the bradycardia ACLS algorithm is 0.5 mg intravenous push and may repeat up to a total dose of 3 mg.
Q.26. A 42 year old lady had corrective surgery for cyanotic congenital heart disease at the age of 3 after having a palliative operation during infancy. On examination, a parasternal heave and a diastolic murmur at the left upper sternal edge is noted. What is the most likely diagnosis?
Correct Answer : D
Pulmonary regurgitation is a common complication after surgical or percutaneous relief of pulmonary stenosis and following repair of Fallot's tetralogy. Pulmonary regurgitation is usually asymptomatic unless severe, when it may lead to signs of right heart failure. Patients can live for many decades following surgical repair of tetralogy of Fallot but a major problem encountered is the development of pulmonary regurgitation which may require pulmonary valve replacement.
Q.27. A 40 year old man was brought into the A&E after being hit by a vehicle. He sustained trauma to the chest. His neck veins look distended and his heart sounds are faint. He has a blood pressure of 80/45 mmHg and pulse is 120 bpm. His trachea is central. What is the most appropriate management?
Correct Answer : C
This question points towards cardiac tamponade. Trachea is central thus tension pneumothorax is less likely. Muffled heart sounds, distended neck veins and hypotension are called Beck’s triad and are a clinical finding in cardiac tamponade. Please see Q-11
Q.28. A 22 year old male athlete has been having frequent fainting attacks since childhood. He has no family history of sudden death or arrhythmias. His ECG demonstrates a sinus rhythm with normal P-R and QRS intervals but a prolonged QT interval. What is the cause of his fainting?
Correct Answer : B
A polymorphic ventricular tachycardia is when there are beat-to-beat variations with no uniform pattern of ventricular contraction. This is also known as Torsades de points. Remember the ECG being described is one at rest, not during the fainting episode (when QRS would be broad due to the ventricular tachycardia) Prolonged QT syndrome is when the QT interval is abnormally long, predisposing individuals to ventricular arrhythmias (particularly Torsades de pointes), syncope, and sudden death.
There are no pre-syncope symptoms before fainting, which can be exacerbated by exercise, stress, medications, and electrolyte abnormalities. Sick sinus syndrome is a group of conditions affecting the function of the sinoatrial node.
It is usually associated with periods of sinus bradycardia, tachy-brady syndrome, atrial fibrillation, or flutter. It is not associated with a prolonged QT interval. The ECG demonstrates a sinus rhythm, which is not seen in a complete heart block (P waves not associated with QRS).
Aystole is not associated with a prolonged QT interval. Atrial fibrillation does not lead to fainting. Remember the atria only contributes to 15% of the overall blood ejected from the ventricle.
Q.29. A 33 year old main complains of occasional left sided chest pain that lasts less than 30 minutes following exercise. The pain is relieved once he takes a rest. What is the most likely diagnosis?
Correct Answer : A
Angina is chest pain or discomfort that is caused when the heart muscle does not get enough blood. In stable angina, the pain is precipitated by predictable factors like exercise. This is relieved by rest.
Q.30. A 72 year old woman is brought in by her husband as she has sudden chest discomfort, palpitations and epigastric pain which started 1 hour ago. She has been feeling nauseous. She denies pain radiating to the arms or neck. There are ST elevations seen on leads II, III and aVF on the ECG. Oxygen has been started. She has been given sublingual GTN and diamorphine which has improved her chest pain. Her heart rate is 90 beats/minute and respiratory rate is 18 breaths/minute. What is the most appropriate next step in management?
Correct Answer : B
Not all myocardial infarctions present with the typical cardiac chest pain symptoms. Some may present with atypical chest pain which can be described as an ache or discomfort. Other atypical symptoms include abdominal discomfort or epigastric pain. As there is ST elevation in leads I, II, and aVF, this confirms the diagnosis of a myocardial infarction. Percutaneous intervention (PCI) would be the best management for myocardial infarction.
POST-MANAGEMENT OF HEART FAILURE AND MYOCARDIAL INFARCTION (MI):
HEART FAILURE: Drugs that decreases mortality -
1. ACE inhibitor (Enalapril, Lisinopril, Ramipril)
2. Beta-blocker (Bisoprolol, Carvedilol, Nebivolol) (Initiate one at a time)
Manage symptoms - Furosemide add on if symptoms are not controlled; Spironolactone, or Digoxin.
ALL pts with MI on discharge:
Dual antiplatelet therapy: Aspirin + Clopidogrel
Note: Aspirin is continued lifelong Clopidogrel for 12 months.
• Beta Blockers : Offer BB to people who present acutely with MI as soon as they are haemodynamically stable. Continue a beta blocker for at least 12 months after an MI in people without heart failure. Continue a beta-blocker indefinitely in people with HF.
• ACEI : Offer ACEI to people who present acutely with MI as soon as they are haemodynamically stable. If intolerant to ACEi – use ARB.
• STATINS.
MYOCARDIAL INFARCTION MANAGEMENT: Myocardial infarction management is tricky and it is always changing. A good way to remember the first few steps of managing myocardial infarction is to remember the mnemonic.
MONA = Morphine, O2, Nitrates, Aspirin 300 mg. Morphine is given intravenously to manage the pain.
Oxygen is administered if there is evidence of hypoxia, pulmonary oedema, or continuing myocardial ischaemia. Nitrates such as GTN sublingual or by intravenous infusion are used to treat angina. Aspirin 300 mg should be given preferably before arrival at the hospital. Clopidogrel 300 mg should also be given. Heparin (unfractionated) or low molecular weight heparin (e.g. enoxaparin sodium) should also be considered.
STEMI management summary .
• If a patient presents to the hospital with symptom onset within 12 hours AND PCI can be delivered within 120 minutes of the time when fibrinolysis could have been given - perform PCI.
• If PCI is not available and cannot be delivered within 120 minutes when fibrinolysis could have been given – Thrombolysis (Alteplase)
• Thrombolysis can only be done within 12 hours of symptom onset.
Q.31. A 6 week old baby presents with the following features of progressive cyanosis, poor feeding, tachypnoea during the first two weeks of life. A holosystolic mumur is heard. What is the most likely diagnosis?
Correct Answer : C
The most common cyanotic heart conditions presenting in the neonatal period are referred to as “The five T’s”
1. Tetrology of Fallot (TOF)
2. Transposition of the Great Arteries (TGA)
3. Truncus Arteriosus
4. Tricuspid Atresia
5. Total Anomalous Pulmonary Venous Connection (TAPVC)
By using the above mnemonic, we are down to 2 options : Tricuspid atresia or Tetralogy of Fallot
Tricuspid Atresia : Manifests early in life with severe cyanosis. Holosystolic murmurs are found along the left sternal border (Most have VSD)
Tetralogy of Fallot : This can also happen at birth but the symptoms depend on the severity. Ejection systolic murmur due to pulmonary stenosis is the common murmur to be heard.
Q.32. A 52 year old man with history of anterior myocardial infarction 3 weeks ago developed a sudden onset of dyspnoea. He has a blood pressure of 100/60 mmHg, pulse rate of 100 beats/minute, SaO2 = 88%, and his chest is audible for bilateral crackles. What is the best investigation to determine the underlying cause?
Correct Answer : C
The key word here to look out for is “investigation to determine the underlying cause”. A chest X-ray might show features of pulmonary oedema but will not show the underlying cause.
An echocardiogram is more likely to identify the underlying cause whether it be a post myocardial infarction complication such as ventricular aneurysm, infarct expansion, acute mitral regurgitation from papillary muscle rupture or ventricular septal rupture.
Q.33. A 72 year old man is found to be unresponsive. The ward doctor is called to the patient’s bedside by one of the patient’s relative. He is not breathing and has no detectable pulse. Which is the most appropriate next step?
Correct Answer : C
This man has had a cardiac arrest. The resuscitation guidelines state that if there are no signs of life, call the resuscitation team. Basic life support is an important topic for exam. Be sure to know the sequence of management.
The other choices in this question are less appropriate.
Get a defibrillator – The guidelines mention starting CPR and sending for a defibrillator as soon as possible. But given the choice, calling the resuscitation team would come first.
Q.34. A 69 year old women had sudden burning chest pain and shortness of breath that started 4 hours ago. The pain was associated with nausea, vomiting and diaphoresis. Her ECG on admission shows ST elevation in leads II, III and aVF. Oxygen has been started and she was given sublingual GTN which has improved her chest pain. She was given aspirin 300 mg by the ambulance crew. Her heart rate is 70 bpm and respiratory rate is 18/min. What is the most approprite next step in management?
Correct Answer : B
Nausea, vomiting, and diaphoresis (sweating) are symptoms that usually accompany cardiac chest pain. Percutaneous intervention (PCI) would be the best management for myocardial infarction. As PCI is not given in the option, thrombolysis would be the next best step. In terms of thrombolysis, Alteplase is preferred over streptokinase. However, alteplase is not given in the options thus the best option would be option B (streptokinase).
Q.35. A 55 year old man had a myocardial infarction 3 days ago. He now complains of a shortness of breath and a sharp pain in the chest. The pain increases when he breathes and is relieved when sitting forward. His respiratory rate is 22 breaths/minute and his heart rate is 95 beats/minute. What is the most likely diagnosis?
Correct Answer : D
Pericarditis is one of the differentials of any patient presenting with chest pain. Pericarditis presents as sharp, pleuritic, and positional chest pain, usually 1 to 3 days post-infarct. The pain that is relieved when sitting forward is a clincher for pericarditis.
Q.36. A 2 week old baby has oxygen saturation of 70% on air. He is cyanosed and has an ejection systolic murmur. What is the most likely diagnosis?
Correct Answer : A
Tetralogy of Fallot is the most likely diagnosis here. It usually presents with an ejection systolic murmur. The low oxygen saturation and cyanosis are consistent with the Tetralogy of Fallot.
TETRALOGY OF FALLOT -
• The most common cause of cyanotic congenital heart disease
• Typically presents at around 1-2 months, although may not be placed until the baby is 6 months old The four characteristic features are:
• Ventricular septal defect (VSD)
• Right ventricular hypertrophy
• Pulmonary stenosis
• Overriding aorta Other features
• Cyanosis
• Causes a right-to-left shunt
• Ejection systolic murmur due to pulmonary stenosis (the VSD does not usually cause a murmur)
• A right-sided aortic arch is seen in 25% of patients
• Chest x-ray shows a ‘boot-shaped’ heart, ECG shows right ventricular hypertrophy.
Q.37. A 56 year old man presents to the emergency department with chest pain. The following ECG was taken. What is the most likely diagnosis?
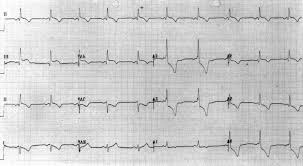
Correct Answer : C
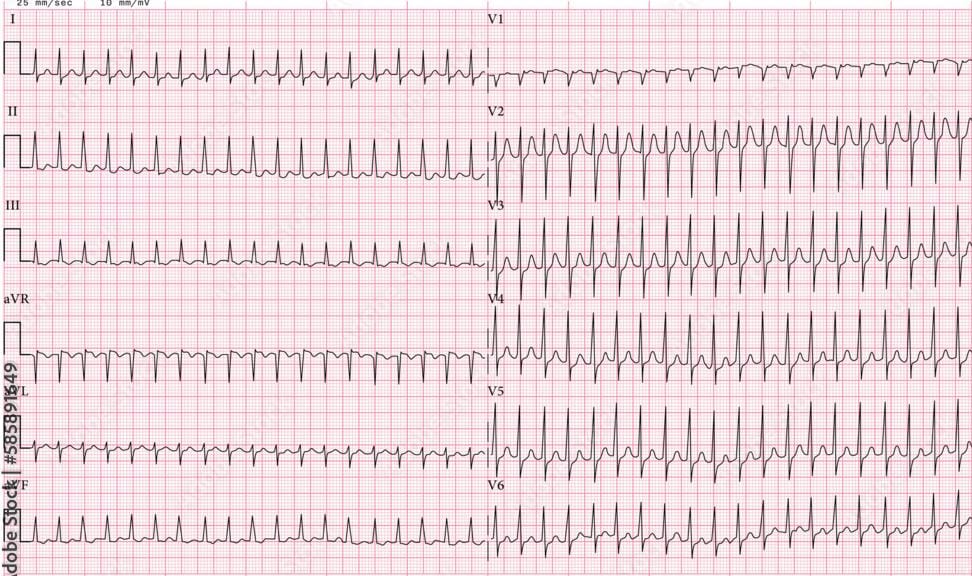
We can note that there is ST elevation in lead V2, V3, V4. This ECG shows a classical example of an anterior myocardial infarction.Those ECG findings are more than enough to answer the questions in the exam and it is highly unlikely that you would need to know more than that. For those who want to go into more details (probably noted needed for the exam), one can notice the following on this ECG :
• Q waves are present in the septal leads (V1-2)
• Note the subtle ST elevation in I, aVL, and V5, with reciprocal ST depression in lead III.
• There are hyperacute (peaked) T waves in V2, V3 and V4. These features indicate an anteroseptal STEMI.
ECG CHANGES IN MYOCARDIAL INFARCTION AND CORONARY ARTERIES :
MOST COMMONLY ASKED :
Anteroseptal : V1-V4 - Left anterior descending (LAD)
Inferior : II, III, aVF - Right coronary (RCA)
Lateral : I, aVL, V5-6 - Left circumflex
Q.38. A 47 year old man with history of a myocardial infarction complains of chest pain with shortness of breath on exertion over the past few days. ECG was shown to be normal. Echocardiogram shows decreased ejection fraction and decreased septal wall thickness. What is the most likely diagnosis?
Correct Answer : A
Although in many cases no cause is apparent, dilated cardiomyopathy is probably the result of damage to the myocardium. In this case, it was due to the fibrous change of the myocardium from a previous myocardial infarction. This is supported by the decreased ejection fraction and thinning of the septal walls seen on an echocardiogram.
DILATED CARDIOMYOPATHY :
• A disorder of heart muscle characterized by left ventricular and/or right ventricular dilation and impairment of systolic function.
• Presents as congestive heart failure, Dyspnoea, Oedema, Raised JVP, Pulmonary congestion, Cardiomegaly.
Q.39. A 55 year old man presents to the Emergency Department with palpitations, chest pain and dizziness. An ECG was performed is shown below. What is the most likely diagnosis?
Correct Answer : C
In Atrial flutter, you will see the characteristic “flutter waves” which are a “saw tooth” shape. The flutter waves replace the P waves. In general, this is managed in the same way as an atrial fibrillation.
ATRIAL FLUTTER VS ATRIAL FIBRILLATION :
ATRIAL FLUTTER: Atrial activity - Rate: 220-350 bpm, Visible flutter (F) waves
Ventricular activity - Rate: Regular, Constant R-R interval. Baseline - Sawtooth
ATRIAL FIBRILLATION: Atrial activity - Rate: > 350 bpm, Fine fibrillatory (f) waves
Ventricular activity - Rate: Variable, No relation to the atrial rate, Variable R-R interval. Baseline - ragged.
Q.40. A 58 year old woman presents to A&E with the complaint of a fall. Her medical records reveal that she has been in attendance to A&E quite frequently over the last few months because of recurrent falls. On examination, she looks slightly pale and she jokes that she is clumsier nowadays. Her past medical history includes asthma, hypertension and a previous myocardial infarction three years ago. She is on a salbutamol inhaler, a beclomethasone inhaler, amlodipine, aspirin, atenolol and bendroflumethiazide. What is the most appropriate investigation to be carried out for this patient?
Correct Answer : B
Her regular medications include multiple blood pressure-lowering agents (amlodipine, atenolol, bendroflumethiazide) which are known to cause postural hypotension. Blood pressure monitoring would be appropriate in this scenario to assess and review her medication therapy.
POSTURAL HYPOTENSION (ORTHOSTATIC HYPOTENSION):
Postural hypotension should always be considered in an elderly patient especially if he is on multiple medications and presents with dizziness. The baroreflex mechanisms that control heart rate and vascular resistance decline with age (particularly in patients with hypertension) who thus display lability in BP. They are particularly prone to postural hypotension and to the effects of drugs. It may present with dizziness or sudden loss of consciousness after getting up from a chair, with recovery within a minute.
Diagnosis :
• Blood pressure is taken when lying down and standing up. Postural hypotension is defined as a drop in BP of more than 20 mmHg after 3 minutes of standing. One of the most common causes of postural hypotension is dehydration. This is the reason that U&Es are always requested if one presents to the hospital with collapse with the likely reason being postural hypotension. A raised creatinine and urea would support dehydration. Hydration using intravenous fluids would be key if dehydration was the cause.
GOLDEN POINTS FOR DIZZINESS :
• Dizzy when rolling over the bed – Benign paroxysmal positional vertigo
• Light sensitivity during dizzy spells – Migraine
• First attack severe vertigo lasting hours with vomiting – Vestibular neuritis
• Lightheaded when getting up from bed – Orthostatic hypertension
• One ear feels full before or during the dizzy attack – Meniere’s disease
Q.41. A 76 year old man with no significant medical history presents to the clinic for his annual checkup. His only complaint is mild exercise intolerance that he attributed to his advanced age. His physical examination is only significant for an ejection systolic murmur that is louder upon auscultation with the patient in the upright position. What is the most likely cardiac defect that this patient has?
Correct Answer : C
Aortic stenosis is the most common type of valvular heart disease in patients over the age of 65 years. Remember that a congenital bicuspid value predisposes to both aortic stenosis and aortic regurgitation. A normal aortic valve has three cusps or leaflets. A clincher for exam would be an elderly patient who is complaining of exercise intolerance or who is otherwise asymptomatic. They will mention a type of systolic murmur THAT IS LOUDER WHEN THE PATIENT SITS UPRIGHT. Remember, the murmur for aortic stenosis is an ejection systolic murmur loudest in the aortic area (2nd intercostal space, right sternal border), radiates to carotids, and louder in expiration.
AORTIC STENOSIS causes :
• Degenerative calcification (most common cause in older patients above 65)
• Bicuspid aortic valve (2nd most common cause, usually in the younger age group)
Clinical features :
• Dyspnoea
• Angina
• Syncope
Remember, the murmur for aortic stenosis is an ejection systolic murmur loudest in the aortic area (2nd intercostal space, right sternal border), radiates to carotids and is louder in expiration.
Q.42. A 79 year old man with a past history of ischemic heart disease presents with yellow haloes, nausea and vomiting. His ECG reveals an arrhythmia. Which of the following medication is most likely responsible for his symptoms?
Correct Answer : D
The words “yellow haloes” are a clincher for digoxin toxicity. For exam, if you see any question with yellow-green colour vision with arrhythmia, it is most likely digoxin toxicity. Digoxin is now mainly used for rate control in the management of atrial fibrillation.
As it has positive inotropic properties it is sometimes used for improving symptoms (but not mortality) in patients with heart failure. Also remember, hypokalaemia predisposes to toxicity because potassium and digoxin bind to the same site on the sodium-potassium ATPase pump, leading to increased intracellular calcium and increased cardiac contractility.
Features of digoxin toxicity :
• Gastrointestinal symptoms are most common. These are nausea, vomiting, diarrhea, and anorexia
• Neurologic and visual symptoms include blurred vision, yellow-green vision, hallucinations and confusion
• Arrhythmias – Bradycardia, premature contractions, ventricular tachycardia, and any other type of arrhythmias may be seen. A serum digoxin level should be ordered in patients you suspect of being toxic (history, etc.)
Management of digoxin toxicity :
• Digibind - Correct arrhythmias
• Monitor potassium.
Q.43. Which is the most likely artery that has artery dominance in 85% of the general population?
Correct Answer : C
The artery that supplies the posterior descending artery (PDA) determines coronary dominance. If the posterior descending artery is supplied by the right coronary artery (RCA), then the coronary circulation can be classified as “right-dominant”.
If the posterior descending artery is supplied by the circumflex artery (CX), a branch of the left artery, then the coronary circulation can be classified as “co-dominant”. Approximately 85% of the general population are right-dominant In 85% of patients (Right Dominant), the RCA gives off the posterior descending artery (PDA). In the other 15% of cases (Left Dominant), the PDA is given off by the left circumflex artery. The PDA supplies the inferior wall, ventricular septum, and the posteromedial papillary muscle.
Q.44. A 43 year old lady is admitted with pyrexia, breathlessness and history of syncope. She was recently diagnosed with a pulmonary embolus. There is an early diastolic sound and a mid-diastoic rumble. Her jugular venous pressure is elevated with prominent a-waves. What is the most likely diagnosis?
Correct Answer : B
Atrial myxomas are benign tumours. Around three-quarters of atrial myxomas occur in the left atria, and tend to grow on the wall (septum). Sometimes small pieces of the tumour can break off and fall into the bloodstream. If this happens, they can block an artery elsewhere in the body such as the brain, which could cause a stroke, or in the lungs causing a pulmonary embolus. Around 10% of myxomas seem to be inherited (passed down through families). These are known as familial myxomas.
The symptoms occur due to obstruction of the mitral valve which results in syncope and heart failure.
Features :
• Symptoms of haemodynamic obstruction, embolization, or constitutional symptoms such as fever, malaise, tachycardia, and tachypnoea
• Symptoms and signs of ischaemia or infarction in the peripheries, due to embolization of adherent thrombus
• Atrial fibrillation
• Large myxomas may impair intracardiac blood flow, causing dyspnoea, syncope, or symptoms and signs of congestive cardiac failure
• ECHO : Pedunculated heterogeneous mass typically attached to the fossa ovalis region of the interatrial septum.
Q.45. A 50 year old female presents with shortness of breath and palpitations which has been on going for the past few hours. She has ankle swelling which has been present for more than a year and feels difficulty in breathing while lying down. She is a known alcoholic. A chest radiograph shows evidence of cardiac enlargement. What is the most likely cause of her worsening condition?
Correct Answer : A
Ankle swelling and orthopnea are features of heart failure. These features in combination with the history of alcoholism give us hints of an alcoholic cardiomyopathy which is a type of dilated cardiomyopathy. Atrial fibrillation is the most common arrhythmia that develops in patients with dilated cardiomyopathy.
Acute decompensation can occur especially in patients with asymptomatic LV dysfunction who develop atrial fibrillation. In some scenarios, there is a setting of acute alcohol use or intoxication followed by palpitations, dizziness, and syncope which can be attributed to arrhythmias such as atrial fibrillation or flutters. This is known as holiday heart syndrome because the incidence increases following weekends and during the holiday seasons.
ATRIAL FIBRILLATION PRESENTATION :
• Dyspnoea
• Palpitation
• Syncope or dizziness
• Chest discomfort or pain
• Stroke or transient ischaemic attack
• An irregularly irregular pulse.
Q.46. A 65 year old man presents with fatigue and dyspnoea 3 days after having a myocardial infarction. On auscultation he has a pansystolic murmur at the apex radiating to the axilla. What is the most likely diagnosis?
Correct Answer : D
Rupture of a papillary muscle is a rare but well-known complication of myocardial infarction. Papillary muscle rupture may lead to worsening of mitral regurgitation features including having a pansystolic murmur radiating to the axilla which is seen in this stem.
Q.47. A 62 year old woman with longstanding anxiety is seen in the outpatient department. She complains of her heart skipping a beat quite often. This particularly occurs when she is trying to get to sleep. The palpitations are never sustained. What is the most likely rhythm disturbance?
Correct Answer : C
From the given options the most likely answer is ventricular ectopics. This is a classic scenario where the patient would complain of having “missed beats”. They are usually otherwise asymptomatic. If ventricular ectopics occur in a normal heart (i.e. no cardiomyopathy or ischaemic heart disease) though symptomatic, it is benign and are of no clinical significance.
VENTRICULAR ECTOPICS: Aetiology:
• Ischaemic heart disease
• Cardiomyopathy
• Stress, alcohol, caffeine, medication, cocaine, or amphetamines
• Occurs naturally Patients may be symptomatic with palpitations often described as "skipped or missed beats" but they may also have symptoms of dyspnoea or dizziness. Over half the population have silent, or asymptomatic, ventricular ectopics which are discovered incidentally on a routine ECG.
In clinical practice, it is important to identify the presence of an underlying cardiomyopathy or ischaemic heart disease. If neither of these are present then it is likely that these ventricular ectopics are benign. Patients with no ischaemic heart disease or cardiomyopathy have an excellent prognosis however, if ventricular ectopics are secondary to heart disease like myocardial infarction, it may precipitate more life-threatening arrhythmias like ventricular fibrillation.
Q.48. A 44 year old man who presently has acute renal failure has an ECG that shows tall tented T waves, flat P waves and a wide QRS complex. What is the most likely electrolyte abnormality?
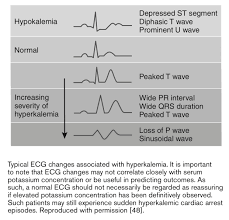
Correct Answer : A
Acute renal failure is one of the causes of hyperkalemia. Together the ECG findings point towards hyperkalemia as the answer.
ECG CHARACTERISTICS IN ELECTROLYTE DISBALANCE:
Hyperkalaemia: Tall-tented T waves, small P waves, widened QRS leading to a sinusoidal pattern and asystole.
Hypokalemia: Flat T waves, ST depression, and prominent U waves
Hypercalcaemia: Shortened QT intervals
Hypocalcaemia: Prolonged QT intervals
Q.49. A 59 year old man who is on multiple medications for ischaemic heart disease, hypertension and diabetes finds it difficult to mobilize as he feels dizzy when trying to stand up. What is the most appropriate investigation for him?
Correct Answer : A
Please see Q-40
Q.50. A 66 year old man with a history of hypertension presents to A&E with sudden, severe lower abdominal pain and back pain. A tender pulsatile abdominal mass is palpated lateral and superior to the umbilicus. His heart rate is 110/min and blood pressure is 80/50 mmHg. What is the most appropriate investigation?
Correct Answer : B
This is a classic picture of a ruptured abdominal aneurysm. An ultrasound scan is the only appropriate investigation given the options. Questions would usually have either an ultrasound or CT abdomen as one of the choices for a ruptured aortic aneurysm. Both choices are correct. It is important to note that both USS and CT scans can be performed. Although, it may be safer and quicker to perform USS in the ED, rather than transfer the patient for a CT scan.
Q.51. A 55 year old man presents to the hospital with symptoms of increasing breathlessness over the past few days and fatigue. He finds it more difficult to sleep during the nights because he is short of breath. On auscultation of his chest, basal crepitations can be heard. He has a history of chronic heart failure and hypertension of which he takes regular ramipril. Investigations were performed and furosemide infusion is given in the department which rapidly improved his symptoms. The medical team dedide to discharge him on furosemide orally with a specialist nurse follow up. What is the most appropriate medication to be added on his discharged medication list?
Correct Answer : C
As this patient is already on an ACE inhibitor, the next most appropriate class of medications would be a beta-blocker (i.e. bisoprolol, carvedilol, nebivolol) to manage his symptoms of chronic heart failure. Start with a low-dose beta blocker and titrate up once the low dose is tolerated. Remember, when starting a beta blocker, “start low and go slow”.
MANAGEMENT OF CHRONIC HEART FAILURE :
The general management of chronic heart failure can be summarized below -
• ACE-inhibitor and a beta-blocker (e.g. Carvedilol)
1st line - Spironolactone
2nd line - Digoxin
Only if heart failure is in combination with atrial fibrillation.
Both an angiotensin-converting enzyme (ACE) inhibitor and a beta-blocker are licensed to treat heart failure but it is good practice to only start one drug at a time. Clinical judgement is used when deciding which drug to start first.
For example, the preferred initial treatment might be :
• An ACE inhibitor if the person has diabetes mellitus or has signs of fluid overload
• A beta-blocker, if the person has angina.
Q.52. A 43 year old man was brought into the A&E after being stabbed in the chest with a knife. His chest is bilaterally clear. He has muffled heart sounds and his neck veins look distended. His systolic blood pressure is 60 mmHg and pulse is 120 bpm. What is the most likely diagnosis?
Correct Answer : A
The question points towards cardiac tamponade. His chest is bilaterally clear thus we can therefore exclude pneumothorax or pleural effusion. Muffled heart sounds, distended neck veins and hypotension are called Beck’s triad and it is a classical finding in cardiac tamponade.
Q.53. A 54 year old man has a temperature of 39 C, a new murmur and cardiac failure. He had a dental extraction several days ago. What is the most likely reason for his symptoms?
Correct Answer : C
Signs and consistent with infective endocarditis. A dental extraction is a known source of infection-causing bacteraemia.
INFECTIVE ENDOCARDITIS :
Fever + new murmur = endocarditis until proven otherwise
Risk Factors :
• Valve replacement
• Recreational drug abuse and invasive vascular procedures
Note: Dentistry interventions are a common cause of bacteremia leading to infective endocarditis.
Cause Strep viridans is a common cause (more than 35%)
Presentation :
• Septic signs: Fever, rigors, night sweats, malaise
• Cardiac lesion: New murmur
• Immune complex deposition: Roth spots (boat-shaped retinal haemorrhage with pale center); splinter haemorrhages, Osler’s nodes (painful pulp infarcts in fingers or toes)
• Embolic phenomena: e.g. Janeway lesions (painless palmar or plantar macules) Some patients may present with congestive cardiac failure.
Diagnosis :
Infective endocarditis is diagnosed if:
• 2 major criteria present or
• 1 major and 3 minor criteria present or
• 5 minor criteria present
Major criteria:
• Positive blood cultures
• Positive echocardiogram - showing abscess formation, new valvular regurgitation
Minor criteria:
• IV Drug user, predisposing heart condition
• Fever >38°C
• Vascular phenomena: e.g. major emboli, clubbing, splinter haemorrhages, Janeway lesions
• Immunological phenomena: Glomerulonephritis, Osler's nodes, Roth spots
• Microbiological evidence does not meet major criteria.
Q.54. A 50 year old man with diabetes mellitus suddenly develops persistent crushing central chest pain radiating to the neck and arm when he was driving. It was associated with nausea, vomiting, dyspnoea, and palpitations. He has a pulse of 122 beats/minute, a blood pressure of 110/70 mmHg and a respiratroy rate of 34 breaths/minute. What is the most likely diagnosis?
Correct Answer : D
These characteristics are classic in myocardial infarction. Do not get fooled into picking dissecting aneurysm. Although the pain of a myocardial infarction can be somewhat similar to a dissecting aneurysm, a myocardial infarction is much more common than a dissecting aneurysm.
The examiners would have to include something specific to dissecting aneurysms for that to be the answer such as a history of severe, tearing chest pain radiating to the back with a history of Marfan syndrome and unequal pulses in upper extremities. If you see any of these key phrases, you should stop and consider dissecting an aneurysm as the answer.
Q.55. A 55 year old man who suffered a myocardial infarction a few days ago is now ready for discharge. His medical history remains insignificant other than the myocardial infarction he had. He has no drug allergies. He has already been put on aspirin and clopidogrel. What is the most appropriate medication(s) to be given to him on discharge?
Correct Answer : C
ALL PATIENTS WITH MI ON DISCHARGE:
• Dual antiplatelet therapy: Aspirin + Clopidogrel
Note: Aspirin is continued lifelong Clopidogrel for 12 months
• Beta Blockers : Offer BB to people who present acutely with MI as soon as they are hemodynamically stable.
Continue a beta-blocker for at least 12 months after an MI in people without heart failure. Continue a beta-blocker indefinitely in people with HF.
• ACEi Offer ACEi to people who present acutely with MI as soon as they are hemodynamically stable. If intolerant to ACEi use ARB
• STATINS
Mnemonic: Once the patient is discharged, he can take the CAB or BAS(BUS) home.
C - Clopidogrel
A - Aspirin
B - Beta Blockers
A - ACEi
S – Statins
Q.56. A 52 year old man underwent a hemicolectomy. A few days after his operation he developes chest pain and a temperature of 38.8 C. He is having rigors and night sweats. On auscultation, a systolic murmur is heard. What is the next most appropriate investigation?
Correct Answer : C
This is a case of infective endocarditis. The most appropriate investigation is blood cultures or echocardiogram. Since an echocardiogram is not one of the options, blood cultures should be picked.
Q.57. A 71 year old woman is brought in by ambulance to the Emergency Department with sudden chest pain and shortness of breath which started 2 hours ago. The pain radiates to her left arm. There is ST elevation seen in leads II, III and aVF on the ECG. Oxygen has been started and she was given sublingual GTN which has improved her chest pain. Her heart rate is 80 bpm and respiratory rate is 18/min. What is the most appropriate next step in management?
Correct Answer : A
Percutaneous intervention (PCI) would be the best management for myocardial infarction. As PCI is not given in the option, thrombolysis would be the next best step. In terms of thrombolysis, Alteplase is preferred over streptokinase.
Q.58. A 65 year old man continues to experience chest pain 2 days after an acute myocardial infarction. He has a temperature of 37.8 C. His ECG shows widespread ST elevation with upward concavity. What is the most likely diagnosis?
Correct Answer : C
Chest pain and ECG findings of widespread ST elevation with an upward concavity are diagnostic of acute pericarditis. The history of a myocardial infarction supports this as one of the causes of acute pericarditis is a recent myocardial infarction. Fever, night sweats, and other constitutional symptoms may be present, depending on the underlying cause.
Q.59. A 55 year old man was brought to the emergency department from a shopping mall after collapsing 2 hours ago. He is now fully conscious and answering questions. His ECG shows an irregular rhythm. His blood pressure is 120/80 mmHg. What is the most appropriate investigation to carry out?
Correct Answer : C
An echocardiogram would be the best option here. It is used to identify structural cardiac abnormalities and assess left ventricular function. It may show a clot in the atrial appendage responsible for syncope which could be due to a transient ischaemic attack secondary to atrial fibrillation.
The most common valvular cause for a syncope is aortic stenosis which needs an echocardiogram to diagnose it. A Holter ECG (24-hour ECG) is not needed as the ECG is already said to have an irregular rhythm.
If they did not state that the rhythm was irregular, then 24-hour ECG would be an option. CT and MRI may be performed in selected cases (eg, aortic dissection and haematoma, pulmonary embolism, cardiac masses, pericardial and myocardial diseases, congenital anomalies of coronary arteries). However, as he has recovered fully, it is unlikely to be any of the causes requiring a CT or MRI. Exercise testing is for patients who have experienced episodes of syncope during or shortly after exertion. There was no mention of exertion in this question.
Q.60. A 6 week old baby has a pansystolic murmur at sternal border. He feeds poorly and has poor weight gain. The baby is acyanotic. What is the most likely diagnosis?
Correct Answer : C
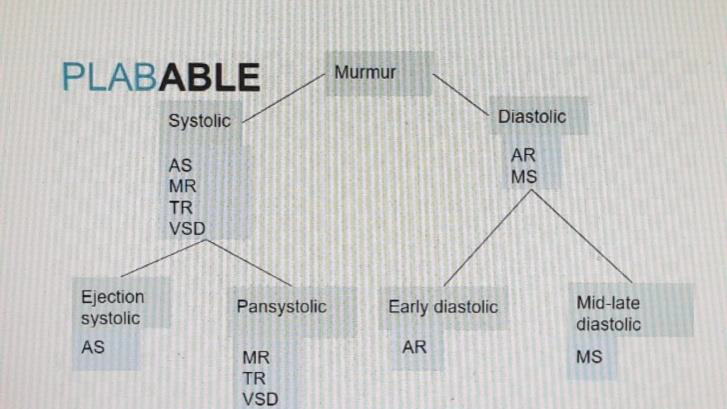
A key mnemonic that can help you get through the exam cardio question is: Pan-systolic MR, TR, VSD. Hence, when you see the words pan-systolic murmur in the question, straight away, you can cut out any options that ARE NOT mitral regurgitation, tricuspid regurgitation, and ventricular septal defect.
Ventricular septal defect :
• A hole connecting the ventricles
Causes :
• Congenital
• Acquired (post-MI)
Symptoms:
• May present with severe heart failure in infancy, or remain asymptomatic and be detected incidentally in later life.
Signs: These depend on size and site
• Small holes : Infant or child is asymptomatic with normal feeding and weight gain May be detected when a murmur is heard on routine examination Give louder murmurs. Classically, a harsh pan-systolic murmur was heard at the left sternal edge, with a systolic thrill, and a left parasternal heave. Most importantly, remember the term “pan-systolic murmur” as often that alone can give you the answer provided mitral regurgitation and tricuspid regurgitation are not one of the options.
• Large holes : Associated with signs of pulmonary hypertension. These babies may develop a right to left shunt with cyanosis or Eisenmenger’s syndrome. The diagnosis and management. Not so important for the exam.
Q.61. A 72 year old woman presents to the emergency department with chest pain. The following ECG was taken. What is the most likely diagnosis?

Correct Answer : B
-
Q.62. A 48 year old man has continuous anterior chest pain which is worse on inspiration. 4 weeks ago, he had a myocardial infarction. He has a temperature of 37.5 C. His blood results show an ESR of 82 mm/h. What is the most likely explanation for the abnormal investigation?
Correct Answer : B
DRESSLER’S SYNDROME tends to occur around 2-6 weeks following an MI. The underlying pathophysiology is thought to be an autoimmune reaction against antigenic proteins formed as the myocardium recovers. It is characterized by a combination of fever, pleuritic pain, pericardial effusion, and a raised ESR.
It is treated with NSAIDs.
Q.63. A 55 year old man with a history of a myocardial infarction three years ago presents with progressive dyspnoea. He has had two previous admissions with heart failure in the past year and complains of the inability to lie down flat on his bed. He has a respiratory rate of 31 breaths/minute and a systolic blood pressure of 90 mmHg. His oxygen saturation is 90% on room air. On examination, he looks pale and sweaty, and has widespread crepitations over both lung fields. Oxygen by face mask was commenced. What is the most appropriate investigation?
Correct Answer : A
The patient is suffering from acute pulmonary oedema brought upon by heart failure. While it is true that an ECG is important to look for arrhythmia, a chest X-ray would be a better answer given that it would be able to confirm pulmonary oedema.
This question is very debatable but the clinical picture here fits pulmonary oedema slightly better than a myocardial infarction. In reality, both will be performed.
Q.64. A 56 year old male with an established lateral myocardial infarction as seen on ECG is taken to the cardiology department for percutaneous coronary intervention (PCI). While in the catheterisation laboratory, the nurse in charge noted that he became increasingly unwell and pale. He eventually became unresponsive. An ABCDE assessment was immediately carried out and his airway was secured via an oropharyngeal mask and oxygen was administered. His vitals are as follows: Blood pressure 75/50 mmHg Heart rate 210 beats per minute Respiratory rate 4 breaths per minute Another ECG was performed and revealed a broad complex tachycardia. What is the next best step in management of this patient?
Correct Answer : A
The scenario depicted here describes a typical complication of a myocardial infarction – a tachyarrhythmia. As is clear from the stem, the patient is haemodynamically unstable.
In addition, there is the presence of a broad complex tachycardia on ECG. Therefore to answer this question correctly, it is important to know about the management of a broad complex tachycardia.
STEPS OF BROAD COMPLEX TACHYCARDIA MANAGEMENT:
1. Check the patient’s pulse - if there is no pulse, follow the arrest protocol immediately.
2. Administer oxygen
3. If the patient is haemodynamically unstable, then commence synchronized cardioversion followed by IV amiodarone and further shocks as needed In the above case, the first two steps have already been performed so the next appropriate step in management would be synchronized cardioversion.
Q.65. A 71 year old man recently feels breathless on exertion with some palpitations when resting. He finds them difficult to describe. An ECG was performed which is attached below. What is the most likely diagnosis?
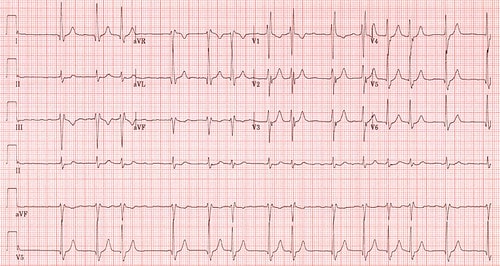
Correct Answer : D
The diagnosis here is atrial fibrillation. A completely irregular rhythm.
When looking at any ECG, try to use a stepwise approach :
Step 1: Calculate rate
Step 2: Determine regularity
Step 3: Assess the P waves
Step 4: Determine the PR interval
Step 5: Determine QRS duration
Step 6: Determine the axis
Step 7: Look at morphology
In this ECG, at step 2 (determine regularity), we can already see irregularity here just by looking at the R-R intervals. We will not discuss management here but the initial thoughts when seeing an ECG like this are :
1. Are they stable?
2. Is there rate control?
3. What is the patient’s CHA2DS2-VASc score?
Q.66. A 60 year old man with a history of ischaemic heart disease starts having chest pain. He has a heart rate of 170 beats/minute and a blood pressure of 70/45 mmHg. An ECG reveals a broad complex tachycardia with absence of atrial activity. He feels unwell and is now semi conscious. What is the most likely diagnosis?
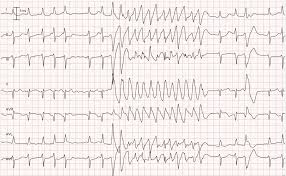
Correct Answer : B
The ECG revealing a broad complex tachycardia with the absence of atrial activity in a conscious person can only be ventricular tachycardia. The hypotension seen here supports this. Cardiac arrhythmias are more common in patients with Ischaemic heart disease hence the given history.
Occasionally, in the exam, they may include a picture of an ECG showing a broad complex tachycardia. Again, pick ventricular tachycardia if the patient is still awake as it is impossible to see ventricular fibrillation in an awake patient.
Ventricular tachycardia may impair cardiac output with consequent hypotension, collapse, and acute cardiac failure.
This is due to extreme heart rates and lack of coordinated atrial contraction (loss of “atrial kick”).
The rate of V. Tach is from about 100-250 bpm. P Waves may be present or absent. P waves are usually not seen if the rate is increased. If present, the P Waves have no relation to the QRS complexes of the V. Tach.
V. Tach can present in two ways.
1. With Pulse
a) Haemodynamically stable or
b) Haemodynamically unstable — e.g. hypotension, chest pain, cardiac failure, decreased conscious level.
2. Without Pulse Management depends on how the patient presents:
1. With Pulse
a) Haemodynamically stable antiarrhythmics e.g. amiodarone, lidocaine, procainamide
b) Haemodynamically unstable — e.g. hypotension, chest pain, cardiac failure, decreased consciousness level. immediate electrical cardioversion is indicated
2. Without Pulse, immediate electrical cardioversion is indicated.
Q.67. A 44 year old woman in the postnatal ward develops sudden onset chest pain and shortness of breath. She had an emergency C-section for fetal distress two days ago. She feels the breathlessness worsen when she lies down. She has a respiratory rate of 32 breaths/minute and a blood pressure of 100/60 mmHg. Her oxygen saturation is 89% on room air and temperature is 36.9oC. On examination, she looks pale and sweaty. Auscultation reveals widespread crepitations over both lung fields. An ECG was performed which shows sinus tachycardia. Oxygen by face mask was commenced. A chest X-ray confirms the diagnosis. Which medication is used as part of the management?
Correct Answer : A
The patient is suffering from acute pulmonary oedema brought upon by heart failure. It is worth noting that this stem is a little tricky as there were no risk factors of heart failure mentioned and the information that the woman had a recent C-section makes physicians (especially if you have worked in an obstetric unit), think of a pulmonary embolism. However, it is important to be aware that cardiac causes of breathlessness do occur in pregnancy and post-delivery as well. This stem gives the history of orthopnea which points towards heart failure as the reason for the shortness of breath.
In terms of the management of acute pulmonary oedema, 4 important steps need to be done:
1. Sit the patient up, and give oxygen – aim for saturations. 95% (>90% in those with COPD)
2. Glyceryl trinitrate (GTN) spray two puffs sublingual
3. Furosemide 40 mg intravenously (slowly) produces transient venodilation and subsequent diuresis
4. Diamorphine 2.5-5 mg intravenously slowly (or morphine 5-10 mg intravenously slowly) can be used to relieve anxiety, pain, and distress.
Q.68. A 54 year old female presents with the inability to lie down flat on her bed at night. On examination, she has widespread bibasilar crepitations on auscultation and an irregularly irregular radial pulse. Her past medical history is significant for an anterolateral myocardial infarction a year ago. Auscultation of the heart reveals a 2/6 grade pansystolic murmur at the cardiac apex. She has no other medical problems. She does not drink alcohol or smoke. What is the most likely cardiac defect that this patient has?
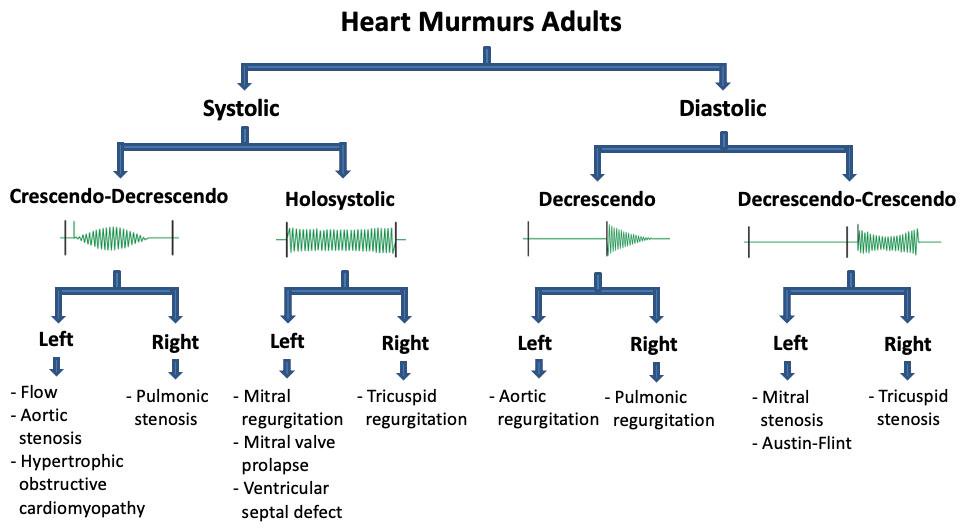
Correct Answer : D
It is clear from the stem that this patient has mitral regurgitation.
There are two types of mitral regurgitation: Primary (degenerative) MR and secondary (functional) MR. From the patient’s past medical history, we can see that she has had a relatively recent myocardial infarction. The most important complications of a myocardial infarction that we need to recognize in this stem are mitral valve dysfunction and atrial arrhythmia.
VALVULAR HEART DISEASE :
We have listed the common heart valve disorders here. There are certain keywords that if you see in the exam, would help point you towards a specific heart valve disorder.
Aortic valve stenosis is the most common valvular heart disease, hence the most commonly asked heart valve question. The two most common pathogenesiss are age-related degenerative sclerocalcific changes to valves (the most common cause, usually an elderly patient) and congenital bicuspid aortic valve (seen in a younger person with aortic stenosis).
Signs : Ejection systolic murmur is best heard at the 2nd intercostal space, at the right sternal border which radiates to carotid arteries.
Mitral regurgitation (MR), which is also known as mitral insufficiency, is the second most common heart valve disorder.
Signs : Soft S1 and S2, pan systolic murmur at the 5th intercostal space in the left midclavicular line which radiates to the axilla.
A useful method to remember is to remember this phrase “When cooking, you do not want to regurgitate onto the cooking pan”. This is a good way to remember pan systolic murmurs are found in mitral and tricuspid regurgitation (and also in ventricular septal defects).
Mitral valve prolapse is a common inheritable connective tissue disorder like Marfan’s syndrome, Ehlers-Danlos syndrome, and osteogenesis imperfecta. Most patients are asymptomatic. The classical case would be a slim young female with low blood pressure. Mitral valve prolapse is a risk factor for mitral regurgitation.
Signs: Mid-systolic click, best heard at the 5th intercostal space in the left midclavicular line, followed by a mid or late-systolic murmur with findings accentuated in the standing position.
Mitral stenosis : Rheumatic heart disease is the most common cause of mitral stenosis worldwide.
Signs : Mid-diastolic murmur with an opening click (the click represents the mitral valve opening) is best heard at the 5th intercostal space in the left midclavicular line.
Aortic regurgitation causes include rheumatic heart disease, infective endocarditis, and Marfan syndrome amongst others.
Signs : Early diastolic murmur, best heard at left sternal edge
Pulmonary stenosis Signs : Ejection systolic murmur best heard over the pulmonary area, radiates to the left shoulder or infraclavicular region.
Tricuspid regurgitation Signs : Pansystolic murmur is best heard over the tricuspid region.
Other common mnemonics that can help you remember heart murmurs are:
Left-sided murmurs louder with expiration
Right-sided murmurs louder with inspiration.
Q.69. A 50 year old man presents with a stab wound to his left anterior chest at the level of the 4th intercostal space. On physical examination, his neck veins are dilated, heart sounds are faint and trachea is central. He has a systolic blood pressure of 80 mmHg and a pulse rate of 130 bpm. What is the most likely diagnosis?
Correct Answer : C
This question points towards cardiac tamponade. Muffled heart sounds, distended neck veins and hypotension are called Beck’s triad and it is a classical finding in cardiac tamponade.
CARDIAC TAMPONADE : A life-threatening condition in which a pericardial effusion has developed so rapidly or has become so large that it compresses the heart.
Aetiology -
• Usually penetrating or blunt chest trauma
Features -
• Dyspnoea
• Raised JVP - seen by having neck veins which are distended
• Tachycardia
• Hypotension
• Muffled heart sounds
• Pulsus paradoxus
Remember Beck’s triad: Muffled heart sounds, distended neck veins, and hypotension
Diagnosis -
• Echocardiography
Treatment - Pericardiocentesis.
Q.70. A 65 year old man presents to the emergency department with chest pain, palpitations and shortness of breath. The following ECG was taken. He was given a glyceryl trinitrate spray and morphine which has improved his chest pain. What is the most appropriate action?
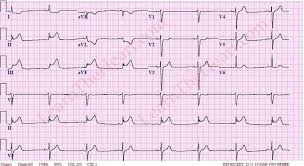
Correct Answer : D
This is a classical ECG showing an inferior myocardial infarction. See the leads II, III, and aVF which show an ST elevationPercutaneous intervention (PCI) would be the best management for myocardial infarction.
Q.71. A 69 year old man was successfully thrombolysed for an inferior myocardial infarction 15 days ago and was discharged 5 days after the thrombolysis. He is now re-admitted as he is hypotensive, tachycardic and with pulmonary oedema. What is the most likely diagnosis?
Correct Answer : C
Acute mitral regurgitation post- MI. This is a mitral regurgitation due to ischaemic papillary muscle dysfunction or partial rupture. It is usually seen 2-10 days post myocardial infarction. It is more commonly associated with inferior myocardial infarction than anterior myocardial infarction. ‘Silent MR’ is quite frequent and must be suspected in any post-MI patient with unexplained haemodynamic deterioration.
Diagnosis- Echocardiogram
Treatment- Acute MR is treated with vasodilator therapy but often requires emergency surgical repair.
Q.72. A 57 year old woman who is suffering from hypertension, presents to the hospital with complaints of recurrent falls when trying to get out of bed or getting up from sitting. She is on antihypertensive therapy with no other medical problems. What is the most likely cause of her falls?
Correct Answer : A
One of the many known adverse effects of thiazides is postural hypotension. Common adverse effects of thiazides worth remembering include:
• Postural hypotension
• Hyponatraemia, hypokaleimia
• Gout
Q.73. A 52 year old man has a suspected diagnosis of a patent foramen ovale while undergoing a transthoracic echocardiography. What is the next most appropriate investigation to confirm the diagnosis?
Correct Answer : D
Transoesophageal echocardiography (TOE) with bubble contrast is the gold standard for the diagnosis of patent foramen ovale. In the absence of TOE, transthoracic echocardiography (TTE) may also be considered. However, a bubble contrast is essential to evaluate a functional right-to-left shunt.
However, it cannot differentiate an intracardiac from a pulmonary shunt.
Q.74. A 55 year old carpenter presents with a history of sudden chest pain which radiates to his jaw accompanied by shortness of breath which started 2 hours ago. An ECG was done which shwos a normal sinus rhythm without ST elevation. What is the most appropriate investigation?
Correct Answer : C
We are suspecting a myocardial infarction in this patient. Cardiac enzymes would need to be ordered. Measurement of cardiac troponins helps to predict which patients are at risk of a cardiac event, and who can be safely discharged early. The risk of death from an ACS is directly related to troponin level and patients with no detectable troponins have a good short-term prognosis.
Serum levels increase within 3-12 hours from the onset of chest pain, peak at 24-48 hours, and return to baseline over 5-14 days. Troponin levels may therefore be normal initially and should be repeated.
Myocardial muscle creatine kinase (CK-MB) is found mainly in the heart. CK-MB levels increase within 3-12 hours of the onset of chest pain, reach peak values within 24 hours, and return to baseline after 48-72 hours. Sensitivity and specificity are not as high as for troponin levels.
Q.75. A 69 year old man has sudden onset chest pain radiating to his left arm while watching television. An ambulance was rushed to the scene and an electrocardiogram shows ST elevation in II, III and aVF. What is the most appropriate analgesia to administer to him while in the ambulance?
Correct Answer : C
Myocardial infarction is a painful condition seen as tightness, pressure, or squeezing pain in the chest. The ECG shows that he is having an inferior myocardial infarction. Pain relief with GTN sublingual or spray and/or an intravenous opioid 2.5-5 mg diamorphine or 5-10 mg morphine intravenously with an anti-emetic is often used as part of the pre-hospital management. Remember, nitrates bring relief to many patients, but up to one-third of those who experience a myocardial infarction have nitrate-resistant chest pain and should receive morphine to help manage the pain.
Avoid intramuscular injections of opioid medication even while in the ambulance, as absorption is unreliable. In addition, the injection site may bleed if the patient later receives thrombolytic therapy.
Q.76. A 74 year old man started having chest pain. He has a blood pressure of 70/50 mmHg. He is conscious and a radial pulse is felt. An ECG shows the following rhythm. What is the most likely diagnosis?
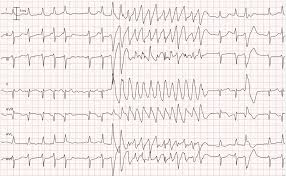
Correct Answer : D
Please see Q-16
Q.77. A 65 year old man presents with recurrent light headedness for one month especially when he gets up from bed in the morning. He also has occasional episodes of lightheadedness when standing for prolonged periods of time. He suffers from hypertension and type 2 diabetes. His regular medications include atenolol, amlodipine, bendroflumethiazide and metformin. On physical examination, his blood pressure was 125/85 mmHg taken when he was supine and 101/69 mmHg when standing. What is the most likely diagnosis?
Correct Answer : A
Please see Q-40
Q.78. A 62 year old woman who had stroke a year ago now reports having increased dyspnoea on exertion. An ECG was performed which showed an atrial fibrillation. Chest X-ray shows a straight left heart border. What is the most likely diagnosis?

Correct Answer : B
The clincher here is the chest X-ray that shows a straight left heart border. This is classic for mitral stenosis where the left atrium enlarges. The rest of the symptoms also match the diagnosis of mitral stenosis. The history of stroke given in this question is a clue that she has had atrial fibrillation for a while and had a systemic embolism (due to stagnation of blood in an enlarged left atrium).
MITRAL VALVE STENOSIS :
• Most commonly due to rheumatic fever
• Results in right ventricular failure
Aetiology: Most cases are secondary to rheumatic fever (This is extremely important to remember for the exam)
Pathogenesis:
• Mitral valve stenosis impedes left ventricular filling
• Increased left atrial pressure is referred to the lungs, causing pulmonary congestion
• Forward cardiac output becomes reduced, secondary pulmonary vasoconstriction occurs, and eventually right ventricular failure results
Clinical symptoms: Usually manifest slowly over the years
• Dyspnoea
• Orthopnoea
• Paroxysmal nocturnal dyspnoea
• Right-sided heart failure
• Hepatomegaly
• Ascites
• Peripheral oedema
The following are presentations that are rare and unlikely to be asked:
• Haemoptysis (due to rupture of pulmonary vessels due to raised atrial pressure)
• Systemic embolism (due to stagnation of blood in an enlarged left atrium)
Physical signs:
• Malar flush on the cheeks
• Atrial fibrillation
Pulmonary rales
• Loud S1 (This is particularly important to note for the exam)
• Diastolic rumble (low-pitched apical murmur)
Diagnosis:
1. ECG -
• May show signs of right ventricular hypertrophy
• Atrial fibrillation may be seen
• P mitrale
2. Chest X-ray -
• Large left atrium, Straightening of the left heart border
• Pulmonary hypertension, including Kerley B lines and increased vascular markings
3. Echocardiography -
• Thickening of mitral valve leaflets.
Q.79. A 52 year old man presents with increased breathlessness when walking. He finds it difficult to sleep at night due to shortness of breath and has to either roll on his side or use a few pillows for his head and upper back to reduce his symptoms. His symptoms have been worsening for the past 5 months. He is currently taking furosemide which gives him some relief. His medical history is significant for diabetes mellitus. On examination, bilateral pedal oedema is noted. What is the most appropriate next step in management?
Correct Answer : A
This patient is suffering from chronic heart failure. Given that this patient has diabetes mellitus, an ACE-inhibitor like ramipril would be more appropriate when compared to a beta blocker.
Q.80. A preterm neonate who was born at 32 weeks has a continuous murmur that disappeared at the time of discharge from the paediatric intensive care unit. What is the most likely diagnosis?
Correct Answer : B
PDAs are very common in preterm babies and they also may close spontaneously and can have significant physiological effects.
• The continuous murmur (rarely heard)
• There may be a rough systolic murmur along the left sternal border
• Bounding peripheral pulses
• The diagnosis is confirmed by echocardiography which not only allows the PDA to be visualised but also assesses the haemodynamic significance of the PDA
• PDA may close spontaneously
• Indomethacin closes the connection in the majority of cases.
Q.81. A 69 year old man is brought in by ambulance to the Emergency Department with central crushing chest pain which radiates to his left arm. On reporting the ECG, he was diagnosed with an acute myocardial infarction. What is the most likely ECG findings that would lead to this diagnosis?
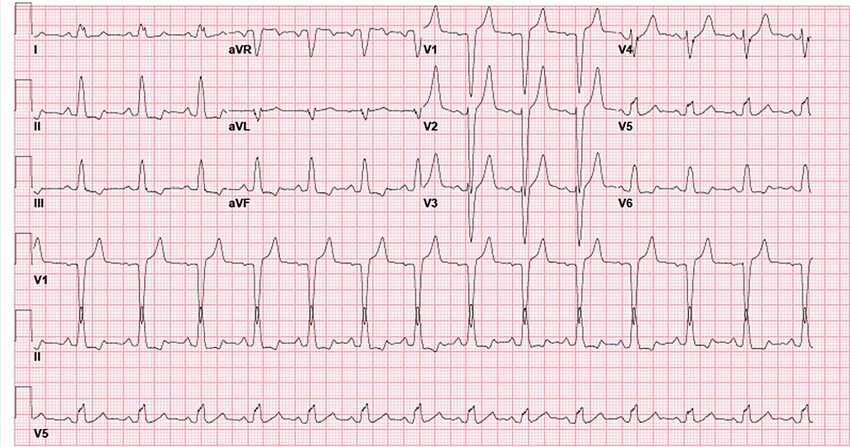
Correct Answer : C
LEFT BUNDLE BRANCH BLOCK (LBBB):
It is always good to be able to recognize a LBBB on an ECG. LBBB is best seen in lead V6, where you would see a broad complex with an “M” morphology. This broad complex “M” morphology can also be seen in leads I and aVL.
Other ECG features of LBBB include:
• Left axis deviation
• Deep S-wave in V1Below are some ECG examples with LBBB seen
• Broad complex “M” morphology seen in leads I and aVL
• Broad complex in V6
• Deep S-wave in V1
• Broad complex “M” morphology seen in leads I
• Broad complex in V6
• Deep S-wave in V1.
Q.82. A 59 years old man returns for routine follow up 6 weeks following a myocardial infarction. He complains of breathlessness when walking uphill. His ECG shows ST elevation in leads V1, V2, V3, V4 and V5. What is the most likely explanation for the abnormal finding?
Correct Answer : B
The two closest options here are left ventricular aneurysm and Dressler’s syndrome. One needs to understand them for the exam. Left ventricular aneurysm is usually a complication resulting from a myocardial infarction. When the cardiac muscle partially dies during a myocardial infarction, a layer of muscle may survive, and being severely weakened, start to become an aneurysm. It usually presents four to six weeks post-myocardial infarction which fits this stem and ECG shows persistently raised ST segments.
Dressler’s syndrome is a secondary form of pericarditis that occurs post-myocardial infarction. It usually presents one-week post myocardial infarction but may also occur several months after a myocardial infarction. Clinical features consist of fever, pleuritic pain, pericardial and pleural effusion. The pleuritic pain is usually the main complaint. As we can see from the presenting symptoms of the patient, a left ventricular aneurysm fits best.
Q.83. A 60 year old woman with a history of ischaemic heart disease presents to A&E with progressive dyspnoea. She has had previous admissions with heart failure in the past year. She has a respiratory rate of 34 breaths/minute and a systolic blood pressure of 90 mmHg. Her oxygen saturation is 88% on room air. On examintion, she looks pale and sweaty, and has widespread crepitations over both lung fields. Oxygen by face mask was commenced. What is the most approprite next step in management?
Correct Answer : A
This patient is suffering from acute pulmonary oedema brought upon by heart failure.
Q.84. A 28 year old man complains of heart racing. He is completely conscious throughout. He has a pulse of 132 beats/minute, a blood pressure of 120/70 mmHg and a respiratory rate of 21 breaths/minute. An ECG was taken which shows supraventricular tachycardia. What is the most appropriate immediate management?
Correct Answer : A
This patient is stable.
Treatment for SVT in stable patients always begins with Valsalva maneuvers followed by carotid massage followed by adenosine provided there are no contraindications for it.If this patient had asthma, verapamil would be a better option. DC cardiovert only if the patient is haemodynamically unstable or if you have given 3 doses of adenosine and the patient is still in SVT.
Q.85. A 52 year old man with a BMI of 27 is being treated for hypertension. He drinks around 8 units of alcohol per week and smokes 20 cigarettes a day. His lipid profile was done and shows a cholesterol of 4.2. What is the best referral for him?
Correct Answer : B
Smoking is the number one factor for all-cause mortality of coronary artery disease and peripheral arterial disease. To reduce his risk of getting heart disease, the best referral for him would be a smoking cessation clinic. This man is well within the allowed consumption of alcohol per week so referring him to an alcohol support group is correct.
Q.86. A 69 year old man has the following ECG. What is the most appropriate next step in management?

Correct Answer : C
The diagnosis here is atrial fibrillation.
The hallmark of atrial fibrillation is the absence of P waves. Instead, irregular fibrillatory waves called “f waves” are seen which produced a ragged baseline. Atrial fibrillation can be differentiated from atrial flutter by the irregular ventricular rate.
Atrial flutter has a more regular ventricular rate. Atrial flutter also has the classical “saw tooth pattern”.
Q.87. A 55 year old man has central chest pain that radiates to his shoulders and arm. It is relieved by sitting up and leaning forward. Pericardial friction rub is heard. A widespread ‘saddle-shaped’ ST elevation is seen on an ECG. The cardiac shadow is not enlarged on a chest X-ray. What is the most likely diagnosis?
Correct Answer : B
Chest pain and ECG findings of widespread ST elevation with an upward concavity are diagnostic of acute pericarditis. The cardiac shadow seen on a chest X-ray is not enlarged in dry pericarditis. A pericardial friction rub is frequently heard in acute pericarditis.
This is a superficial, scratchy, grating sound that is best heard in the second to fourth intercostal spaces when pressure is exerted on the diaphragm of the stethoscope.
Q.88. A 55 year old woman was found collapsed at home. The paramedics revived her but in the ambulance she had a cardiac arrest and could not be saved. The paramedic’s report states that the woman was immobile lately due to hip pain and that they found ulcers on the medial side of ankle. She has a history of diabetes mellitus and was on anti-diabetics. What is the likely cause of her death?
Correct Answer : C
The two top choices here are acute myocardial infarction (a silent MI) or pulmonary embolism due to immobilization which may result in deep vein thrombosis.
Given the history of immobilization, pulmonary embolism should be suspected.
Q.89. A 58 year old man suddenly becomes shocked several days after suffering an acute myocardial infarction. His chest X-ray shows a large globular shaped heart and clear lung fields. His neck veins look distended. What is the most likely diagnosis?
Correct Answer : A
A myocardial infarction can cause acute pericarditis which can lead to pericardial effusion. A chest X-ray shows an enlarged globular heart at this stage. A pericardial effusion of a significant amount can cause cardiac tamponade which shows up as a sign of shock.
One can expect his blood pressure to be low and his JVP to be high.
Q.90. An 18 year old man complains of fatigue and dyspnoea. On examination, he has left parasternal heave and systolic thrill with a harsh pan-systolic murmur at left parasternal edge. What is the most likely diagnosis?
Correct Answer : C
Please see Q- 60
Q.91. A 60 year old lady has severe chest pain. ECG shows changes of inferior wall myocardial infarction. The ECG also shows progressive prolongation of PR interval until a QRS complex is dropped. What is the most likely diagnosis?
Correct Answer : B
Inferior myocardial infarction is frequently associated with conduction defects.
Mobitz type I AV block (also known as Wenckebach’s phenomenon) There is a progressive prolongation of the P-R interval following each atrial impulse until an atrial impulse fails to be conducted to the ventricles causing a ‘dropped beat’.
Q.92. A 46 year old African-Caribbean man is found to have blood pressure of 160/90 mmHg on 3 separate occasions. What is the most appropriate initial treatment?
Correct Answer : C
Since the patient has Afro-Caribbean origins calcium channel blockers would be the best antihypertensive medication to start. Afro-Caribbeans tend to develop low-renin, salt-sensitive type hypertension.
Monotherapy for hypertension with beta-blockers or ACE inhibitors is less effective than calcium channel blockers in this particular ethnicity.
Q.93. A 76 year old diabetic man was recently admitted after being found to be in atrial fibrillation. He has no other medical conditions and takes metformin regularly. His fibrillation was managed in hospital and he was deemed safe for discharge. On discharge, what is the most appropriate long term medication for this patient?
Correct Answer : A
This patient is at high risk of stroke with a CHA2DS2-VASc score of 3 (2 for age and 1 for diabetes). Anticoagulation using warfarin is the most appropriate long-term management in these options to prevent stroke.
Q.94. A 28 year old man presents with a 2 hours history of rapid palpitations. He feels lightheaded but is otherwise well. On examination he has a pulse of 170 beats/minute, regular. His blood pressure is 100/68 mmHg. He had 2 similar episodes of feeling palpitations in the past 3 months. What is the most likely rhythm disturbance?
Correct Answer : B
The given history of palpitations, lightheadedness with tachycardia plus a history that this has occurred before, gives the likely diagnosis of supraventricular tachycardia.
Q.95. A 66 year old man has presented to the Emergency Department with a facial droop, arm weakness and speech difficulties that started 2 hours ago. A computed tomography scan of head shows no evidence of an acute haemorrhage. An ECG was performed which shows an atrial fibrillation. There is no history of atrial fibrillation in the past. He was managed by the medical team and was thrombolysed and currently awaiting discharge. He has been informed by the medical team that he suffered from a non-disabling ischaemic stroke. He has no other medical conditions. What is the most appropriate long term prophylactic regimen for stroke prevention for him?
Correct Answer : B
Firstly, we must define what a non-disabling ischaemic stroke is. It is defined as an ischaemic stroke with symptoms that last for more than 24 hours but later resolve, leaving no permanent disability. The reason this is important is often anticoagulation treatment is deferred for at least 14 days from the onset in people with disabling ischaemic stroke for a fer of a haemorrhagic event. In the interim aspirin 300 mg daily will be used.
For non-disabling ischaemic strokes, it depends on specific circumstances. Nonetheless, in this question, they are asking for a long-term prophylactic regimen and thus warfarin is still the best option whether it started in 14 days or right away. He has atrial fibrillation which could lead to another stroke which is the reason that anticoagulation is extremely important. If atrial fibrillation was not included in this question, then the answer would be aspirin for 2 weeks and clopidogrel long-term for stroke prevention.
Q.96. A 69 year old hypertensive white British man is currently on Indapamide 2.5 mg daily but his blood pressure is still high. Which of the following is the best choice to add in order to control his blood pressure?
Correct Answer : C
You should be able to recognize that the patient is currently on Step 1 of the NICE hypertension treatment pathway. Persons aged over 55 or black persons of African or Caribbean family origin of any age with hypertension, offer antihypertensive treatment with a CCB.
If a CCB is not suitable, for example, because of oedema or intolerance, or if there is evidence of heart failure or a high risk of heart failure, offer a thiazide-like diuretic. He should therefore commence with Step 2 by adding an ACE inhibitor or an angiotensin-II receptor blocker. An increase in his Indapamide dose is not recommended as doses larger than 2.5 mg daily showed no appreciable antihypertensive effect but a diuretic effect may become apparent.
Q.97. A 57 year old man presents to A&E with central abdominal and lower back pain associated with feeling faint and sweaty. The pain started very suddenly and it is very severe. His heart rate is 105 bpm and blood pressure is 88/50 mmHg. On physical examination, there is a tender pulsatile abdominal mass and his left femoral pulse is absent. What is the most approprite initial investigation?
Correct Answer : D
This is a classic picture of a ruptured abdominal aneurysm. An ultrasound scan is the only appropriate investigation given the options. Questions would usually have either an ultrasound or CT abdomen as one of the choices for a ruptured aortic aneurysm.
Both choices are correct. It is important to note that both USS and CT scans can be performed. Although, it may be safer and quicker to perform USS in the ED, rather than transfer the patient for a CT scan.
Q.98. A 45-year-old lady has 10 months history of shortness of breath. She is found to have irregularly irregular pulse and loud P2 with fixed splitting and ejection systolic murmur in left 2nd intercostal space. What is the probable diagnosis?
Correct Answer : B
Atrial septal defect.
Most adult patients with a large defect present with (some or all) symptoms including fatigue, exercise intolerance, palpitations, syncope, shortness of breath, peripheral oedema, thromboembolic manifestations, and cyanosis. Arrhythmias are more common after 40 years of age. The common arrhythmias are atrial flutter and atrial fibrillation.
Auscultatory findings are: Loud P2 with fixed splitting of 2nd heart sound.
A left-to-right shunt caused increased loading on the right ventricle, leading to delayed emptying and therefore delayed closure of the pulmonary valve which caused this splitting. Soft systolic ejection murmur in the pulmonary area at the upper left sternal border.
A diastolic rumble over the left lower sternum because of increased flow through the tricuspid valve. Classic auscultatory findings as described above are not present unless the shunt is reasonably large.
Q.99. A 64-year-old man has recently suffered from an MI and is on aspirin, atorvastatin and ramipril. He has been having trouble sleeping and has been losing weight for the past 4 months. He doesn’t feel like doing anything he used to enjoy and has stopped socializing. He says he gets tired easily and can’t concentrate on anything. What is the most appropriate treatment?
Correct Answer : C
Citalopram.
Depression is common among patients recovering from a myocardial infarction. Approximately 1 in 6 patients with MI experience major depression and at least twice as many as that have significant symptoms of depression soon after the event.
Post -MI depression is an independent risk factor for increased mortality (as depression is associated with poor compliance with risk-reducing recommendations).
For treating this depression SSRIs are recommended as first-line agents and among SSRIs Sertraline is the drug of choice for ischemic heart disease. The next choice is citalopram (as it is often related to torsades de pointes it is not 1st choice). If SSRI cannot be used Mirtazapine is recommended as the next antidepressant.
Q.100. A 75-year-old man collapsed while walking in his garden. He recovered fully within 30 minutes with BP 110/80 mmHg and regular pulse of 70 bpm. He has a systolic murmur on examination. His activities have been reduced lately which he attributes to old age. What is the definitive diagnostic investigation that will assist you with his condition?
Correct Answer : B
This is a case of exercise-related syncope.
Exercise-related syncopes are of 2 types,
i) Syncope during exercise or exertional syncope (this is ominous)
ii) Post exercise syncope (this is benign).
A few examples of Syncope during exercise- are arrhythmia, valvular heart disease, structural heart disease like hypertrophic cardiomyopathy, coronary artery disease, myocarditis, etc.
Example of Syncope following exercise- orthostatic hypotension as in the case of exercise in a hot environment with vasodilation and increased sweating, prolonged standing, vasovagal related to a sudden decrease in venous return, etc.
Given cause is exertional syncope and systolic murmur indicate valvular lesions (particularly aortic stenosis) in this elderly man.
Q.101. A 65-year-old man with hypertension presents with lower abdominal pain and back pain. An expansive abdominal mass is palpated lateral and superior to the umbilicus. What is the most discriminating investigation?
Correct Answer : D
Abdominal aortic aneurysm (AAA or triple A) is a localized enlargement of the abdominal aorta such that the diameter is greater than 3 cm or more than 50% larger than normal. They usually cause no symptoms, except during rupture. Occasionally, abdominal, back, or leg pain may occur. A single most discriminating investigation is abdominal ultrasound.
Q.102. A 54-year-old man has recently been diagnosed with moderate depression. He has history of MI and is suffering from insomnia. What is the drug of choice for him?
Correct Answer : A
Depression is common among patients recovering from a myocardial infarction. Post -MI depression is an independent risk factor for increased mortality.
For treating this depression SSRIs are recommended as first-line agents and among SSRIs Sertraline is the drug of choice for ischemic heart disease. The next choice is citalopram (as it is often related to torsades de pointes it is not 1st choice). As the patient has insomnia and citalopram can cause insomnia too, it should be taken in the morning. If SSRI cannot be used Mirtazapine is recommended as the next antidepressant.
Q.103. Which finding, on clinical examination of the pulse, suggests a diagnosis of hypertrophic obstructive cardiomyopathy (HOCM)?
Correct Answer : D
Pulsus bisferiens, is a sign where, on palpation of the pulse, a double peak per cardiac cycle can be appreciated. Bisferious means striking twice.
Classically, it is detected when aortic insufficiency exists in association with aortic stenosis, but may also be found in hypertrophic obstructive cardiomyopathy.
Q.104. A man with prosthetic heart valve underwent hemicolectomy and after some days complains of left hypochondriac pain, fever and has a systolic murmur. What is the next investigation to ascertain the cause of HF?
Correct Answer : B
The diagnosis is infective endocarditis.
Fever + new murmur suggest endocarditis until proven otherwise.
Important risk factors: dermatitis, IV injections, renal failure, organ transplantation, DM, post-operative wound.
Risk of developing endocarditis in following abnormalities of valves: aortic or mitral valve disease, tricuspid valve in IV drug users, prosthetic valves.
Q.105. A 45-year-old lady has 10 months history of SOB (shortness of breath). She is found to have irregularly irregular pulse and loud P2 with fixed splitting and ejection systolic murmur in left 2nd ICS. What is the probable diagnosis?
Correct Answer : B
Diagnosis is ASD with atrial fibrillation.
i) Atrial fibrillation = irregularly irregular pulse.
ii) ASD = SOB, fixed splitting with loud P2, ESM in pulmonary area]. This picture is typical. One should not misdiagnose SOB, ESM in the pulmonary area, and loud P2 as pulmonary hypertension (though in the elderly this can develop with ASD).
Q.106. A 72-year-old man has been advised to have antibiotic prophylaxis for some years now before dental treatment. He has never experienced chest pain. Three weeks ago, he noticed breathlessness on exertion and for one week he had orthopnea. His pulse is normal. What is the most probable diagnosis?
Correct Answer : D
Antibiotic prophylaxis points towards rheumatic fever. Present complaints of breathlessness and orthopnea suggest probable valvular disease. Mitral stenosis is the most common valvular complication of rheumatic fever.
Q.107. A 67-year-old man presents with palpitations. ECG shows an irregular rhythm and HR 140bpm. He is otherwise stable, BP 124/80 mmHg. What is the most appropriate management?
Correct Answer : A
In acute AF (<48h) if stable, rate control by verapamil or bisoprolol.
In chronic AF (>48h) rate control with beta-blocker or rate limiting CCB.
Q.108. A 67-year-old man had successful thrombolysis for an inferior MI 1 month ago and was discharged after 5 days. He is now readmitted with pulmonary edema. What is the most probable diagnosis?
Correct Answer : B
Ischaemic mitral regurgitation > raised pulmonary capillary pressure > pulmonary oedema. Inferior myocardial infarction causes left ventricular remodeling, which displaces posterior papillary muscle away from its normal position, leading to ischemic mitral regurgitation.
Q.109. A 60-year-old lady who had stroke 3 years ago now reports having increased dyspnea on exertion and atrial fibrillation. CXR: straight left border on the cardiac silhouette. What is the most probable diagnosis?
Correct Answer : D
Points in favour of rheumatic valve stenosis:
i) Dyspnoea on exertion
ii) Straight left border of the cardiac silhouette. Straightening the left heart border requires underfilling of the left ventricle and aorta, which occurs in mitral stenosis.
iii) Atrial fibrillation is a common association.
Q.110. A 60-year-old diabetic complains of pain in thigh and gluteal region on walking up the stairs for the last 6 months. She is a heavy smoker and has ischemic heart disease. What is the most appropriate diagnosis?
Correct Answer : D
Atherosclerotic narrowing of vessels produces these symptoms.
Why atherosclerosis? There is other vasculopathy as IHD. Smoking is a risk factor for atherosclerosis.
Now if we think of exclusion:
i) It is not sciatica as sciatica pain is worse when sitting. There may be weakness, numbness, or difficulty moving the leg or foot. A constant pain on one side of the rear. A shooting pain that makes it difficult to stand up.
ii) It is not DVT as no swelling, warmth or redness of the skin is there
iii) It is not thromboangitis obliterans as pulses are ok, no colour change or reduced hair growth, no ulceration or gangrene
iv) Not embolism as no pain (rest pain), no numbness, not pale or blue, no rash, no ulceration of skin.
Q.111. A 50-year-old man has a stab wound to his left anterior chest at the level of the 4th ICS. He has a BP 80 mmHg, pulse 130bpm. His neck veins are dilated and his heart sounds are faint. His trachea is central. What is the most appropriate diagnosis?
Correct Answer : A
Beck's triad is a collection of three medical signs associated with acute cardiac tamponade, an emergency condition wherein fluid accumulates around the heart and impairs its ability to pump blood. The signs are low arterial blood pressure, distended neck veins, and distant, muffled heart sounds.
Q.112. A 28-year-old man with complains of headache and nose bleeds also has pain in the lower limbs on exertion. Examination: radio-femoral delay, cold legs with weak pulse and mild systolic murmur with normal S1S2. What is the most probable diagnosis?
Correct Answer : C
Coarctation of the aorta :
Headache and nosebleeds - >hypertension, pain in lower limb on exertion -> as reduced blood supply to leg due to coarctation.
Radio-femoral delay, cold legs with a weak pulse and mid-systolic murmur are all features of coarctation of the aorta.
Q.113. A 75-year-old lady who had mitral valve replacement 13 years ago has developed recurrent breathlessness. Her husband has noticed prominent pulsation in her neck. She complains of abdominal pain and ankle swelling. What is the most probable diagnosis?
Correct Answer : D
Tricuspid regurgitation.
Long standing complication of mitral valve replacement is tricuspid regurgitation. In tricuspid regurgitation there is recurrent breathlessness (mostly exertional), prominent pulsation in the neck (giant V wave), abdominal pain due to the enlarged congested liver (due to CHF), and ankle oedema due to right heart failure.
Q.114. A 40-year-old man collapsed at home and died. The GPs report says he suffered from T2DM and BMI=35. What is the most likely cause of death?
Correct Answer : A
Diabetes mellitus and obesity are risk factors for developing MI. In diabetics, MI pain is not felt if there occurs autonomic neuropathy. But if there are no autonomic neuropathy diabetics will feel the pain of MI.
Q.115. An 18-year-old man complains of fatigue and dyspnea. He has left parasternal heave and systolic thrill with a harsh pan-systolic murmur at left parasternal edge. What is the most probable diagnosis?
Correct Answer : C
A small ventricular septal defect may cause no problems, and many small VSDs close on their own.
Medium or larger VSDs may need surgical repair early in life to prevent complications. If not treated may cause symptoms like shortness of breath, a feeling of tiredness or weakness (especially during exercise), poor appetite, and trouble gaining weight. left parasternal heave and systolic thrill with a harsh pan-systolic murmur at the left parasternal edge are examination findings of moderate to severe ventricular septal defect.
Q.116. An MI patient who is already on aspirin no longer smokes and his cholesterol, ECG, echo and BP are normal. Choose the best option for him:
Correct Answer : D
Statin + ACEi.
Offer all people who have had an acute MI treatment with the following drugs: ACE (angiotensin-converting enzyme) inhibitor dual antiplatelet therapy (aspirin plus a second antiplatelet agent) beta-blocker statin.
Q.117. In 85% of the population this artery is dominant. What is the most appropriate option?
Correct Answer : D
If the posterior descending artery is supplied by the circumflex artery then it is left dominant and if the posterior descending artery is supplied by the right coronary artery then it is right dominant. As in 85% of population posterior descending the artery is supplied by the right coronary artery which is called the dominant that is right coronary artery is dominant.
Q.118. A 60-year-old patient who has had a MI a week back presents with dyspnea and pericardial rub. ECG shows ST elevation. CXR: loss of margin at costo-vertebral angle. What is the most likely cause?
Correct Answer : C
Dressler syndrome is a secondary form of pericarditis that occurs in the setting of injury to the heart or the pericardium such as heart attack (myocardial infarction), heart surgery, heart procedure, or chest trauma due to an accident or injury. It is also known as post-myocardial infarction syndrome, post-cardiac injury syndrome, or post-pericardiotomy syndrome.
Dressler’s syndrome is characterized by combinations of pericarditis, pleuritis, and pneumonitis.
This pleuritis is responsible for pleural effusion leading to loss of margin at the costo-vertebral angle. The disease consists of a persistent low-grade fever, chest pain (usually pleuritic), pericarditis (usually evidenced by a pericardial friction rub, chest pain worsening when recumbent, and diffuse ST elevation with PR segment depression), and/or a pericardial effusion.
The symptoms tend to occur 2–3 weeks after myocardial infarction but can also be delayed a few months. It tends to subside in a few days, and very rarely leads to pericardial tamponade.
Q.119. A-57-year old woman who is suffering from hypertension, presented to the hospital with complaints of recurrent falls when trying to get out of bed or getting up from sitting. She is on some anti-hypertensive therapy with no other medical problems. What is the cause of her fall?
Correct Answer : C
It causes postural hypotension by volume depletion.
Q.120. A 47-year-old man with history of IHD complains of chest pain with SOB on exertion over the past few days. ECG normal, Echo reveals decreased EF (ejection fraction) and decreased septal wall thickness. What is the most likely diagnosis?
Correct Answer : A
Dilated cardiomyopathy (DCM) is a condition in which the heart becomes enlarged and cannot pump blood effectively. Symptoms vary from none to feeling tired, leg swelling, and shortness of breath. It may also result in chest pain or fainting.
Causes include genetics, alcohol, cocaine, certain toxins, complications of pregnancy, and certain infections. Coronary artery disease and high blood pressure may play a role, but are not the primary cause.
Q.121. A 66-year-old man has the following ECG. What is the most appropriate next step in management?
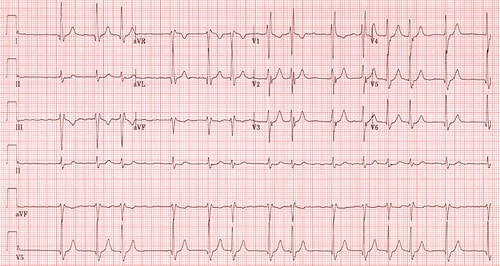
Correct Answer : A
Metoprolol.
P waves are replaced by fibrillatory f-waves. Irregular R-Rintervals. The diagnosis is atrial fibrillation.
Q.122. ECG of an 80-year-old patient shows saw-tooth like waves, QRS complex of 80ms duration,ventricular rate=150/min and regular R-R interval. What is the most probable diagnosis?

Correct Answer : B
Atrial flutter.
Saw-tooth-like waves, normal QRS complex of 80 ms (normal range 70-100 ms), ventricular rate of 150/min, and regular R-R intervals are diagnostic of atrial flutter.
Q.123. A 54-year-old patient 7 days after a total hip replacement presents with acute onset breathlessness and raised JVP. Which of the following investigation will be most helpful in leading to a diagnosis?
Correct Answer : B
The patient has a +ve two-level PE.
Wells score (if it was negative we should do D-Dimer) and there is no renal impairment or history suggestive of allergy to contrast media (if these were present we should have gone for VQ scan) the investigation of choice is PTCA.
Q.124. A 61-year-old man has been referred to the OPD with frequent episodes of breathlessness and chest pain along with palpitations. He has a regular pulse rate 60bpm. ECG sinus rhythm. What is the most appropriate investigation to be done?
Correct Answer : D
24h ECG.
Episodic breathlessness, chest pain, and palpitations are suggestive of paroxysmal arrhythmia. As paroxysmal arrhythmia it will only be evident during the attack and in between attacks ECG will be normal (as in the given case). So to confirm the diagnosis 24h ECG should be done.
Indications of 24 h ambulatory heart monitoring:
1. To evaluate chest pain not reproduced with exercise testing
2. To evaluate other signs and symptoms that may be heart-related, such as fatigue, shortness of breath, dizziness, or fainting
3. To identify arrhythmias or palpitations
4. To assess risk for future heart-related events in certain conditions, such as idiopathic hypertrophic cardiomyopathy, post-heart attack with weakness of the left side of the heart, or Wolff-Parkinson-White syndrome
5. To assess the function of an implanted pacemaker
6. To determine the effectiveness of therapy for complex arrhythmias.
Q.125. A woman had an MI. She was breathless and is put on oxygen mask and GTN, her chest pain has improved. Her HR 40bpm. ECG shows ST elevation in leads I, II, III. What is your next step?
Correct Answer : C
If no time limit is mentioned it is assumed that the patient has reached within the time required for primary PCI. There is general agreement that PCI should be considered if there is an ST-elevation. ACS if symptoms started up to 12 hours previously.
Q.126. A 45-year-old man who is diabetic and hypertensive but poorly compliant has chronic SOB (Shortness Of Breath), develops severe SOB and chest pain. Pain is sharp, increased by breathing and relieved by sitting forward. What is the most appropriate diagnosis?
Correct Answer : B
Nature of pain i.e. sharp pain increased by breathing and relieved by sitting forward is suggestive of pericarditis.
Nature of pericardial pain: the most common symptom is sharp, stabbing chest pain behind the sternum or in the left side of your chest. However, some people with acute pericarditis describe their chest pain as dull, achy, or pressure-like instead, and of varying intensity.
The pain of acute pericarditis may radiate to your left shoulder and neck. It often intensifies when you cough, lie down, or inhale deeply. Sitting up and leaning forward can often ease the pain.
Q.127. A 50-year-old lady presents to emergency department with sudden severe chest pain radiating to both shoulder and accompanying SOB (shortness of breath). Examination: cold peripheries and paraparesis. What is the most appropriate diagnosis?
Correct Answer : B
Cold peripheries due to reduced blood flow to distal parts of dissection. Paraperesis or paraplegia due to spinal cord ischemia and infarction as a presenting manifestation of aortic dissection has been found in 2 to 5 % of patients.
Usual management for type A dissection is surgery and for type B is conservative.
Q.128. A 28-year-old man presents with rapid pounding in the chest. He is completely conscious throughout. The following ECG was taken. What is the 1st medicine to be used to manage this condition?
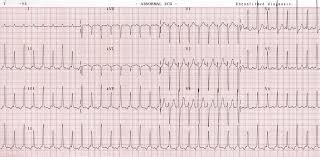
Correct Answer : B
Management of SVT:
i) Vagal manoeuvres (carotid sinus message, Valsalva manoeuvre) transiently increase AV-block, and unmask the underlying atrial rhythm. If unsuccessful then the first medicine used in SVT is adenosine, which causes transient AV block and works by : Transiently slowing ventricles to show the underlying atrial rhythm.
ii) Cardioverting a junctional tachycardia to sinus rhythm.
Q.129. A 72-year-old man is found to be not breathing in the CCU with the following rhythm. What is the most likely diagnosis?

Correct Answer : C
Ventricular fibrillation is when the heart quivers instead of pumping due to disorganized electrical activity in the ventricles.
Diagnosis is by an electrocardiogram (ECG) showing irregular unformed QRS complexes without any clear P waves.
Q.130. A 65-year-old male presents with dyspnea and palpitations. Examination: pulse 170 bpm, BP 120/80 mmHg. Carotid massage has been done as first instance. What is the next step of the management?
Correct Answer : A
The likely diagnosis is SVT. 1st vagal maneuvers (carotid sinus massage, Valsalva manoeuvre), if fails then next is to give iv adenosine.
Q.131. A 55-year-old woman was found collapsed at home, paramedics revived her but in the ambulance she had a cardiac arrest and couldn’t be saved. The paramedic’s report tells that the woman was immobile lately due to hip pain and that they found ulcers on the medial side of ankle. She had DM and was on anti-diabetics. What is the cause of her death?
Correct Answer : C
Pulmonary embolism.
Immobilization due to hip pain may result in DVT and later pulmonary embolism.
Q.132. A 58-year-old type 1 diabetic on anti hypertensive therapy for 13 years developed central chest pain for 45 minutes while driving along with cold sweating and dyspnea. What is the most appropriate diagnosis?
Correct Answer : A
The given picture of central chest pain for 45 minutes (more than 30 minutes), sweating, and dyspnoea with major risk factors of DM and HTN suggest the diagnosis of MI.
In pericarditis pain is aggravated by inspiration or lying flat and relieved by leaning forward.
A pericardial rub may present and there may be fever. In pneumothorax pain is not central but pleuritic. Pulmonary embolism causes dyspnoea and pleuritic chest pain. In costochondritis, localized pain / tenderness at the costochondral junction is enhanced by motion, coughing, or sneezing.
Q.133. A 45-year-old manual worker presented with a 2 hour history of chest pain radiating to his left arm. His ECG is normal. What is the most appropriate investigation?
Correct Answer : A
Probable diagnosis is MI. In MI often ECG doesn’t show the changes in the early stage. Cardiac enzymes will help in such cases.
Q.134. A 50-year-old man with DM suddenly develops persistent crushing central chest pain radiating to the neck. What is the most appropriate diagnosis?
Correct Answer : D
The features described are insufficient and can be seen in both aortic dissection and MI. However, dissection pain is described as tearing and crushing pain and is often used for MI pain. Both dissection and MI can cause pain radiation to the neck.
The history of diabetes goes with MI as it is a recognized risk factor for MI. Some may argue that DM MI will be painless! But it is not always the case. MI is only painless when autonomic neuropathy becomes well established.
Q.135. A 50-year-old woman returned by air from Australia. 3 days later she presented with sharp chest pain and breathlessness. Her CXR and ECG are normal. What is the most appropriate investigation?
Correct Answer : C
Wells score is >4. So single most appropriate investigation is CTPA.
Q.136. A 48-year-old presents with severe chest pain since the last 40 mins. In the emergency department he is given oxygen, GTN, morphine. ECG shows ST elevation. Bloods increased troponin levels. What is the next step of management?
Correct Answer : D
In any case of IHD, the most important initial management is aspirin (unless decided to go for thrombolysis). Aspirin, the most widely used anti-platelet agent, is effective, safe, and inexpensive and is recommended for all patients undergoing PCI.
Patients already on daily aspirin therapy should be given 75–325 mg of aspirin before PCI; those not taking aspirin should be given 500 mg at least 3 hours before the procedure or 300 mg intravenously immediately before the procedure. After PCI, aspirin should be continued at 75–160 mg/day indefinitely.
Q.137. A 65-year-old man with hypertension develops gingival hyperplasia. What is the most likely cause?
Correct Answer : C
Gingival hyperplasia is a recognized side effect of calcium channel blockers.
Q.138. A 65-year-old woman is undergoing coronary angiography. What measure will protect her kidneys from contrast?
Correct Answer : D
Contrast media that are pushed in blood are nephrotoxic and IV normal saline will help to maintain adequate hydration to pass it out with urine.
Q.139. A 53-year-old had a dental extraction after which he recently had a mitral valve prolapse, high temp of 39C, cardiac failure and new cardiac murmur. What is the most likely diagnosis?
Correct Answer : D
Infective endocarditis (IE) is defined as an infection of the endocardial surface of the heart which may include one or more heart valves, the mural endocardium, or a septal defect. Its intracardiac effects include severe valvular insufficiency, which may lead to intractable congestive heart failure and myocardial abscesses. If left untreated, IE is almost inevitably fatal. Dental extraction is a risk factor for infective endocarditis.
Q.140. A 46-year-old African-Caribbean man is found to have BP 160/90mmHg on 3 separate occasions. What is the best initial treatment?
Correct Answer : B
If age less than 55 years In general ACEI or Beta blockers are preferred. But in the case of Afro-Caribbean origin, CCB is chosen even in younger age as it gives better results in this ethnic group.
Q.141. A 45-year-old man had recently started taking anti-hypertensive therapy. 6 months later his RBS is 14mmol/l. Which drug is most likely to have caused this?
Correct Answer : B
High blood sugar is a well-known side effect of thiazide (here bendroflumethiazide).
Q.142. A 43-year-old lady is admitted with pyrexia, arthropathy, breathlessness and syncope. She was recently diagnosed with pulmonary emboli. There is an early diastolic sound and a mid-diastolic rumble. Her JVP is elevated with prominent a-waves. What is the most likely cause?
Correct Answer : C
Atrial myxomas are the most common primary heart tumors. Two-dimensional echocardiography is the diagnostic procedure of choice. Most atrial myxomas are benign and can be removed by surgical resection. Constitutional symptoms that include fever, weight loss, arthralgias, and the Raynaud phenomenon. These symptoms may be related to the overproduction of interleukin-6. Left heart failure may cause dyspnea on exertion caused by obstruction at the mitral valve orifice.
Valve damage may result in mitral regurgitation. Jugular venous pressure may be elevated, and a prominent A wave may be present. An early diastolic sound called a tumor plop, is heard.
A diastolic atrial rumble may be heard if the tumor is obstructing the mitral or tricuspid valve. Systemic or pulmonary embolization may occur from left- or right-sided tumors. Embolization to the central nervous system may result in transient ischemic attack, stroke, or seizure.
Q.143. A 60-year-old lady has severe chest pain. ECG shows changes of inferior wall MI. ECG also shows progressive prolongation of PR interval until a QRS complex is dropped. What is the most probable diagnosis?
Correct Answer : C
Mobitz type I 2nd-degree heart block.
Inferior MI is frequently associated with conduction defect.
Q.144. A 56-year-old man was recently put on anti-hypertensive medications and recent biochemistry on 2 occasions showed: Na+ 132, K+ 7.6, Urea 11.3, Creatinine 112. Which of the following drugs is responsible for this result?
Correct Answer : D
ACEI and ARB are known to raise the serum potassium level.
Q.145. A 63-year-old man continues to experience chest pain and has a temperature of 37.8C 2 days after an acute MI. His ECG shows widespread ST elevation with upward concavity. What is the most likely explanation for the abnormal investigation?
Correct Answer : A
Chest pain, raised temperature and ECG findings of widespread ST elevation with upwards concavity are diagnostic of acute pericarditis, particularly after MI.
Q.146. A 55-year-old man returns for routine follow up 6 weeks after an MI. He gets breathless when walking uphill. His ECG shows ST elevation in leads V1, V2, V3 and V4. What is the most likely explanation for the abnormal investigation?
Correct Answer : D
Left ventricular aneurysm is defined as a localized area of the myocardium with abnormal outward bulging and deformation during systole and diastole. Clinically, ventricular aneurysms may be recognized late with features of heart failure and persistent ST elevation, recurrent ventricular arrhythmias, or recurrent embolization.
Risk factors for these aneurysms after acute MI include the following: Female sex, Total occlusion of the left anterior descending (LAD) coronary artery, Single-vessel coronary artery disease (CAD), Absence of previous angina pectoris.
Q.147. A 76-year-old man suddenly collapsed and died. At post mortem exam, a retroperitoneal hematoma due to ruptured aortic aneurysm was noted. What is the most likely underlying cause of the aortic aneurysm?
Correct Answer : A
Any condition that causes the walls of the arteries to weaken can lead to an aneurysm. Atherosclerosis is the leading cause. Others are high blood pressure and smoking. Deep wounds, injuries, or infections can also cause blood vessels to bulge.
Q.148. A 33-year-old male came to the hospital with complaint of occasional left sided chest pain that lasts <30 minutes, following exercise, which relieves upon taking rest. What is the most probable diagnosis?
Correct Answer : C
Stable angina is chest pain or discomfort that most often occurs with activity or emotional stress and lasts for <30 minutes, relieved by rest or nitroglycerine. Symptoms of angina occur when the blood supply to the heart muscle is reduced. This happens when the coronary arteries are narrowed or blocked by atherosclerosis or by a blood clot.
Q.149. An 82-year-old male suddenly becomes unconscious and fell down. He recovered completely within minutes. What is the best investigation you do to diagnose the case?
Correct Answer : A
Here sudden unconsciousness without any provocation makes arrhythmia the most likely cause; hence we should do an ECG.
Q.150. A 56-year-old man presents to the emergency department with chest pain. The following ECG was taken. What is the most likely diagnosis?
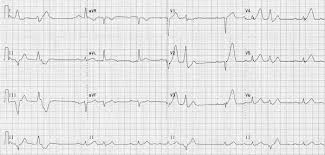
Correct Answer : A
Here ST elevation in L1, aVL, v2,v3,v4 and v5. So the diagnosis is anterior MI (as L1 and aVL and v2-v5, anterolateral would be more appropriate description).
Q.151. A man comes to the emergency department with history of pulsatile swelling in the abdomen, he has history of hypertension and on examination: pulse 120 bpm, BP 70/40 mmHg. He is restless and in shock. What emergency management should be done on priority basis?
Correct Answer : C
IV fluids 0.9%. NS crystalloids to bring SBP to 90 mmHg.
Probable ruptured aortic aneurism. Immediate IV normal saline to raise the BP to 90 mmHg to keep the vital organs perfused till definitive measures are taken.
Q.152. A 72-year-old man presents to the ED (emergency department) with chest pain. The following ECG was taken. What is the most likely diagnosis?
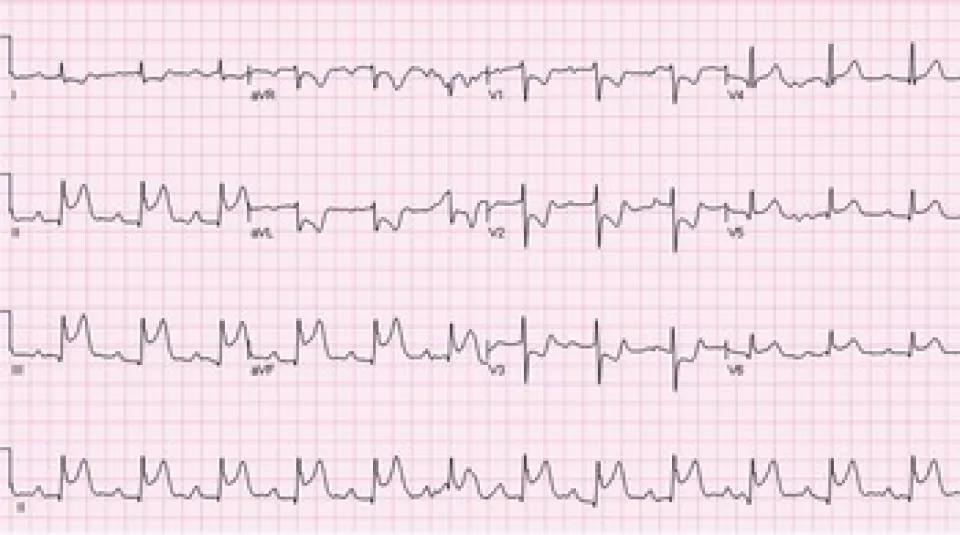
Correct Answer : B
There is ST elevation in leads II, III and aVF and pathological Q wave in lead III.
Q.153. A patient underwent hip surgery. Later he presents with SOB (shortness of breath) and chest pain. What is the diagnosis?
Correct Answer : A
History of surgery (particularly when patients are immobile like hip surgery) followed by chest pain and breathlessness strongly suggests diagnosis of pulmonary embolism.
Q.154. A 25-year-old man presents with history of breathlessness. A transthoracic echo reveals a patent foramen ovale. What diagnostic investigation would you do for a patent foramen ovale?
Correct Answer : B
This is a test that can help identify a Patent Foramen Ovale. Pictures are taken of the heart in the same way a normal echocardiogram is performed. A small thin plastic cannula will be inserted into a vein in the patient’s arm.
A small amount of sterile salty water (saline) will be mixed with a small amount of the patient’s blood and then injected into the vein in the patient’s arm. The salty water contains tiny harmless bubbles which can be tracked on the echocardiogram scan revealing any potential abnormal flow through patent foramen ovale.
Q.155. The body of a 65-year-old man who was treated for TB and bronchitis was seen at autopsy. His legs were swollen and his liver showed signs of a transudate fluid. What was the cause of the transudate?
Correct Answer : C
Chronic bronchitis is a well-known cause of congestive cardiac failure. Leg oedema and transudative fluid in the liver are suggestive of congestive cardiac failure.
Q.156. A woman presents with history of falls, becomes pale and clumsy. She is hypertensive and takes atenolol, bendroflumethiazide and amlodipine. What investigation is needed?
Correct Answer : B
All these drugs (particularly prolonged use of thiazide and amlodipine) are well-established causes of postural hypotension. So 24-hour BP monitoring should be done.
Q.157. A 52-year-old man with history of anterior MI 3 weeks ago developed sudden onset of dyspnea. Examination: BP 100/60 mmHg, pulse 100 bpm, SaO2 88%, chest bilateral crackles. Which investigation would you do to find the underlying cause?
Correct Answer : B
Sudden papillary muscle rupture or VSD may be the likely cause (ventricular aneurism may take a slower course), so echo is a more logical approach.
Q.158. A 74-year-old lady called an ambulance for an acute chest pain. She has a history of diabetes mellitus and hypertension, and is a heavy smoker. Paramedics mentioned that she was overweight and recently immobile because of a hip pain. She collapsed and died in the ambulance. What is the most likely cause of death?
Correct Answer : A
Clue - h/o immobilisation.
Q.159. A 78-year-old gentleman suddenly collapsed. His heart rate 120 bpm, BP 70/40 mmHg. Examination: pulsatile mass in abdomen. What is the most appropriate diagnosis?
Correct Answer : A
There are features of shock with a pulse of 120 bpm and BP 70/40 mmHg and the sudden collapse of the patient with a pulsatile mass in the abdomen makes the likely diagnosis of ruptured aortic aneurysm.
Q.160. A 48-year-old man has continuous anterior chest pain which is worse on inspiration and has temperature of 37.5C since 4 weeks after a MI. His ESR is 45 mm/h. What is the most likely explanation for the abnormal investigation?
Correct Answer : D
Dressler’s syndrome is a form of pericarditis or inflammation of the pericardium. Dressler’s syndrome can occur after a heart attack (myocardial infarction), heart surgery, heart procedure, or chest trauma due to an accident or injury.
It is also known as post-myocardial infarction syndrome, post-cardiac injury syndrome, or postpericardiotomy syndrome. Dressler’s syndrome usually occurs within two to six weeks after heart surgery or a heart attack, but it can take up to several months for symptoms to develop. It is characterized by pleuritic chest pain which is worse on inspiration, low-grade fever, and pericarditis.
Q.161. A patient diagnosed with DVT is taking warfarin. What is his cut off INR limit?
Correct Answer : C
This range is appropriate for the prophylaxis or treatment of venous thromboembolism and reduction of the risk of systemic embolism for people with atrial fibrillation and valvular heart disease.
Q.162. A 70-year-old woman with longstanding anxiety is seen in the OPD. She complains of her heart skipping a beat quite often. This particularly occurs when she is trying to get to sleep. The palpitations are never sustained. What is the most likely rhythm disturbance?
Correct Answer : D
An ectopic rhythm is an irregular heart rhythm due to a premature heartbeat. Ventricular ectopic rhythm is also known as premature ventricular contraction and ventricular extrasystole. When a patient's heart experiences an early beat, a brief pause usually follows. Ventricular-ectopics If occurs in a normal heart though symptomatic it is benign but if it is secondary to heart disease like MI it may precipitate to more life-threatening arrhythmia like ventricular fibrillation.
Q.163. A 29-year-old man was involved in an RTA (road traffic accident). He presents with distended neck veins, clear breath sounds and a trachea which is in the midline. His RR (respiratory rate) 34 bpm, BP 60/0 mmHg. What is the most likely diagnosis?
Correct Answer : C
Cardiac tamponade is a clinical syndrome caused by the accumulation of fluid in the pericardial space, resulting in reduced ventricular filling and subsequent hemodynamic compromise. The condition is a medical emergency, the complications of which include pulmonary edema, shock, and death. Distended neck vein, clear breath sound, no tracheal shift, and BP of 60/0 points towards cardiac tamponade.
Q.164. A 50-year-old man presented with increased breathlessness at rest. He is currently on furosemide, digoxin and isosorbide mononitrate. What drug is going to help him?
Correct Answer : B
This is a case of diuretic resistance. Heart failure represents the most common clinical situation in which diuretic resistance is observed. In mild CHF, diuretic resistance is not commonly encountered, as long as renal function is preserved. However, in moderate and severe CHF patients, diuretic resistance occurs more frequently and often becomes a clinical problem. In diuretic resistance, another diuretic is added to get optimal or desirable results.
As the patient is still in heart failure and pulmonary edema with the usage of a loop diuretic (frusemide), a thiazide diuretic could be added with frusemide when the response is inadequate. This will reduce the volume overload and improve breathing.
Q.165. A 52-year-old man underwent a hemicolectomy. After a few days he complains of left ventricular pain and fever. ECHO has been done and shows a systolic murmur. What is the next appropriate investigation?
Correct Answer : D
History of surgery, left ventricular pain, fever, and murmur suggest a diagnosis is infective endocarditis. Therefore the next appropriate investigation is blood culture.
Q.166. A 63-year-old man has been brought to the hospital after collapsing during a wedding. His ECG is below. What is the most likely diagnosis?
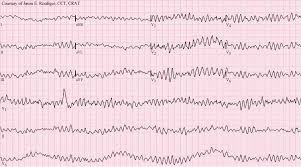
Correct Answer : C
QRS complex is chaotic, wide, bizarre, and irregular which is characteristic of ventricular fibrillation.
Q.167. A 56-year-old man who is hypertensive recently underwent a change in medicines. 2 days later he developed wheezing. Which drug can cause this?
Correct Answer : A
Beta blockers can precipitate asthma attacks even though cardioselective.
Q.168. A hypertensive patient on bendroflumethiazide 2.5mg/d has come for his routine checkup. Examination: BP 145/85mmHg. Lab investigation: K+ 5.9, Na+ 137. What is the most appropriate management for this patient?
Correct Answer : D
Bendroflumethiazide causes hyponatremia and hypokalemia. But the findings are the opposite which is probably the error of the test. Hence blood tests should be repeated to confirm the level of potassium and sodium.
Q.169. A 57-year-old man having hypertension is on oral anti-hypertensive. However, he is finding it difficult to mobilize as he feels dizzy whenever he tries to get up. What is the most appropriate investigation for him?
Correct Answer : A
Ambulatory BP to document low BP as the cause of presenting symptoms. The case seems to be of postural hypotension and low BP as a result of the given antihypertensive.
Q.170. After surgery a patient’s left leg has become swollen and tender. The diameter of the calf has increased and passive movements cause pain. What is the most probable diagnosis?
Correct Answer : A
Swelling, tenderness, and enlarged calf diameter are features of DVT supported by positive Homan’s test (pain on passive movement).
Q.171. A 50-year-old female had swelling in her ankles. She is a known alcoholic. Now she presented with breathlessness and palpitations. What is the most likely cause of her condition?
Correct Answer : D
Ankle swelling suggests alcoholic cardiomyopathy and alcoholism is also a well-known cause of atrial fibrillation.
Q.172. A 42-year-old lady had corrective surgery for cyanotic congenital heart disease at the age of 3y, after a palliative operation during infancy. There is a parasternal impulse and an early diastolic murmur. What is the most probable diagnosis?
Correct Answer : D
In the present day, some patients with tetralogy of Fallot have survived for longer than 15-20 years after their first operation. The major problem encountered by these individuals is the development of pulmonary valvular regurgitation. It appears that a number of these individuals require pulmonary valve replacement.
Q.173. What is the most likely diagnosis based on this ECG?
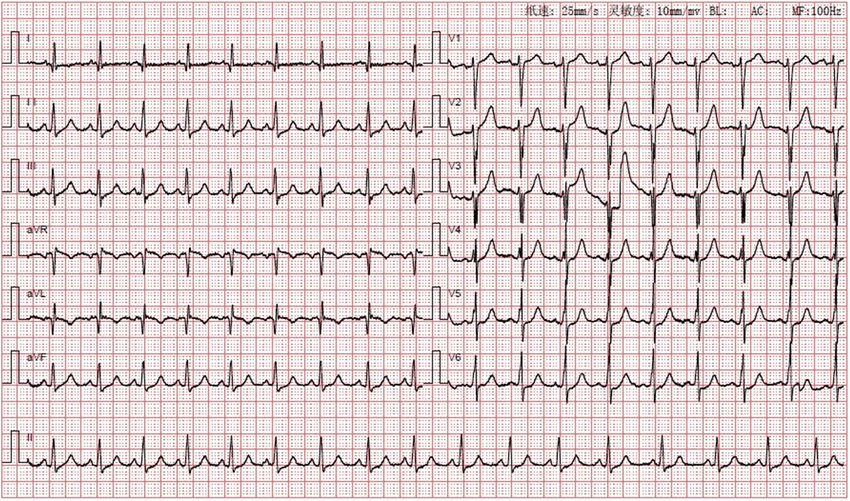
Correct Answer : C
Sinus Tachycardia
Q.174. Patient with pain and swelling in left leg and thigh up to the level of inguinal ligament. Where is the level of occlusion?
Correct Answer : B
The general rule is occlusion occurs in proximal bifurcation.
Left common iliac artery. That is an occlusion in the bifurcation of the left common iliac artery (as the femoral artery bifurcates more distally to superficial and deep branches).
Q.175. A 65-year-old man presents with dyspnea 3 days after an MI. On auscultation he has a pansystolic murmur at the apex radiating to the axilla. What is the most likely diagnosis?
Correct Answer : A
Pansystolic murmur in apex radiating to the axilla may be due to mitral regurgitation secondary to papillary muscle rupture.
Q.176. A 63-year-old man presented with sudden onset of severe dyspnea, orthopnea, raised JVP and bilateral basal crackles 3 days after an episode of MI. A diagnosis of acute congestive cardiac failure was made and IV furosemide was started for this patient. What electrolyte abnormality is expected?
Correct Answer : C
Low Na+, Low K+.
Frusemide causes hyponatremia, hypochloremic alkalosis, hypokalemia, hypomagnesemia and hypocalcemia.
Q.177. A 7-year-old hypertensive white british man on thiazide diuretics needs a 2nd drug to control his BP. Which one of the following is the best choice for him?
Correct Answer : B
In patients >55 yrs - CCB.
If CCB is not suitable (oedema, heart failure) thiazide is preferred.
In patients <55yrs - ACEI or ARB.
Now if the patient is on CCB or Thiazide and 2nd drug is to be added it should be one of ACEI or ARB and not one from CCB or Thiazide.
Q.178. A 62-year-old man has slow palpitations and the following ECG. What is the most likely diagnosis?
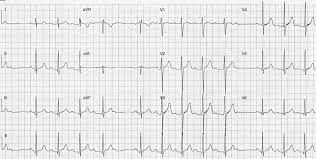
Correct Answer : C
Mobitz type 1 block.
Gradual prolongation of PR interval followed by a drop beat.
Q.179. A 70-year-old woman is admitted with diarrhea, vomiting and dehydration. Examimation: yellow visual halos in her eyes, ECG bradycardia. She has a history of chronic atrial fibrillation. Which drug causes the above mentioned side effects?
Correct Answer : D
Digoxin toxicity causes diarrhea, vomiting, dehydration, xanthopsia (yellow halos around light), bradycardia. History of atrial fibrillation is also a clue of digoxin use.
Q.180. A white English man with a past history of MI is a known hypertensive and diabetic. He is currently on aspirin, statin and metformin. What would you add to the treatment?
Correct Answer : A
The patient is diabetic and has a pass history of MI. In both of these situations ACEI is the antihypertensive of choice.
Q.181. A 51-year-old man had an MI a few days ago. He developed breathlessness. Echo was done and showed a pansystolic murmur. What can be the cause of this symptom?
Correct Answer : A
Papillary muscle rupture causes mitral regurgitation causing pancystolic murmur leading to features of heart failure like breathlessness.
Q.182. A 72-year-old man presents to the emergency department with chest pain. The following ECG was taken. What is the most likely diagnosis?

Correct Answer : D
Ans. The key is D. NSTEMI
Q.183. A 65-year-old lady who is on thiazide suffers from falls in the morning. What is the cause for her symptoms?
Correct Answer : A
Orthostatic hypotensin.
Thiazide diuretic is associated with orthostatic hypotension due to fluid depletion.
Q.184. A 28-year-old man presents with a 2 hours history of rapid palpitations. He feels a little light headed but is otherwise well. Examination: pulse 170 bpm and regular, BP 100/68 mmHg. He has had 2 similar episodes in the past. What is the most likely rhythm disturbance?
Correct Answer : A
Palpitation, lightheadedness with a tachycardia of 170bpm that is regular are most likely SVT. Ventricular tachycardia is usually seen in patients with cardiac disease like ischemic heart disease and may frequently lead to hemodynamic instability.
Q.185. A 45-year-old man is admitted to emergency department with excruciating pain in the right leg. Examination: limb is pale and dorsalis pedis and posterior tibial pulses are absent. Pulse=88bpm, irregular and he has a pansystolic murmur at apex. What is the most probable diagnosis?
Correct Answer : D
Pansystolic murmur at apex indicates mitral regurgitation and irregular pulse indicates AF which can lead to thrombus formation which probably is responsible for this embolus in the leg.
Q.186. A 58-year-old man suddenly becomes shocked several days after suffering an acute anterior MI. His CXR shows a large globular-shaped heart and clear lung fields. What is the most likely explanation for the abnormal investigation?
Correct Answer : B
Cardiac tamponade.
Shock in a post-MI patient with a globular heart on X-ray and clear lung field indicate Cardiac tamponade.
Q.187. A branch of the dominant coronary artery that supplies the inferior portion of the septum. What is the most appropriate option?
Correct Answer : D
Left main stem, posterior descending artery.
Here no option is satisfactorily correct! By dominant coronary artery, we mean the coronary artery which gives the branch of the posterior descending artery.
Mostly it is the right coronary artery and if there is left coronary dominance, the posterior descending artery is the branch of the circumflex artery and not the direct branch of the left main artery.
However, the only option that goes nearer is D. Left main stem, post. descending artery.
Q.188. The artery that supplies the anterior right ventricular wall. What is the most appropriate option?
Correct Answer : A
Acute marginal branch
Q.189. After an MI, a man presents with pansystolic murmur which is radiating to the axilla. What is the diagnosis?
Correct Answer : B
MI can lead to papillary muscle rupture causing mitral regurgitation.
Q.190. A 59-year-old patient has been diagnosed with hypertension. His BP has been >160/90mmHg on 3 separate occasions. His biochemical profile is as follows: Na+ 145mmol/l, K+ 6.2mmol/l, creatinine 112umol/l, urea 5.7mmol/l. What is the most appropriate anti-hypertensive drug for him?
Correct Answer : B
Thiazide reduces Na+ and K+ level. So in this picture of upper normal Na+ with hyperkalemia thiazide seems to be appropriate.
Q.191. A 46-year-old man with tachycardia has the following ECG. What is the most likely diagnosis?
Correct Answer : D
WPW syndrome.
Short PR interval and slurred delta wave indicates WPW syndrome.
Q.192. A 55-year-old patient presents with collapse and complains of abdominal pain that radiates to the back. An expansile abdominal mass is felt on examination and the patient is in shock. What is the most likely diagnosis?
Correct Answer : A
Ruptured aortic aneurysm.
Q.193. A new born baby is borught with pansystolic murmur at sternal border but the baby is not cyanosed. What is the diagnosis?
Correct Answer : A
Pancystolic murmur in sternal border without cyanosis is indicative of VSD.
Q.194. A 55-year-old man is having slow growing ascites. When we tap the peritoneal fluid the protein is <25 and it is clear and yellow. What could be the origin for ascites?
Correct Answer : A
In gastrinoma there is no ascites! In hepatoma, there will be exudative ascites as in TB and pancreatitis. Budd-Chiary syndrome causes transudative ascites and the likely option here.
Q.195. A 50-year-old man came to the hospital a few months after he had a MI. Examination: everything normal, S1 and S2 were heard on auscultation, but there is a new pan-sytolic murmur. What is the most appropriate investigation of choice?
Correct Answer : C
To rule out any valvular lesion (following papillary muscle rupture) or septal lesion.
Q.196. A man after MI presented with sudden breathlessness and dyspnea. Examination: scattered pansystolic murmur all over the precordium. What is the next investigation that will lead to diagnosis?
Correct Answer : B
Sudden breathlessness and dyspnea suggest mitral regurgitation secondary to papillary muscle rupture. D/D is VSD. However, in either case, the required investigation is echo.
Q.197. A man is brought to the emergency department after he was stabbed in the chest. Chest is clear bilaterally with muffled heart sounds. BP- 60/40mmHg, pulse 120bpm, JVP is raised. What is the most probable diagnosis?
Correct Answer : B
Lungs clear bilaterally excludes effusion and pneumothorax.
Muffled heart sounds and low bp with raised jvp point towards the diagnosis of cardiac tamponade.
These three signs together are known as Beck’s triad.
Q.198. A 68-year-old man on treatment for an irregular heart beat comes to the emergency depatment. He has palpitations for the last 3 hours. Examination: pulse regular, 154 bpm. Carotid sinus massage settled his pulse down to 80 bpm. What is the most likely rhythm disturbance?
Correct Answer : A
Regular tachycardia responding to vagal maneuver is SVT.
Q.199. A 76-year-old man is in the CCU 2 days after an acute MI. He tells you that he had an episode of rapid pounding in the chest lasting for about 2minutes. He remains conscious throughout. What is the most likely rhythm?
Correct Answer : D
VT is a common arrhythmia post MI. Sustained ventricular tachycardia (VT) is defined as a fast heart rhythm originating in the ventricles that lasts for 30 seconds or longer, or is terminated due to hemodynamic compromise before that time. Non-sustained VT (NSVT) is a similar rapid rhythm but lasts less than 30 seconds and doesn't cause hemodynamic instability and patient remains conscious throughout, as is the case here.
Q.200. A 70-year-old lady on Raloxifene for osteoporosis has recently to the Gulf from Australia. She now presents with severe chest pain, SOB and suddenly collapsed in the emergency department. What is the most appropriate diagnosis?
Correct Answer : C
Prolonged air travel is a risk factor for pulmonary embolism.
Q.201. A 54-year-old man comes with sudden onset of palpitations and breathlessness. His heart rate is 164 bpm. What is the most appropriate treatment in the acute phase?
Correct Answer : B
The arrhythmia where we use acute and chronic phases is AF. This is an acute phase of atrial fibrillation for which we use beta-blockers. So the answer should be B. Metoprolol here.
Q.202. A 72-year-old woman who is taking loop diuretics for left ventricular failure. She now is suffering from palpitations and muscle weakness. What is the electrolyte imbalance found?
Correct Answer : A
Na+=130mmol/L, K+=2.5mmol/L.
Loop diuretics causes hyponatremia and hypokalemia.
Q.203. A patient came to the hospital with a complaint of severe chest pain lasting for >1 hour. Following ECG test, patient revealed to have ST depression. He was already on aspirin. What is the most specific treatment for this patient?
Correct Answer : D
LMWH
Q.204. The ECG of a 65-year-old shows absent P waves, narrow QRS complex, ventricular rate of 120 bpm and irregular R-R interval. What is the most probable diagnosis?
Correct Answer : A
In Atrial fibrillation fibrillatory f waves replace p waves and R – R intervals are irregular.
Q.205. The ECG of an 80-year-old patient of IHD (ischemic heart disease) shows sawtooth like waves, QRS complex of 80 ms, ventricular rate of 150 bpm and regular R-R interval. What is the most probable diagnosis?
Correct Answer : B
Sawtooth like waves and regular R-R interval are diagnostic of atrial flutter.
Q.206. A 70-year-old man presents with a punched out ulcer between his toes. He is a heavy drinker and smoker. Examination: ulcer is yellow and the foot turns red when dangling off the bed. What is the most likely diagnosis?
Correct Answer : A
Arterial ischemia ulcer
Q.207. A 65-year-old woman complains of a painful discharging ulcer above her ankle on the inner side of her left lower leg. Examination: the base of the ulcer is red and covered by a yellow fibrous tissue. The border is irregular. The skin is tight. What is the most likely diagnosis?
Correct Answer : D
Some people with venous insufficiency develop stasis dermatitis. Blood pools in the veins of the lower leg. Fluid and blood cells leak out of the veins into the skin. It is usually seen above the ankle and the inner side of the leg.
Q.208. A 55-year-old woman suffered from an acute MI 5 days ago. While she was in the hospital the patient developed features of pulmonary edema and heart failure. What is the most probable cause of her present condition?
Correct Answer : B
Post MI rupture of papillary muscle is responsible for valve failure (mitral regurgitation) causing pulmonary oedema and heart failure.
Q.209. A 70-year-old man presents with acutely painful, pale paralysed and pulseless left leg. He is noted to have atrial fibrillation. What is the most probable diagnosis?
Correct Answer : D
AF may be the cause of thrombus leading to embolic acute limb ischemia.
Q.210. A 60-year-old man has had increasing pain in both buttocks, thighs and calves on walking for three months. He has also recently developed impotence. Femoral and distal pulses are absent in both limbs. What is the most likely site of arterial obstruction?
Correct Answer : A
Aorto iliac (saddle embolus; surgical intervention)
The patient is suffering from Leriche’s syndrome.
The classic triad of:
• Pain and claudication of buttock and thighs (pale cold leg)
• Erectile dysfunction from aorto iliac occlusive disease
• Absent femoral and distal pulse.
Q.211. A patient presents with irregularly irregular pulse of 162bpm. What drug is most useful initially?
Correct Answer : C
Most likely it's acute AF and 1st line is verapamil/bisoprolol, 2nd line digoxin/amiodarone.
Q.212. Which finding on clinical examination of the pulse, suggests a diagnosis of hypertrophic obstructive cardiomyopathy (HOCM)?
Correct Answer : D
Pulsusbisferiens, is a sign where, on palpation of the pulse, a double peak per cardiac cycle can be appreciated. Bisferious means striking twice.
Classically, it is detected when aortic insufficiency exists in association with aortic stenosis, but may also be found in hypertrophic obstructive cardiomyopathy.
Q.213. For the following type of surgery what is the most likely agent that may cause post-operative infection aorto-iliofemoral reconstruction with a Dacron vascular prosthesis?
Correct Answer : D
Staphylococcus epidermidis is most common cause of infections in prosthesis.
Q.214. Which one of the following electrocardiographic changes is found in hypercalcaemia?
Correct Answer : D
Short Q-T interval secondary to a shortened ST segment.
Q.215. A 58 year old man suddenly becomes shocked several days after suffering an acute myocardial infarction. His chest X-ray shows a large globular shaped heart and clear lung fields. What is the most likely diagnosis?
Correct Answer : C
Large globular heart indicates cardiac tamponade. Shock is due to compromised cardiac output due to tamponade.
Q.216. A 47-year-old man with a history of ischaemic heart disease complains of chest pain with shortness of breath on exertion over the past few days. ECG is normal and echocardiography shows decreased ejection fraction and decreased septal wall thickening. What is the most likely diagnosis?.
Correct Answer : A
Diagnosis is ischemic dilated cardiomyopathy.
Q.217. A 50-year-old man present with central crushing chest pain radiating to the left arm. ECG is shown below. What is the next step in management?
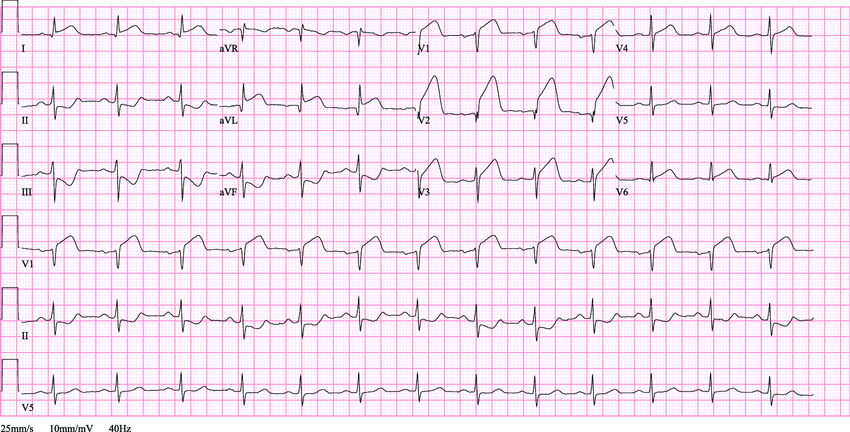
Correct Answer : C
Aspirin.
All patients with STEMI should receive an empiric loading dose of aspirin (325 mg) as early as possible and prior to reperfusion, regardless of the perfusion method. A lifelong maintenance dose of (75 mg) daily should be prescribed to all patients after STEMI.
Choose a Question
×Choose a Question
×
Trial Access Limit Reached
You’ve reached the limit of free content. Subscribe to continue learning without restrictions.