

Hello,
Dr. Batman
Hello Doctor, Welcome!
Profile

Name: Batman
Email: batman@gotham.com
ENDOCRINOLOGY
(Total Questions - 162)Q.1. A 38 year old male was rushed to Accident & Emergency after his wife found him unconscious on the floor of his home. Initial evaluation of the patient revealed severe dehydration, hypotension, tachycardia and a body temperature of 39°C. Blood tests done in A&E revealed hyponatraemia, hyperkalemia and hypoglycaemia. His wife mentions that he had been diagnosed with Addison’s disease a few years ago. Following resuscitation with normal saline, what is the other treatment that you should give this patient?
Correct Answer : B
This patient has an adrenal crisis. This is an emergency. Clues that point you toward this patient having an adrenal insufficiency is the mention of hyponatraemia, hyperkalemia upon blood testing. Addison’s disease describes a condition of primary adrenal insufficiency.
If a patient with known adrenal insufficiency presents with adrenal crisis, intravenous steroids need to be administered to rapidly decrease the inappropriate vasopressin production which therefore increases clearance of free water and corrects hyponatremia.
An adrenal crisis can be precipitated in patients with adrenal insufficiency by conditions such as an infection, trauma, or surgery.
The most common cause is usually a sudden withdrawal of chronic steroid therapy however in this scenario the reason for this patient’s adrenal crisis is probably an infection as evidenced by his high body temperature.
Treatment steps for patients with a suspected adrenal crisis:
1. Hydrocortisone IV
2. Normal saline infusion
3. Cardiac and electrolyte monitoring
4. Broad-spectrum antibiotics if infection is suspected as the precipitating cause.
5. Hydrocortisone in 5% glucose via IV infusion
6. Weaning off of IV steroids and commencing oral steroids.
From the above steps, we can determine that the next best step in the treatment of this patient is to administer hydrocortisone since a normal saline infusion has already been started. If you chose 5% glucose infusion, you are partially correct.
This patient has hypoglycaemia and should be given glucose. But this is the wrong step in management at this stage. This answer is therefore incorrect. Rarely, you would ever use 0.45% normal saline in clinical practice.
Generally, it is usually given in hypernatraemia along with dextrose and potassium. If this was given to this patient, this hypotonic saline would worsen the hyponatremia. Intravenous potassium would likely kill this patient.
Intravenous antibiotics are to be used to treat the underlying disorder (which is probably an infection in this case), but again the more important step here is intravenous hydrocortisone.
Q.2. A 21 year old man is brought into A&E semi-conscious by his friends. They were at a party and have been drinking alcohol when they found him unconscious in a corner. He is groaning and unable to give any information to the doctors. During the initial evaluation, his respiratory rate is 17/min and pulse rate is 88 bpm, BP is 110/70 mmHg, pupils are responsive. His Glasgow Coma Scale (GCS) score is 11/15. What is the most appropriate next course of action?
Correct Answer : D
Alcohol intoxication can cause hypoglycaemia which presentations include a coma. Checking venous or capillary blood with a glucose oxidase strip would be an appropriate first step before taking him for a CT scan or any other investigation.
It is fast and easy and if hypoglycaemia is the cause, it can be quickly reversible.
Always exclude hypoglycaemia in any patient with coma, altered behaviour, neurological symptoms, or signs.
Causes :
The commonest cause is a relative imbalance of administered versus required insulin or oral hypoglycaemic drug.
This results from Exercise Insufficient or delayed food intake. Excessive insulin administration.
Other causes are:
• Alcohol (in addition to alcohol directly causing hypoglycaemia, the features of hypoglycaemia may be mistaken for alcohol intoxication or withdrawal).
• Addison’s disease
• Insulinomas
• Liver failure
• Malaria
Common features : Plasma glucose is normally maintained at 3.6-5.8 mmol/L. Cognitive function deteriorates at levels < 3.0 mmol/L, but symptoms are uncommon > 2.5 mmol/L.
• Sweating
• Pallor
• Tachycardia
• Palpitations
• Hunger
• Trembling
• Altered or loss of consciousness
• Fitting
• Coma
Diagnosis :
• Venous or capillary blood with glucose oxidase strip (BMG)
• If < 3.0 mmol/L, take a venous sample for a formal blood glucose level, but do not delay treatment.
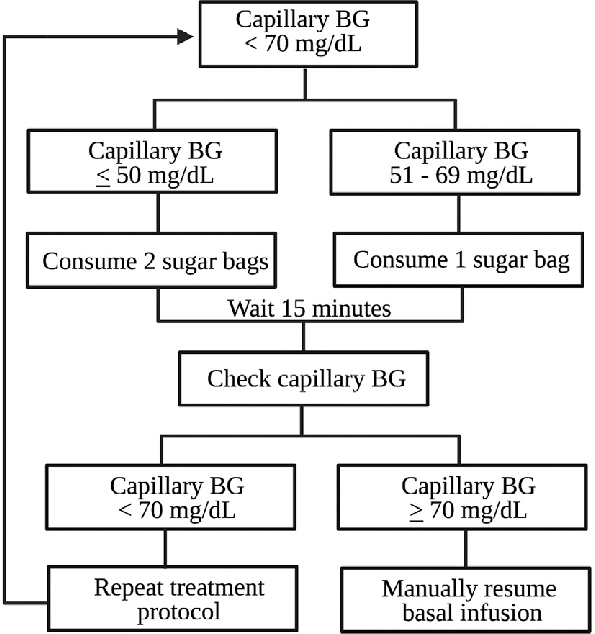
HYPOGLYCAEMIA : Hypoglycaemia in practical terms is regarded as blood glucose < 4 mmol/L however, cognitive function is only seen to deteriorate once glucose levels are less than 3.0 mmol/L.
Recognizing hypoglycaemia -
1. Assess the patient clinically for symptoms and signs of hypoglycaemia like sweating, tachycardia, altered mental state, confusion, and reduced consciousness.
2. Check the capillary blood glucose and, if < 4 mmol/L, immediately proceed to initiate treatment
3. Take a venous sample for formal blood glucose.
Common causes :
• Drug-induced: Sulphonylureas used to treat diabetes or excessive insulin
• Alcohol : Impairs hepatic gluconeogenesis
• Addison’s disease : Inadequate counter-regulatory response (e.g. cortisol) to insulin
• Liver failure : Impaired hepatic glucose production
• Certain medications e.g. paracetamol excess, quinine, salicylates
• If it is unclear why the person has hypoglycaemia, consider investigations such as renal function, liver function, full blood count, coagulation, and paracetamol/salicylate levels.
HYPOGLYCAEMIA VS HYPERGLYCAEMIA:
HYPOGLYCAEMIA -
Onset - Minutes.
EVENTS - Missed meal or increased activity.
SYMPTOMS - Hunger, perspiration, confusion, stupor, headache, tremors, fatigue, nervousness, seizures.
PHYSICAL FINDINGS - Tachycardia, normal to fast respiration rate
URINE - Negative for glucose and ketones
BLOOD GLUCOSE - < 4.0 mmol/L.
RESPONSE TO GLUCOSE - Dramatic
TREATMENT - Fast-acting glucose given orally or IV
HYPERGLYCAEMIA:
ONSET - Hours to days.
EVENTS - Omission of insulin
SYMPTOMS - Headache, nausea, abdominal pain, vomiting, polyphagia, polydipsia, acetone breath.
PHYSICAL FINDINGS - Kussmaul respirations, dehydration, tachycardia.
URINE - Positive for glucose and ketones.
BLOOD GLUCOSE - > 7.0 mmol/L when fasting or, > 11.1 mmol/L 2 hours after meal. Note symptoms usually only occur if there is marked hyperglycaemia (30mmol/L or more)
RESPONSE TO GLUCOSE - None
TREATMENT
- Regular insulin, fluids, electrolyte replacement.
Q.3. A 56 year old man was recently started on antihypertensive medication. His recent blood results show: Sodium 134 mmol/L Potassium 5.9 mmol/L Urea 7 mmol/L Creatinine 111 micromol/L. What is the most likely medication responsible for the abnormal results?
Correct Answer : A
Ramipril is an ACE inhibitor. ACE inhibitors are known for their effects on hyperkalemia.
HYPERKALEMIA : Untreated hyperkalemia may cause life-threatening arrhythmias.
ECG changes seen in hyperkalemia include tall-tented T waves, small P waves, widened QRS leading to a sinusoidal pattern, and asystole.
Causes of hyperkalemia that are important for exam:
• Acute renal failure
• Potassium-sparing diuretics, ACE inhibitors, angiotensin 2 receptor blockers, spironolactone
• Metabolic acidosis
• Addison's
Management :
1. Stop drugs that cause hyperkalemia
2. If ECG changes of hyperkalemia are seen : IV calcium gluconate
• IV calcium gluconate is used to stabilize the cardiac membrane
• Note that ECG changes are more accurate in identifying cardiac toxicity than plasma K+ levels
3. If a severely hyperkalemic - Insulin and dextrose infusion
Other methods to remove K+ from the body :
• Calcium meconium lowers potassium very slowly
• Loop diuretics
• Dialysis
Q.4. A 56 year old man has noticed a strange tingling around his mouth for the past few weeks. It was very subtle at first but has become increasingly apparent. On examination, twitching facial muscles were noticed. His past medical history includes type 1 diabetes. What is the most likely biochemical finding?
Correct Answer : C
This question is rather straightforward. The tingling around his mouth is called perioral paraesthesia, which, in combination with twitching facial muscles leads us to think that this is hypocalcemia. The history of diabetes was given as another hint for the diagnosis. He most likely has a degree of chronic renal impairment due to diabetes which supports the findings of hypocalcemia.
HYPOCALCAEMIA
Common causes :
• Vitamin D deficiency (osteomalacia)
• Chronic renal failure
Less common causes :
• Hypoparathyroidism (e.g. post thyroid/parathyroid surgery)
• Hyperphosphatemia
• Hypomagnesemia
Also, hyperventilation can include transient hypocalcemia however the serum calcium levels are usually normal.
The clinical history combined with parathyroid hormone levels will reveal the cause of hypocalcemia in the majority of cases.
Clinical Findings : Hypocalcaemia results in increased neural hyperexcitability such as seizures, tetany, circumoral numbness, and tingling of the extremities. Arrhythmias may develop because of a prolonged QT.
A mnemonic to help with clinical signs and symptoms is: “SPASMODIC”
• S -Spasm (carpopedal spasms = Trousseau's sign)
• P - Perioral paraesthesia • A - Anxious, irritable, irrational
• S - Seizures
• M - Muscle tone increased in smooth muscles
• O - Orientation impaired (time, place, and person) and confusion
• D - Dermatitis
• I - Impetigo herpetiformis (rare and serious)
• C - Chvostek’s sign, Cardiomyopathy (long QT interval on ECG)
Examination findings:
• Trousseau’s sign in which the wrist flexes and the fingers are drawn together in response to occlusion of the brachial artery.
• Chvostek’s sign is that facial muscles twitch in response to tapping over the parotid, revealing neuromuscular excitability due to the low calcium.
Management :
• Acute management of severe hypocalcemia is with intravenous replacement (10 ml of 10% calcium gluconate over 30 minutes)
• Further management depends on the underlying cause.
Q.5. A 30 year old man has frequent episodic headaches with palpitations. He suffers from anxiety and has the occasional tremor on both his hands. His blood pressure was found to be 160/110 mmHg. What is the most likely diagnosis?
Correct Answer : C
Phaeochromocytoma is a rare catecholamine secreting tumour.
Rule of 10 -
• Bilateral in 10%
• Malignant in 10%
• Extra-adrenal in 10% (most common site = organ of Zuckerkandl, adjacent to the bifurcation of the aorta)
• 10% are familial and may be associated with MEN type II, neurofibromatosis, and von Hippel-Lindau syndrome
• 10% not associated with hypertension
Features are typically episodic
• Hypertension (around 90% of cases and may be sustained)
• Headaches
• Palpitations
• Profuse sweating
• Anxiety
• Tremor
Mnemonic : PHaeochromocytoma P - Palpitations H- Headaches PH -PH lushings (flushing)
Tests -
• 24-hour urinary collection of metanephrines (sensitivity 97%)
Note: this has replaced a 24-hour urinary collection of catecholamines (sensitivity 86%)
Management : Surgical resection of the tumour is the treatment of choice and usually results in a cure for hypertension. However, the patient must first be stabilized with medical management:
• Alpha-blocker (e.g. phenoxybenzamine)
• Beta-blocker (e.g. propranolol)
Note: Alpha blocker must be given before a beta blocker. The reason behind medical management with alpha-blockers and beta-blockers is it is required to control blood pressure to prevent intraoperative hypertensive crises. Alpha blockade with phenoxybenzamine is started at least 7 to 10 days before operation to allow for expansion of blood volume. Only once this is achieved is the beta-blockade considered. If beta blockade is started too soon, unopposed alpha stimulation can precipitate a hypertensive crisis.
Q.6. A 50 year old lady presents with tiredness and weight gain over the last 6 months. She has glucose in her urine and has recently been diagnosed with hypertension. Investigations were performed and a diagnosis of Cushing’s disease was made. Which of the following findings is NOT found in Cushing’s disease?
Correct Answer : D
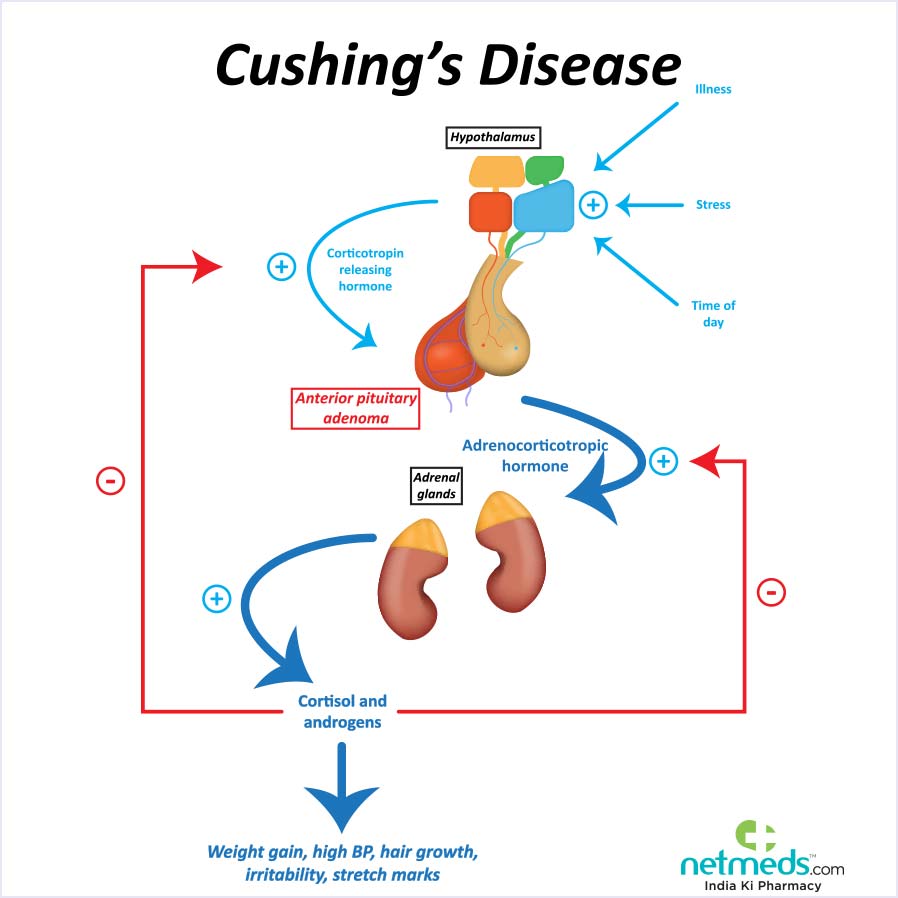
One must remember that Cushing’s disease is not the same as Cushing’s syndrome. Cushing’s syndrome are clinical signs and symptoms of excess cortisol.
Cushing’s disease is a pituitary adenoma that causes Cushing’s syndrome. Note, however, that Cushing’s syndrome could be caused by many other aetiologies besides a pituitary adenoma. In this step, they are asking about Cushing’s disease (pituitary adenoma causing cushing’s syndrome).
In Cushing’s disease, the pituitary adenoma produces massive amounts of ACTH which travels through the bloodstream and causes the normal adrenal glands to make excessive amounts of cortisol. This can lead to hyperactivity of both adrenal glands called bilateral adrenal hyperplasia. Remember that both adrenals would respond to ACTH equally causing bilateral adrenal hyperplasia rather than unilateral adrenal enlargement.
CUSHING’S SYNDROME :
- A clinical state caused by prolonged exposure to elevated levels of either endogenous or exogenous glucocorticoids.
Causes can be divided into 2 groups:
• Adrenocorticotropic hormone (ACTH)-dependent disease: Excessive ACTH from the pituitary (Cushing's disease), Ectopic ACTH-producing tumours (Especially small cell lung cancer and carcinoid tumours)
• Non-ACTH-dependent : Adrenal adenomas, Excess glucocorticoid administration. This is the chief cause.
Investigations:
• 24-hour urinary free cortisol as an outpatient screening tool
• Overnight dexamethasone suppression test
Administration of 1mg dexamethasone at midnight is followed by a serum cortisol measurement at 9 a.m. The 1 mg overnight dexamethasone suppression test is the best initial diagnostic test to establish a diagnosis of Cushing syndrome.
• ACTH levels : This is the next test to do once the diagnosis of Cushing’s syndrome is confirmed. We do this test to differentiate between ACTH-dependent and ACTH-independent aetiologies. ACTH levels are elevated with either a pituitary source of ACTH such as an adenoma or with an ectopic source.
• High-dose dexamethasone suppression test : This test is done to differentiate between a pituitary adenoma and an ectopic source.
Investigations for Cushing’s syndrome are a must especially when using a high-dose dexamethasone suppression test. It is a commonly asked question.
Q.7. A 44 year old lady has just recovered from an upper respiratory tract infection. She feels her heart racing and has increased perspiration. Her blood tests show: Free thyroxine (T4) 48 pmol/L Free triiodothyronine (T3) 15 pmol/L Thyroid stimulating hormone (TSH) 0.1 mU/L Thyroid antibodies negative. What is the most likely diagnosis?
Correct Answer : C
The patient has features of hyperthyroidism. Her T3 and T4 levels are high and her TSH levels are low. In subacute thyroiditis, patients will experience a hyperthyroid period which is typically followed by a hypothyroid phase as the pituitary reduces TSH production before resolving to euthyroid.
Hence, the symptoms are those of hyperthyroidism and hypothyroidism.
This stem includes having a history of upper respiratory tract infections because subacute thyroiditis is usually viral in origin, usually preceding an upper respiratory tract infection. Subacute thyroiditis is usually self-limited and is not treated with radioiodine.
Q.8. A 79 year old man has a diagnosis of lung cancer. He has a sodium level of 122 mmol/L but remains asymptomatic for hyponatraemia. What is the most appropriate management?
Correct Answer : C
This man is suffering from the effects of the syndrome of inappropriate antidiuretic hormone secretion (SIADH) which is leading to his hyponatraemia.
One of the causes of SIADH is small-cell lung cancer. Treating the cause of SIADH and restriction of fluid is the mainstay management for the majority of cases of SIADH. Consider Tolvaptan or demeclocycline if poor response after fluid restriction.
Q.9. A 65 year old man with a body mass index is 33 kg/m2 has been diagnosed with Type 2 diabetes mellitus. Diet and lifestyle modifications have failed to control his blood sugar over the last three months. He has no known allergies and does not take any regular medications. His blood results are as follows: Serum urea 3.6mmol/L Creatinine 82 mmol/L eGFR 79 ml/min. What is the most appropriate pharmacological management?
Correct Answer : C
Guidelines recommends biguanide (such as Metformin) as first-line treatment for patients with type 2 diabetes unless this is contraindicated. Contraindications to Metformin include eGFR less than 30 ml/min, severe infection, shock, hepatic insufficiency, and alcohol addiction – all of which predispose a risk of developing lactic acidosis. The patient is also obese hence sulfonylureas are not suitable as they can cause weight gain.
• Offer standard-release metformin as the initial drug treatment for adults with type 2 diabetes
• If metformin is contraindicated or not tolerated, consider initial drug treatment with a dipeptidyl peptidase-4 (DPP-4) inhibitor or pioglitazone, or a sulfonylurea.
Q.10. A 51 year old man presents to the medical out-patient clinic with the complaint of difficulty in climbing up stairs. He has been having these symptoms for a few months and has complaint to his general practitioner before of diffuse muscular aches in the limbs and back. He describes difficulty in getting up from a seated position and general weakness of his quadriceps. He has a poor diet and drinks about 3-4 units of alcohol a week. He gives a history that he does not go out much. He takes oral steroids during his COPD exacerbations which usually occurs three times a year. A full blood count, urea and electrolytes and a liver function test were done, and they show: Haemoglobin: 13.2 g/dL Platelets: 220 x 109/L White cell count: 5.8 x 109/L Sodium: 138 mmol/L Potassium: 4.1 mmol/L Bilirubin: 13 micromol/L Alanine transferase (ALT): 24 U/L Asparate transaminase (AST): 19 U/L Alkaline phosphatase (ALP): 391 U/L Gamma glutamyl transferase (Gamma-GT): 34 U/L Creatine kinase: 192 U/L. What is the most likely diagnosis?
Correct Answer : C
We can see from the lab values that this patient’s blood values are all within the normal reference range. The only thing that stands out is a slight increase in ALP. This is because the man is suffering from osteomalacia secondary to vitamin D deficiency.
Pain, exposure to sunlight, and a poor diet support osteomalacia as the answer. The amount of alcohol consumed or the occasional steroid intake is not significant enough to cause a myopathy.
The key point to remember in this question is vitamin D deficiency can be the cause of asymptomatic raised alkaline phosphatase.
In this case, raised ALP was due to bone!
Osteoporosis - Serum calcium - Normal, Serum phosphate - Normal, Alkaline phosphate - Normal
Paget’s disease - Serum calcium - Normal , Serum phosphate - Normal, Alkaline phosphate - High
Osteomalacia - Serum calcium - Low , Serum phosphate - Low, Alkaline phosphatase - High
OSTEOMALACIA : Osteomalacia can be defined as normal bony tissue but decreased mineral content. We use the term rickets because the epiphyses have not fused (in younger people).
Commonly asked causes -
• Vitamin D deficiency e.g. malabsorption, lack of sunlight, diet
• Renal failure
• Drug induced e.g. anticonvulsants
Presentation :
• Bone pain
• Fractures & Muscle tenderness
Q.11. A 30 year old woman complaints of decreased appetite and weight gain. She has been having irregular, infrequent periods in the last 10 months. She also feels tired and lethargic majority of the day. On inspection, she has a dry coarse skin. What is the most likely diagnosis?
Correct Answer : A
Primary hypothyroidism :
• Autoimmune hypothyroidism - Hashimoto's thyroiditis (associated with a goitre) and atrophic thyroiditis.
• Iatrogenic - Radioiodine treatment, surgery, radiotherapy to the neck
• Iodine deficiency - the most common cause worldwide, and goiter is present
• Drugs - amiodarone, contrast media, iodides, lithium, and antithyroid medication.
• Congenital defects - e.g. absence of thyroid gland
Secondary hypothyroidism :
• Isolated TSH deficiency
• Hypopituitarism - neoplasm, infiltrative, infection and radiotherapy
• Hypothalamic disorders - neoplasms and trauma
Symptoms :
• Tiredness, lethargy, intolerance to cold, dry skin and hair loss
• Slowing of intellectual activity - eg, poor memory and difficulty concentrating.
• Constipation
• Decreased appetite with weight gain
• Menorrhagia and later oligomenorrhoea or amenorrhoea
Signs :
• Dry coarse skin, hair loss, and cold peripheries
• Puffy face, hands, and feet (myxoedema)
• Bradycardia
In autoimmune hypothyroidism, patients may have features of other autoimmune diseases, such as vitiligo, pernicious anaemia, Addison's disease, and diabetes mellitus.
Q.12. A 28 year old woman presented to her GP with the complaint of amenorrhoea. On further questioning, she reveals that her last menstrual period was approximately twelve months ago and that she has not had a period since. Her menarche was at the age of twelve years. She reports no symptoms regarding the halt of her menses but claims that her menses have always been rather “light”. She has never had any children and does not think that she could be pregnant as she is not in a current relationship. She has lost 2.3 kilograms (around 5 pounds) of body weight over the past three months and reports a two week history of unilateral foot pain. She is a professional athlete and is currently training hard for the 10 km long distance race in the Olympics. She typically runs around twelve kilometres per day, at least five times per week. She has a very healthy lifestyle and does not smoke or drink alcohol. On physical examination, her body mass index is 19 kg/m2. There is dull pain on palpation along the fourth and fifth metatarsal of her left foot. The physical examination was otherwise normal. A blood sample was taken from the patient and her results are as follows: Follicle stimulating hormone (FSH) 10 U/L Luteinizing horome (LH) 5 U/L Prolactin 750 mU/L Oestradiol 120 pmol/L. What is the most likely diagnosis for this patient?
Correct Answer : C
In this scenario, the patient has not been menstruating for twelve continuous months. This is termed secondary amenorrhoea. Secondary amenorrhoea can be due to different causes but in this patient, it is most likely due to hypothalamic dysfunction.
She is an athlete by profession and hypothalamic failure can occur due to excessive exercise, stress, or being significantly underweight. In this patient, the body mass index (BMI) is within the normal range (18.5 to 25), so the cause of this patient’s hypothalamic dysfunction is excessive exercise and stress about the upcoming race.
In hypothalamic amenorrhoea, due to low levels of the gonadotrophin-releasing hormone (GnRH), there is a decrease in follicle-stimulating hormone (FSH) and luteinizing hormone (LH). This will further decrease the release of oestrogen from the ovary.
This can be seen in the laboratory values of this patient. It is less likely that the patient has premature ovarian failure as there will be an elevation of FSH, which is not the case in this patient. There is nothing to indicate in the scenario that the patient has polycystic ovarian syndrome, is taking ovulation induction drugs, or that she has coeliac disease.
AMENORRHOEA : Amenorrhoea is the absence of menstruation. Pathological amenorrhoea is the failure to menstruate for at least 6 months.
Amenorrhoea can be divided into:
• Primary amenorrhoea – lack of menstruation before age 16 years or 14 in the absence of secondary characteristics
• Secondary amenorrhoea – cessation of menstrual cycles following established cycles.
• Hypothalamic amenorrhoea o Most common o Usually due to low BMI or excessive exercise
• Polycystic ovarian syndrome (PCOS)
• Hyperprolactinaemia
• Premature ovarian failure, Raised FSH levels
• Anatomical problems, Usually results in primary amenorrhoea, Vaginal examinations to rule out imperforate hymen is important,
Pelvic ultrasound is also useful to determine the pelvic anatomy (Mullerian agenesis), Anatomical problems can also cause secondary amenorrhoea (Asherman’s syndrome)
• Thyroid problems, Both hyperthyroidism and hypothyroidism can cause amenorrhoea Don’t forget pregnancy as a cause of amenorrhoea Specific to look for in the stems
• Short stature – may indicate Turner syndrome
• Hirsutism, acne (androgen excess) – May indicate PCOS or hyperprolactinemia
• Menopausal symptoms in women before age 40 – May indicate premature ovarian failure
• Eating disorder – May indicate anorexia nervosa
• Galactorrhoea – May indicate hyperprolactinaemia.
Q.13. A 63 year old man who takes spironolactone and ramipril for hypertension and was found to have elevated potassium of 5.8 mmol/L on routine blood test on a day ward. He is otherwise well and has no allergies. An ECG is carried out which is normal. What is the best initial treatment in light of his potassium levels?
Correct Answer : D
Spironolactone is a potassium-sparing diuretic and ramipril is an ACEi. Both can cause hyperkalaemia. There are different severities of hyperkaleimia, and these are as follows:
Mild – 5.5-5.9 mmol/L Moderate – 6.0-6.4 mmol/L Severe: > 6.5 mmol/L The aggression of treatment depends upon the level of potassium, the rate of rise of potassium, and any ECG abnormalities seen. Remember the following in regards to ECG changes in hyperkaleimia
• ECG may be normal even in severe hyperkaleimia
• The absence of ECG changes does not mean there is no need for treatment
• The presence of ECG changes means a need for urgent treatment
• The severity of ECG changes does not always relate to the severity of hyperkaleimia Take note of how the question is phrased. It says the best INITIAL treatment. The best initial treatment is to discontinue the drugs that are directly contributing to this patient’s hyperkalemia. As we can see, the potassium level in this patient is only slightly elevated so stopping the medication would suffice. We can expect potassium levels to fall.
It is important to check for symptoms and do an ECG, but at this level, it is unlikely that the patient is symptomatic or an ECG is abnormal. In this question, the patient has a normal ECG with no symptoms so calcium gluconate is not indicated. This man is certainly not a candidate for dialysis.
Q.14. A 32 year old smoker presents with double vision on looking upwards. She also complains of pain on eye movement as well as dry eyes most of the day. The eye pain is described as an ache which is worse in the morning. On examination, her eyelids appear to move more slowly than the eyes on looking downwards. There is noticeable swelling of her eyelids. What is the most appropriate investigatin that would lead to a diagnosis?
Correct Answer : C
Although there is no mention of goitre or symptoms of hyperthyroidism, it is clear that she has a thyroid eye disease which in most cases is associated with Graves’ disease. The failure of the upper eyelid to follow promptly and smoothly with the downward movement of the eye secondary to thyroid disease is called Von Graefe’s sign.
A thyroid function test would be the most appropriate next step that would give a conclusive answer by showing elevated thyroid hormones (T3 and T4) with low thyroid stimulating hormone (TSH) Autoantibodies would generally be ordered when taking blood for the thyroid function test in reality when suspecting Graves’ disease.
But if you were to pick a thyroid function test or autoantibodies, you would pick a thyroid function test as it is more sensitive and can guide you with your management.
Q.15. A 27 year old woman presents with tremors, anxiety. She has a history of significant weight loss over the last 6 months.She has a heart rate of 112 beats/minute. Mild proptosis was seen on examination. What is the most likely mechanism that accounts for her symptoms?
Correct Answer : B
The given features are of thyrotoxicosis in which increased metabolism causes tremors, anxiety, weight loss, and an increased heart rate.
Q.16. A 55 year old woman with a history of a right mastectomy 5 years ago for breast cancer is brought into the Emergency Department by her husband as she has been increasingly drowsy over the past 48 hours. He mentions that she has been complaining of increased thirst for the past week. She suffers with depression and has started fluoxetine 4 months ago. What is the most likely cause of her symptoms?
Correct Answer : A
Drowsiness and increased thirst with a history of breast cancer should spark the thought of hypercalcemia as a differential. Breast cancers commonly spread to bones and remember, bone metastases are one of the most common causes of hypercalcemia. Fluoxetine has no significance in this scenario however depression can be worsened with hypercalcemia.
HYPERCALCAEMIA :
• Primary Hyperparathyroidism. This is the main cause of hypercalcemia. It is the most common cause of hypercalcemia but it is usually mild most of the time so most patients have no symptoms at all.
• Malignancy i.e. multiple myeloma, production of PTH-like molecule (Squamous cell carcinoma of the lung). This is a common cause of hypercalcemia that requires hospital admission.
• Familial Hypocalciuric , Hypercalcaemia
• Immobilization
• Sarcoidosis
Clinical features : Mnemonic: "moans, stones, groans, and bones".
• Neuro and psych: Hypercalcemia results in decreased mental activity leading to lethargy, confusion, and depression (Groans)
• Gastrointestinal: Hypercalcemia results in decreased bowel activity such as constipation (Moans).
• Renal: Hypercalcemia results in polyuria and polydipsia because of the induction of nephrogenic diabetes insipidus. Calcium also precipitates in the kidney, resulting in both kidney stones as well as nephrolithiasis. (Stones)
• Bone pain is only seen when it is hyperparathyroidism which is causing hypercalcemia (Bones)
• Cardiovascular: The ECG shows a short QT segment
Hypercalcaemia Management :
• The initial management of hypercalcemia is rehydration with normal saline, typically 3-4 liters/day. Increasing the circulating volume with 0.9% saline helps to increase the urinary output of calcium.
• Following rehydration bisphosphonates may be administered intravenously.
Other less-used options include:
• Calcitonin It has fewer side effects than bisphosphonates but is less effective in reducing hypercalcemia.
• Steroids in sarcoidosis
• Cinacalcet hydrochloride is a calcimimetic agent that effectively reduces parathyroid levels in patients with secondary hyperparathyroidism.
• Haemodialysis or peritoneal dialysis may be relevant in patients with severe hypercalcemia secondary to renal failure.
• Furosemide has a limited role. It is occasionally used where there is fluid overload but it does not reduce serum calcium.
Q.17. A 38 year old lady was admitted with severe abdominal pain and diarrhoea. On examination, hyperpigmentation is noticed at the palmar creases and buccal mucosa. She has muscle cramps and joint pain. Her blood pressure is 79/50 mmHg. What is the most likely diagnosis?
Correct Answer : D
The signs and symptoms are classic for Addison’s disease. The hyperpigmentation alone should prompt you to pick Addison’s disease. This is supported by the symptoms of abdominal pain and diarrhoea. Muscle pain, joint pain, and hypotension are also seen in Addison’s disease.
Sometimes they would give you a history of postural hypotension instead of hypotension. Note that hyperpigmentation is especially noticeable in buccal mucosa, lips, palmar creases. Adrenal Insufficiency Primary insufficiency (Addison's disease)
• An inability of the adrenal glands to produce enough steroid hormones. The most common cause for this in the developed world is autoimmune disease.
Secondary insufficiency
• Inadequate pituitary or hypothalamic stimulation of the adrenal glands.
Features :
• Nausea/vomiting
• Abdominal pain
• Diarrhoea/constipation
• Weakness
• Postural hypotension, dizzy
• Hyperpigmentation (only for Addison’s disease)
Think of adrenal insufficiency in all with unexplained abdominal pain or vomiting It is especially important to note for the exam that in secondary insufficiency, there is no hyperpigmentation of the skin as ACTH is decreased. Hyperpigmentation would only happen in primary insufficiency (Addison's disease) as the ACTH is extremely high.
Q.18. A 40 year old man has been feeling weak, tired and has been complaining of headaches. He has a blood pressure of 210/100 mmHg. He is not on any medications. His blood test show: Haemoglobin 130 g/L Serum sodium 144 mmol/L Serum potassium 2.9 mmol/L . What is the most likely diagnosis?
Correct Answer : A
Classically, the combination of hypokalaemia and hypertension should put primary hyperaldosteronism on the list of differentials.
Conn’s syndrome (Adrenal adenoma) :
• Hypertension associated with hypokalaemia
• Refractory hypertension, eg despite 3 antihypertensive drugs
• Hypertension occurring before age 40.
Classic features include:
• Hypertension
• Hypokalaemia (usually < 3.5 mmol/L, although 70% of patients may be normokalaemic)
• Metabolic alkalosis
• Sodium may be normal or at the high end of normal
• Weakness may be present from hypokalaemia
• Headaches and lethargy may also be present.
Management Medical management is used in the period before surgery.
Medical management involves the use of aldosterone antagonists - eg, spironolactone.
Surgery is the definitive treatment. Surgical treatment involves adrenalectomy. Laparoscopic surgery is safe and effective and may be better than open surgery.
Q.19. A 64-year-old man with multiple myeloma has been vomiting for the past 2 days. His blood tests show: Serum calcium 3.2 mmol/L Serum potassium 5 mmol/L Serum sodium 149 mmol/L Packed cell volume 55%. What is the most appropriate next step?
Correct Answer : C
Multiple myeloma itself is a cause of vomiting and is also associated with hypercalcemia which can cause sickness. As the patient has been vomiting for 2 days there may be considerable dehydration. He also has hypercalcemia which needed to be treated with IV fluids.
Q.20. A 54 year old woman was admitted to the medical ward with pneumonia. Due to her nausea, she has not had anything to eat or drink for the past 12 hours. She was started on intravenous antibiotics and intravenous fluids several hours ago whilst in the A&E department. A venous blood glucose sample taken in the medical ward showed a level of 9 mmol/L. Two days later she recovered and was discharged home. A blood test was organised 6 weeks after discharge which results show: Glucose (fasting) 6.3 mmol/L 2 hour postprandial glucose 7.1 mmol/L. What is the most likely reason for her hyerglycaemia on admission?
Correct Answer : D
Stress hyperglycemia refers to blood glucose that is elevated transiently due to the stress of an illness. It spontaneously resolves within several hours.
Hyperglycemia occurs due to stress hormones that are released as a response to tissue damage. Stress hyperglycemia is described in many situations such as in patients with pneumonia like in this stem. Other situations include myocardial infarction, stroke, or even post-surgery.
Examples of medical diseases that can cause secondary diabetes are cystic fibrosis, hemochromatosis, chronic pancreatitis, or Cushing’s syndrome.
Q.21. A 36 year old male diagnosed with glioblastoma has been receiving dexamethasone for several months to treat cerebral oedema. He started having diarrhoea and vomiting for the last 3 days. He complains of abdominal pain. He feels dizzy when he gets up from bed or stands up from a chair. What is the most likely reason for his symptoms?
Correct Answer : C
The symptoms here are consistent with adrenal insufficiency. The pathogenesis of this question is not clear. But it is most likely due to the cessation of steroids causing the Addisonian crisis. Bear in mind that, the commonest cause of secondary adrenal insufficiency is iatrogenic.
This is due to long-term steroid therapy leading to suppression of the pituitary-adrenal axis. This only becomes apparent on withdrawal of the steroids. Other causes are rare and include hypothalamic-pituitary disease leading to decreased ACTH production.
Steroid side effect is not the right answer because the side effects of steroids do not produce these symptoms. It is the cessation of the steroids that causes the symptoms of vomiting, abdominal pain, and sudden dizziness on standing which is evidence of postural hypotension.
Q.22. A 54 year old woman has presented with episodes of abdominal ache, vomiting and postural hypotension. She also has a dark pigmentation of her skin. A diagnosis of Addison’s disease was made. What is the most likely electrolyte abnormality expected in this patient?
Correct Answer : D
Addison's disease associated electrolyte abnormalities:
• Hyperkalaemia
• Hyponatraemia
• Hypoglycaemia
• Metabolic acidosis
Q.23. A newborn has congenital hypothyroidism. What feature might develop if no treatment is given?
Correct Answer : A
Congenital hypothyroidism :
The following features are late sequelae of congenital hypothyroidism and, with routine screening now available should never be seen nowadays.
• Physiological jaundice
• Goitre
• Delay in reaching normal milestones of development, short stature
• Coarse features with protruding tongue, broad flat nose, widely set eyes
• Sparse hair and dry skin
• Impaired mental development
• Epiphyseal dysgenesis, delayed dentition.
Q.24. A 33 year old woman has amenorrhoea and galactorrhoea. An MRI shows a 9mm tumour in the pituitary fossa. What is most appropriate management?
Correct Answer : C
Drug treatment should always be tried first. Cabergoline is a dopamine agonist used in treatment of prolactinoma.
Prolactinoma management :
Drug therapy - dopamine agonists
• Suppresses prolactin in most patients, with secondary effects of normalization of gonadal function, and terminates galactorrhoea.
• Shrinks tumours by shrinking the tumour, restoration of other hormonal axes may occur.
• Corrects visual field defect by chiasmal decompression thus immediate surgical decompression is not necessary .
• Note: Cabergoline is more effective in normalization of prolactin in microprolactinoma compared to bromocriptine. It is also associated with fewer side effects than bromocriptine Surgery Since the introduction of dopamine agonist treatment, transsphenoidal surgery is indicated only for patients who are resistant to, or intolerant of, dopamine agonist treatment Radiotherapy
Q.25. A 45 year old man with diagnosed colon cancer develops increased thirst, and frequent urination. He is also noted to have been losing weight in the last couple of months. His blood test shows a fasting blood glucose of 9 mmol/L. He has a pulse of 70 beats/minute, a blood pressure of 125/80 mmHg and a respiratory rate of 18 breaths/minute. What is the most appropriate management?
Correct Answer : A
The diagnosis of diabetes is very clear here. Increased thirst and increased frequency in urination along with weight loss is suggestive of diabetes mellitus. The fasting blood glucose of 9 mmol/L supports the diagnosis of diabetes. At the age of 45, the most likely type of diabetes is type 2 diabetes mellitus.
This is treated with oral hypoglycemic agents. The first line is usually metformin but this again depends on other factors and if there are any contraindications for its use. Insulin can be used in type 2 diabetes as well. But it is used in combination with metformin or it is used in very sick patients with high blood glucose (hyperosmolar hyperglycaemic state) often having a blood glucose level of more than 40 mmol/L.
Q.26. A 49 year old man with a diagnosis of squamous cell carcinoma of the lung is broght to the Accidents & Emergency Department by his wife as he is confused and lethargic. He complains of increasing weakness over the past few days. His wife is especially concerned as he has been having repeated falls over the past few days. His blood tests show: Sodium 149 mmol/L Calcium 3.2 mmol/l Potassium 4.5 mmol/l Urea 7 mmol/L Creatinine 190 micromol/L. What is the most appropriate initial step?
Correct Answer : B
This patient is suffering from hypercalcemia due to the production of a PTH-like molecule (Squamous cell carcinoma of the lung). The first step in management is always rehydration with IV fluids.
Q.27. A 35 year old man is feeling unwell after a recent myocardial infarction. A recent ECG of the patient shows widening of the QRS complex and tall-tented T wave. His recent blood results show: Sodium 136 mmol/L Potassium 6.2 mmol/L Urea 5 mmol/L Creatinine 90 ?mol/L. What is the most appropriate management?
Correct Answer : B
The ECG changes point towards hyperkalaemia. The need for urgent intravenous calcium gluconate is life-saving as this patient could have a cardiac arrest.
Q.28. A 31 year old man has profuse sweating, palpitations, headaches, flushing and hypertension. He was diagnosed with phaeochromocytoma and is to have a surgical removal of the tumour in a week. What is the most appropriate initial medication to prescribe?
Correct Answer : A
Please see Q-5
Q.29. A 35 year old man who a known type 1 diabetic has abdominal pain with deep breathing and drowsiness. The nurse has said that his breath has a fruity smell. His mucous membranes look dry. A urine dipstick testing shows marked glycosuria and ketonuria. Plasma glucose was elevated. What is the most appropriate immediate management?
Correct Answer : C
It is clear in this question that this man is suffering from diabetic ketoacidosis. Most DKA patients have a depletion of around 5 litres thus initial intravenous normal saline is very important. 0.9% saline is the replacement fluid of choice. Insulin should be infused continuously at 0.1u/kg/h.
Diabetic ketoacidosis :
• Characterised by hyperglycemia, acidosis, and ketonaemia
• May be a complication existing type 1 diabetes mellitus or be the first presentation
Precipitating factors :
The most common are:
• Infection
• Missed insulin doses
• Cardiovascular disease (e.g. stroke or myocardial infarction)
Features :
• Polyuria, polydipsia, dehydration, vomiting
• Abdominal pain
• Kussmaul respiration (deep hyperventilation)
• Acetone-smelling breath ('pear drops' smell)
• If the severe altered mental state, including coma
Diagnosis :
• Glucose > 11 or known diabetic
• pH < 7.3
• Bicarb < 15
• Ketones > 3 or urine dipstick ketones ++
Management :
• The most important initial intervention is appropriate fluid replacement followed by insulin administration.
• When plasma glucose is below 12 mmol/L then replace normal saline with 5% dextrose to prevent over-rapid correction of blood glucose and hypoglycaemia.
• Hypokalaemia may need to be corrected with KCL.
Q.30. A 39 year old woman has been feeling lethargic and tired. She has a blood pressure of 160/90 mmHg despite being on enalapril. Her blood test show: Haemoglobin 130 g/L Serum sodium 144 mmol/L Serum potassium 3.1 mmol/L. What is the most likely diagnosis?
Correct Answer : B
Please see Q-19
Q.31. A 26 year old woman with diagnosed carcinoma of the bronchus has been receiving steroid treatment for the last several months. She started vomiting and having severe abdominal pain for the past 2 days. She also complains of sudden dizziness in the morning. What is the most likely reason for her symptoms?
Correct Answer : C
The symptoms here are consistent with adrenal insufficiency. The pathogenesis in this question is not clear. But it is most likely due to cessation of steroids causing Addisonian crisis. Bear in mind that, the commonest cause of secondary adrenal insufficiency is iatrogenic.
This is due to long-term steroid therapy leading to suppression of the pituitary-adrenal axis. This only becomes apparent on withdrawal of the steroids. Other causes are rare and include hypothalamic-pituitary disease leading to decreased ACTH production.
Steroid side effect is not the right answer because the side effects of steroids do not produce these symptoms. It is the cessation of the steroids that causes the symptoms of vomiting, abdominal pain, and sudden dizziness in the morning which is evidence of postural hypotension.
Q.32. An 18 year old man has extreme thirst and polyuria. 6 months ago he had a significant head injury as the result of a road traffic accident. A diagnosis of diabetes insipidus is suspected. What is the most likely laboratory findings after fluid deprivation before the administration of desmopressin? (normal plasma osmolality 275-295 mosmol/kg and normal urine osmolality is 300-900 mosmol/kg)
Correct Answer : A
In diabetes insipidus, one can expect excess fluid loss with urine. Urine osmolality would be low and plasma osmolality would be high.
Diabetes Insipidus : Fluid deprivation test and assessment of response to vasopressin:
1. The patient is then deprived of fluids
2. Plasma osmolality is measured 4 hourly and urine volume and osmolality every 2 hours
3. The patient is then given IM desmopressin with urine volume and urine and plasma osmolality measured over the next 4 hours.
NORMAL PATIENT: Fluid restriction causes a decrease in urine volume and an increase in urine osmolality.
DIABETES INSIPIDUS: Despite fluid restriction, urine volume remains high and urine osmolality is decreased.
CENTRAL DIABETES INSIPIDUS: Urine volume decreases and urine osmolality increases after administering desmopressin.
Q.33. A 22 year old footballer collapses during a game and is brought into A&E by ambulance. During the initial evaluation, his respiratory rate is 14/min and pulse rate is 84 bpm, BP is115/80 mmHg. He is sweating profusely and muttering incomprehensible words. What is the most appropriate next course of action?
Correct Answer : B
The collapse could be due to hypoglycaemia. Checking venous or capillary blood with a glucose oxidase strip would be an appropriate first step before taking him for a CT scan or any other investigation. It is fast and easy and if hypoglycaemia is the cause, it can be quickly reversible. Always exclude hypoglycaemia in any patient with coma, altered behaviour, neurological symptoms, or signs.
Causes :
• The commonest cause is a relative imbalance of administered versus required insulin or oral hypoglycaemic drug. This results from: Exercise, Insufficient or delayed food intake, excessive insulin administration.
Other causes are:
• Alcohol (in addition to alcohol directly causing hypoglycaemia, the features of hypoglycaemia may be mistaken for alcohol intoxication or withdrawal)
• Addison’s disease
• Insulinomas
• Liver failure
• Malaria
Common features: Plasma glucose is normally maintained at 3.6-5.8mmol/L. Cognitive function deteriorates at levels < 3.0mmol/L, but symptoms are uncommon >2.5mmol/L.
• Sweating
• Pallor
• Tachycardia
• Palpitations
• Hunger
• Trembling
• Altered or loss of consciousness
• Fitting
• Coma
Diagnosis:
• Venous or capillary blood with glucose oxidase strip (BMG)
• If < 3.0mmol/L, take a venous sample for a formal blood glucose level, but do not delay treatment.
Q.34. A 68 year old woman was diagnosed with Type 2 Diabetes Mellitus. Diet and lifestyle modifications have failed to control his blood sugar over the last three months. She has no known allergies and takes Ramipril 5mg daily. She has a body mass index is 35 kg/m2. Her blood results are as follows: Serum urea 13.2 mmol/L Creatinine 390 mmol/L eGFR 25 ml/min. What is the most appropriate pharmacological management?
Correct Answer : A
Guidelines recommends biguanide (such as Metformin) as first-line treatment for patients with type 2 diabetes unless this is contraindicated. This patient is obese and has poor renal function, hence biguanides, sulfonylurea, and sodium-glucose co-transporter 2 inhibitors are contraindicated. Pioglitazone causes weight gain so this is not an appropriate option as well.
Q.35. A 33 year old man comes to clinic to have an oral glucose tolerance test. What is the plasma glucose level two-hours after glucose intake which indicates an impaired glucose tolerance?
Correct Answer : C
Impaired glucose tolerance is defined as a fasting plasma glucose concentration of less than 7.0 mmol/L with a two-hour oral glucose tolerance test value of 7.8 to 11.1 mmol/L.
Q.36. A 46 year old woman who lives in the US complains of weight gain, constipation and sensitivity to cold. Her pulse is regular at 50 beats/minute. What is the most likely underlying mechanism for her condition?
Correct Answer : B
She is suffering from hypothyroidism. Note that Iodine deficiency (nutritional causes) is the most common cause of hypothyroidism worldwide but in developed countries, autoimmune hypothyroidism is more prevalent.
Q.37. A 29 year old male comes to clinic with a swollen, painful right wrist joints. On further questioning, he gives a history of noticing a change in his shoe size. His other complains also include constipation, feeling cold and needing more warm clothes to keep him warm. On examination, his skin is found to be dry and his right wrist is erythematous and tender to touch. What is the most likely diagnosis?
Correct Answer : C
This is a two-part question. The first part is recognizing the symptoms of hypothyroidism. The change of shoe size is probably due to myxoedema. The other features given like constipation, cold intolerance, and dry skin are features seen in hypothyroidism.
The second part is recognizing that pseudogout may be precipitated by hypothyroidism. This explains the swollen wrist joint. Pseudogout may have an acute presentation like gout. It may also present in an asymptomatic and chronic form.
The knee is the most commonly affected joint. The other joints commonly affected are the wrist, shoulder, and ankle. Presentation is similar (but usually milder) to acute gout, with acute joint pain and swelling. Attacks may be associated with fever and a raised white cell count. Positive birefringent crystals in synovial fluid evaluation are pathognomonic for acute pseudogout.
Q.38. A 4 year old child is brought to the emergency department by his mother with complaints of vomiting for the past 4 days. On examination, he has clinical signs of mild to moderate dehydration. What is his arterial blood gas profile likely to show?
Correct Answer : D
Prolonged vomiting causes loss of H+ from the body resulting in metabolic alkalosis. Thus, the pH will be higher than usual. To compensate for metabolic alkalosis, the respiratory system will retain carbon dioxide through slower breathing or alveolar hypoventilation in an attempt to diminish the change in pH that would otherwise occur. This would result in a higher PCO2.
Q.39. A 29 year old woman stopped taking combined oral contraceptive pills 11 months ago as she and her partner wuold like to have a child. They have been having regular intercourse but she fails to become pregnant. She has not had her menstrual period since stopping the contraceptive pill H Her blood results show: Follicle-stimulating hormone (FSH) 11 IU/L Luteinizing Hormone (LH) 15 IU/L Prolactin 2500 ng/mL Oestradiol 53 pmol/L. What is the most likely cause?
Correct Answer : D
Prolactinomas are a form of pituitary tumour secreting prolactin. Hyperprolactinemia in premenopausal women causes hypogonadism which results in symptoms of infertility, oligomenorrhoea, amenorrhoea, and less commonly galactorrhoea. Hypothalamic amenorrhoea usually occurs due to chronic illness like being significantly underweight and rightly so, it is seen commonly in anorexia nervosa.
Diagnosis of hypothalamic amenorrhoea with biochemical findings of low serum gonadotropins and low oestradiol with clinical picture of excessive exercise, low weight or stress. There are no features of PCOS in this stem. In regards to biochemical tests, elevated insulin levels, elevated LH levels, and moderately elevated testosterone levels would be seen in PCOS The oestrogen levels would be low and the gonadotropic hormones would be raised in premature ovarian failure.
HYPERPROLACTINAEMIA :
Excess prolactin secretion is a common clinical problem in women and causes the syndrome of galactorrhoea-amenorrhoea. The amenorrhoea appears to be caused by inhibition of the hypothalamic release of luteinizing hormone-releasing hormone (LHRH) with a decrease in luteinizing hormone (LH) and follicle-stimulating hormone (FSH) secretion. Prolactin inhibits the LH surge that causes ovulation. Although hyperprolactinemia is also seen in men, gynecomastia and especially galactorrhoea is very rare.
Etiology hyperprolactinemia can be seen in natural physiologic states such as pregnancy, nipple stimulation/suckling, stress Pituitary tumours such as prolactinomas Hypothalamic disease mass compressing stalk (craniopharyngioma, meningioma) Hyperprolactinaemia can also occur with decreased inhibitory action of dopamine. (e.g. Antipsychotic agents). Antipsychotics are the most common pharmacological cause of hyperprolactinemia. Some are known dopamine D2 receptor antagonists and would raise serum prolactin. Remember a few of them like risperidone and haloperidol as a cause of hyperprolactinemia.
Q.40. A 34 year old woman is referred to the endocrine clinic with a history of thyrotoxicosis. At her first appointment she is found to have a smooth goiter, lid lag and bilateral exophthalmos with puffy eyelids. She wants to discuss the treatment of her thyroid problem as she is keen to become pregnant. What is the most likely treatment to be given to her?
Correct Answer : D
Of the three recognized treatment options for hyperthyroidism (radioiodine therapy, antithyroid drug therapy, and surgery), generally, only drug therapy (preferably propylthiouracil) is considered for treating pregnant women. As this patient is not yet pregnant but trying to conceive, there is no consensus on the treatment option. However, propylthiouracil would likely be the preferred treatment as she has not attempted any anti-thyroid drug therapy in the past.
Both propylthiouracil (PTU) and carbimazole are effective in controlling the disease in pregnancy. Historically, propylthiouracil has been preferred in pregnancy because it is not associated with aplasia cutis and omphalocele, which may be the case for carbimazole. However, recent concern regarding the hepatotoxicity of PTU, particularly in children, has led to recommendations that it should only be prescribed in the first trimester.
Nonetheless, PTU is the drug of choice when trying to conceive (preconception) and also in the first three months of pregnancy. If PTU is not available, carbimazole can be used. Surgical management is also something to consider and in several women planning to become pregnant, it is the therapy of choice. As stated above, there is no consensus as to which management pathway should be used but propylthiouracil would likely be attempted first before consideration of surgery.
While subtotal or near-total thyroidectomy achieves a 98% cure rate, it is indicated if there is a suboptimal response to anti-thyroid medication or radioiodine. Anti-thyroid medication has a slightly increased risk of babies developing structural abnormalities, so it is common for physicians to encourage patients to choose to have definitive treatment of Grave’s disease with radioactive iodine or surgery before considering pregnancy. But then again, a trial of anti-thyroid medication is likely to be attempted first. It is also important to note that the patient has symptoms of Graves’s ophthalmopathy of which radioactive iodine should not be used as part of the management.
There is evidence that Graves’s ophthalmopathy worsens after administration of radioactive iodine. Pre-pregnancy counseling is also important. It should include informing the patient of the importance of euthyroidism before conception since uncontrolled hyperthyroidism is associated with an increased risk of congenital abnormalities. If the patient was already pregnant, the decision to pick propylthiouracil becomes more clear.
Also, points to note if the patient is pregnant are as follows:
• The use of iodides and radioiodine is contraindicated in pregnancy
• Patient still needs to continue taking anti-thyroid medication during pregnancy. As anti-thyroid medication can cross the placenta, the lowest possible dose should be prescribed.
• If already on carbimazole, change carbimazole to propylthiouracil.
• Thyroidectomy is rarely performed in pregnancy. It is reserved for patients not responding to anti-thyroid medication. If necessary, it is preferable to perform thyroidectomy in the second trimester.
Q.41. A 45 year old woman has lost weight 12 kg over the past half year. She has also noticed episodes where she feels her heart beat beating rapidly. She has a regular pulse rate of 90 bpm. Her ECG shows sinus rhythm. What is the most appropriate investigation to be performed?
Correct Answer : A
Hyperthyroidism Symptoms: Weight loss, tachycardia, diarrhoea, oligomenorrhoea, irritability, heat intolerance, tremors, sweating, and weight loss despite increased appetite, atrial fibrillation/sinus tachycardia.. The most sensitive test in thyroid diseases is the TSH. If the TSH is normal, then the patient is euthyroid.
Q.42. A 9 year old girl who is known to have type 1 diabetes mellitus presents with drowsiness and deep breathing. Her blood glucose is 18 mmol/L. She has a blood pressure of 120/80 mmHg and her mucous membranes are dry. What is the most appropriate next step?
Correct Answer : D
This child is likely suffering from diabetic ketoacidosis. An arterial blood gas at this time would be a good investigation of choice to determine the severity.
Q.43. A 65 year old female was admitted to the hospital with a severe community acquired right lower lobe pneumonia as seen on a chest x-ray. Treatment was commenced with 1.2 g of co-amoxiclave intravenously. On the fourth day, her skin, sclerae and mucosae were noted to be yellow in colour and it was also observed that she was passing dark urine. The patient’s vitals were noted as follows: Blood pressure 120/80 mmHg Heart rate 80 beats per minute Respiratory rate 30 breaths per min A liver function test was subsequently done and the results are shown as follows: Bilirubin 65 micromol/L (3-17 micromol/L) Aspartate transaminase (AST) 1500 IU/L (5-35 IU/L) Alanine transferase (ALT) 1850 (5-35 IU/L) Alkaline phosphatase (ALP) 290 IU/L (30-130 IU/L) The patient’s past medical history is significant for her drinking around 20 units of alcohol per week for the last ten years. What is the most likely cause of this patient’s deranged liver function tests?
Correct Answer : C
The scenario depicted here describes a typical presentation of drug-induced hepatitis. As is clear from the stem, this patient was treated with intravenous antibiotics due to severe community-acquired pneumonia. It is essential to remember that co-amoxiclav (amoxicillin + clavulanic acid) delivered in high therapeutic doses may induce cholestasis in patients who are already susceptible to liver damage as it is metabolized mainly in the liver. Therefore to answer this question correctly, it is important to know about the laboratory changes in different types of liver diseases.
Elevated bilirubin and massive elevations of ALP and AST are seen in drug-induced hepatitis. In this patient, it has likely developed due to impaired hepatic excretion (cholestasis) because of the high hepatic toxicity of clavulanic acid that is present in co-amoxiclav. Drug-induced liver impairment is less likely to develop in healthy patients.
It has likely occurred here because this patient has a history of prolonged alcohol intake and this patient’s alcohol intake is a predisposing factor for a drug-induced hepatitis.
Q.44. A 39 year old man has complaints of galactorrhoea over the past month. On examination of his visual fields, a bitemporal hemianopia was noted. What is the most likely diagnosis?
Correct Answer : C
The pituitary macroadenoma is causing compression of the optic chiasm causing bitemporal hemianopia. Galactorrhoea (although rare in men) occurs because the adenoma is secreting prolactin.
Q.45. A 26 year old woman comes to the emergency department with vomiting, abdominal pain and tachypnoea. Her breath has a fruity smell. She has a heart rate of 99 beats/minute and a respiratory rate of 30 breaths/minute. Her blood pressure is 110/70 mmHg. Her blood and urine results show: Blood Ketones 3.3 mmol/L (high) Urine Ketones +++ Venous pH 7.2 (low) Blood Glucose 22 mmol/L (high). What is the most appropriate immediate management?
Correct Answer : A
It is clear in this question that this man is suffering from diabetic ketoacidosis. Most DKA patients have a depletion of around 5 litres thus initial intravenous normal saline is very important. 0.9% saline is the replacement fluid of choice. Insulin should be infused continuously at 0.1u/kg/h.
Q.46. A 42 year old lady has unexplained milk secretion from her nipples. Her last menstrual period was 6 months ago. She says she has been experiencing a loss of libido. What is the most likely diagnosis?
Correct Answer : A
Galactorrhoea is one of the features of hyperprolactinemia (although it is uncommon in a premenopausal woman). Hirsutism, amenorrhoea, vaginal dryness, and loss of libido are features that are consistent with hyperprolactinemia.
Q.47. A 55 year old man who is a chronic alcoholic stops drinking alcohol 4 days ago. He usually drinks around 5 cans of beer a day for the past 6 years. Since stopping, he has been feeling nauseous and has been vomiting several times a day. There is no blood in his vomitus and he reports normal coloured stool. He denies sweating, palpitations, and tremors. What is the most likely electrolyte abnormality?
Correct Answer : D
The likely electrolyte imbalance would be low potassium. This is because he has been vomiting severely over the past few days. Firstly, potassium may be lost with vomitus. Secondly, metabolic alkalosis would be present due to excretion of hydrochloric acid with vomitus and state of volume depletion which would additionally cause a loss of potassium through the renal system via aldosterone-mediated mechanisms. Another reason for hypokalemia is that he is a chronic alcoholic.
Many patients with potassium deficiency are also magnesium deficient. So if the potassium was very low, a magnesium level should be ordered. He would also require an ECG, replacement of potassium, and a cardiac monitor as cardiac arrhythmias are the most serious emergency due to hypokalemia. If the magnesium levels came back low, he would also require magnesium replacement.
Q.48. A 32 year old man has paroxysmal hypertension. He has frequent headaches and complains of profuse sweating. His blood pressure remains high despite having started on an ACE inhibitor. What is the most likely diagnosis?
Correct Answer : A
Please see Q-5
Q.49. A 40 year old male with pre-existing glomerulonephritis deteriorates and presents with oliguria. Lab results show the following: Serum K+ = 7.8mmol/L Urea = 13 mmol/L Creatinine = 342 mmol/L GFR = 19mL/h. What is the most appropriate initial management?
Correct Answer : C
Calcium gluconate is the most appropriate initial management as it is used to prevent cardiac arrhythmia. It prevents cardiac arrest or life-threatening cardiac arrhythmia to buy time till definitive measures are taken.
Q.50. A 33 year old patient has a routine fasting blood glucose of 7.4. He is otherwise well and has no complaints of polydipsia or polyuria. He has no medical issues in the past. What is the most appropriate next step in action?
Correct Answer : B
Diabetes may be diagnosed based on one abnormal plasma glucose (random - 11.1 mmol/L or fasting - 7 mmol/L) in the presence of diabetic symptoms (e.g. polydipsia, polyuria, recurrent infections, drowsiness, coma). In asymptomatic patients such as this stem, two fasting venous samples in the abnormal range ( 7 mmol/L) are recommended for diagnosis.
Q.51. A 32 year old woman with headaches and lethargy has hypertension. A recent blood test shows a serum potassium of 2.9 mmol/L. What is the most appropriate hormone test to order?
Correct Answer : B
Hypertension and hypokalemia are seen in hyperaldosteronism. Aldosterone would be the most appropriate hormone test.
Q.52. A 31 year old man has tremors, profuse sweating and palpitations. His blood pressure was measured at 160/115 mmHg but dropped to 139/92 on standing. What is the most likely diagnosis?
Correct Answer : B
Postural hypotension is defined as a reduction in systolic blood pressure of 20 mmHg or more after standing for at least one minute. Postural hypotension can be seen in phaeochromocytoma.
Q.53. A 24 year old schizophrenic has been under antipyschotic treatment for the last year. He has been experiencing headaches and erectile dysfunction. Which medication is most likely to have caused this?
Correct Answer : D
Haloperidol can raise prolactin levels causing hyperprolactinemia which can cause erectile dysfunction. Fluoxetine which is a selective serotonin reuptake inhibitor (SSRI) can also cause erectile dysfunction however it is not classed as an antipsychotic treatment.
Q.54. An 8 year old boy with a body mass index of 25 kg/m2 was admitted to a surgical ward following a road traffic accident. He was found to have glycosuria. When he recovered from his injury the glycosuria resolved. What is the most appropriate follow-up investigation?
Correct Answer : A
Glycosuria can be seen during any event that contains stress to the body. Stress-related cortisol release can elevate blood glucose and in severely ill patients they may elevate glucose beyond the renal threshold leading to glycosuria. Once the patient recovers, glycosuria resolves. Nonetheless, a fasting blood glucose concentration should be performed in his follow-up visits to exclude diabetes.
Q.55. A 75 year old man with a recent diagnosis of prostate cancer has confusion, thirst, lower back pain and abdominal pain. An ECG was performed which showed shortening of QT interval. What is the most appropriate investigation?
Correct Answer : B
It is clear from the clinical features that this man is suffering from hypercalcemia. Prostate cancer is typically associated with metastatic osteoblastic lesions, hypocalcemia, and hypophosphatemia. Although, hypercalcemia is sometimes encountered like in this case. Prostate cancer cells in a bone may make extra calcium pass out of the damaged bone and into the blood.
Hypercalcaemia explains the symptoms in this stem of confusion, thirst because of polyuria, and abdominal pain. The back pain seen in this stem is due to metastatic bone disease. As there are no symptoms of tingling or numbness in the legs in this stem, there is no rush to perform a magnetic resonance imaging of the spine to investigate for malignant spinal cord compression.
Obtaining a serum calcium would be the most appropriate since ECG changes are already seen and hypercalcemia would need to be treated as soon as possible. Remember the clinical features of hypercalcemia.
PROSTATE CARCINOMA PRESENTATION :
- Increasing age is the most important risk factor.
- Men of black African-Caribbean family origin
- First-degree relative with prostate cancer
Presentation Lower urinary tract symptoms (LUTS) do not particularly raise suspicion of prostate cancer because LUTS are common in older men and are rarely the presenting symptom of prostate cancer.
However, locally advanced prostate cancer may cause obstructive LUTS :
• Raised PSA on screening
• Weak stream, hesitancy, sensation of incomplete emptying, urinary frequency, urgency, urge incontinence
• Urinary tract infection
Locally invasive disease:
• Haematuria, dysuria, incontinence
• Haematospermia
• Perineal and suprapubic pain
• Obstruction of ureters, causing loin pain, anuria, symptoms of acute kidney injury or chronic kidney disease
Metastatic disease:
• Bone pain or sciatica
• Paraplegia secondary to spinal cord compression
• Lymph node enlargement
• Lethargy (anaemia, uremia)
• Weight loss, cachexia.
Q.56. A 44 year old woman has menstrual irreuglarities and unexplained milk discharge from her nipples. An MRI reveals a pituitary tumour. What is the most likely visual abnormality associated with a pituitary tumour?
Correct Answer : D
Pituitary tumour by pressing optic chiasma causes bitemporal hemianopia.
Q.57. A 41 year old obese woman has recently undergone a blood test. Her results show: Fasting blood sugar 6 mmol/l Oral glucose tolerance test 10.1 mmol/l. What is the most likely diagnosis?
Correct Answer : A
Impaired glucose tolerance is defined as a fasting plasma glucose concentration of less than 7.0 mmol/L with a two-hour oral glucose tolerance test value of 7.8 to 11.1 mmol/L.
Q.58. A 29 year old known diabetic man comes to A&E after falling down the stairs. While waiting in the waiting room, he becomes unconscious and collapses. What is the most appropriate initial investigation?
Correct Answer : B
A random blood sugar is the first investigation to do. In an unconscious patient especially a diabetic, ruling out hypoglycemia has to be treated as a priority. It is easy and fast to perform.
Q.59. A 9 year old boy had glycosuria following an appendectomy. He has a history of diabetes mellitus. A few days later, his glycosuria resolved. What is the most appropriate follow-up investigation?
Correct Answer : B
Glycosuria can be seen during any event that contains stress to the body. Stress-related cortisol release can elevate blood glucose and in severely ill patients they may elevate glucose beyond the renal threshold leading to glycosuria. Once the patient recovers, glycosuria resolves. Nonetheless, a fasting blood glucose concentration should be performed in his follow-up visits to exclude diabetes.
Q.60. An 8 year old boy presents to his GP surgery with his mom with complaints of lethargy, increased thirst and increased frequency of urination for the past month. A urine dipstick is positive for glucose. On examination, he looks well and is seen playing. There are no signs of dehydration. What is the most appropriate next investigation?
Correct Answer : B
The first step for diagnosing diabetes is having the result of fasting blood glucose. In the presence of symptoms, a fasting glucose 7 mmol/L confirms the diagnosis. In the absence of symptoms, you would need two separate fasting glucose results of 7 mmol/L. HbA1c can also be used as a diagnostic test for diabetes, but since it is a more expensive test, it would be ideal to use fasting blood glucose to diagnose diabetes and to use HbA1c at times of clinical uncertainty.
The oral glucose tolerance test which was the gold standard for diagnosing diabetes in the past is now rarely used because it is time-consuming and troublesome. Patients would have to be in the hospital for at least 2 hours with two venipunctures performed. Oral glucose tolerance test still has its place in diagnosing gestational diabetes and remains the gold standard for that although we may see a change in diagnostic tests for gestational diabetes in the next few years.
Q.61. A 62 year old man had a bowel resection 3 days ago for colorectal cancer. His urine output has been low since the procedure and he is now becoming breathless. He has a blood pressure of 130/95 mmHg. On auscultation, he has crackles at both lung bases and on palpation, he has sacral oedema. His blood tests show: Haemoglobin 109 g/L Serum urea 50.5 mmol/L Serum creatinine 603 mmol/L Serum potassium 6.72 mmol/l. What is the most appropriate immediate management?
Correct Answer : D
The most significant point to highlight in this case is his potassium levels. His potassium levels are high enough to cause a life-threatening arrhythmia. The high levels of potassium could be due to many reasons but he is likely suffering from acute kidney injury due to heart failure causing low blood volumes. The hyperkalaemia needs to be addressed first to prevent cardiac arrest. Shifting potassium intracellularly is a useful holding measure in life-threatening hyperkalemia.
This can be done quickly by administering Insulin Actrapid 10 units in 50 mL of Glucose 50% intravenously over 30 minutes via a volumetric pump. Insulin stimulates cellular uptake of potassium, so it drops serum potassium levels rapidly, and glucose is given with insulin to prevent hypoglycemia. This would reduce serum potassium levels by 0.65 - 1.0mmol/L but the reduction only lasts for about an hour.
This is usually followed by monitoring blood glucose after 15 minutes, 30 minutes, and then hourly for up to 6 hours as there is a risk of late hypoglycemia. Again this regimen would differ depending on your local hospital guideline for hyperkalaemia. Just remember that capillary blood glucose needs to be checked before, during, and after insulin-glucose infusion.
Other methods that can be used to treat life-threatening hyperkalemia include 10-20 mg nebulized salbutamol - this reduces serum potassium (0.5-1.0 mmol/L) in 15-30 minutes and lasts for two hours.
• Remove excess potassium - Calcium Resonium has a slow onset of action (at least 2-6 hours) (This is the reason it is not the answer to this question. The action to correct hyperkalemia is too slow. Calcium Resonium has no role in an acute situation)
• Dialysis - This is useful if all the above measures have been done and the patient still has high serum potassium.
The use of sodium bicarbonate is controversial in patients with acidosis and there is still insufficient evidence to justify routine use. It is therefore likely to always be the WRONG answer in the test in the context of hyperkalemia. If intravenous calcium gluconate was one of the options, that would also be a correct answer because it is needed to stabilize the cardiac membrane to prevent arrhythmias. Intravenous calcium has rapid effects, resulting in improvement of ECG abnormalities within minutes of administration.
Q.62. A 43 year old man complains of thirst, lethargy and frequent urination. He was diagnosed with multiple myeloma. What is the most likely biochemical abnormality to be associated with this condition?
Correct Answer : A
One of the causes of hypercalcemia is multiple myeloma. Thirst, lethargy, and increased frequency of urination are all symptoms of hypercalcemia.
Q.63. A 44 year old man presents to the Emergency Department with palpitations, nausea, vomiting and drowsiness. His ECG shows tall tented T waves and a wide QRS complex. His blood results show the following: Calcium 2.65 mmol/L Potassium 6.3 mmol/L Urea 21 mmol/L Magnesium 0.65 mmol/L eGFR 41 On viewing his blood results 2 months ago, his previous eGFR was found to be normal. What is the most appropriate next step?
Correct Answer : B
There is clear derangement of his electrolytes but what is important to know is to treat the hyperkalemia first as levels higher than 6 with ECG changes can be life-threatening. His hyperkalemia is probably secondary to an acute kidney injury which can be seen with a low eGFR. He would require intravenous fluids but the most important part of management now is intravenous calcium chloride (or calcium gluconate) and cardiac monitoring.
The slightly elevated calcium and low magnesium can be managed after stabilizing the cardiac membrane with calcium chloride or calcium gluconate. Nebulized salbutamol has a role in lowering potassium quickly and can lower potassium levels by 1 mmol/L in about 30 minutes and maintain it for up to 2 hours however in moderate hyperkalemia such as in this stem (values of 6.0-6.5 mmol/L), salbutamol nebulizers may be considered but calcium chloride (or calcium gluconate) is a must.
Often salbutamol nebulizers, calcium chloride, and intravenous insulin with dextrose are all prescribed at the same time, but if one were to choose, pick intravenous calcium chloride (or calcium gluconate).
Q.64. A 55 year old man has weight loss, dyspnoea and syncope. He smokes 20 cigarettes/day. Investigations confirm squamous cell carcinoma in the left bronchus. What is the most likely biochemical abnormality to be associated with this condition?
Correct Answer : A
Hypercalcemia can occur due to the production of PTH like molecule in squamous cell carcinoma of the lung.
Q.65. A 12 year old boy is clinically obese and is the shortest in his class. His medical history includes having a renal transplant 2 years ago. There are purple striae noticed on his skin. What is the most likely diagnosis?
Correct Answer : D
Cushing’s syndrome is the most likely diagnosis here. The history of a renal transplant means that he is probably taking exogenous steroids which are causing his syndrome.
Q.66. A 34 year old woman presents with truncal obesity, easy bruising, hyperglycaemia and depression. She has a blood pressure of 165/95 mmHg. Which of the following investigations will be most helpful in localizing the cause of Cushing’s syndrome?
Correct Answer : D
The features are representative of Cushing’s syndrome. A high dose dexamethasone suppression test to differentiate between a pituitary adenoma and an ectopic source which is producing ACTH.
Q.67. A 28 year old woman complains of tiredness, lethargy, and intolerance to cold. She has a history of Addison’s disease. Her skin looks dry on examination. She has been having infrequent periods in the one year and her last menstrual period was 3 months ago. What is the most likely diagnosis?
Correct Answer : B
Please see Q-12
Q.68. A 45 year old woman presented to Emergency Department with the complaint of nausea and vomiting for one week. She also reported a three month history of progressively worsening fatigue. The patient had been previously very active as a swimming instructor but, for the past three months, had been unable to carry out her job because of a lack of energy. She also reported a poor appetite for the preceding months and had lost approximately three kilograms of body weight during that time as well. One week prior to admission, she had also started feeling dizzy and described the room as spinning around her when she stood for long periods of time. Her blood pressure was measured on admission and showed 140/80 mmHg (lying down) and 110/60 mmHg (standing up). Blood tests were also done and the results are as follows: Sodium 124 mmol/L Potassium 6.5 mmol/L Urea 7.9 mmol/L Creatinine 100 micromol/L. What is the most common cause of her pathology?
Correct Answer : B
The patient has presented with the classic symptoms of Addison’s disease. This describes an inability of the adrenal glands to produce sufficient steroid hormones. The most common cause of adrenal insufficiency is autoimmune in nature (85% of cases).
Other causes include surgical removal of the adrenal glands, injury, infections (of which TB is the commonest cause worldwide), haemorrhage, and infarction. The most common feature of Addison’s disease is fatigue and weakness. Patients also complain of dizziness and vertigo – this is due to postural hypotension.
Aldosterone helps maintain blood pressure and salt and water homeostasis in the body by helping the kidneys retain sodium and excrete potassium. In adrenal insufficiency, the levels of aldosterone fall so low that the kidneys are unable to regulate water and salt balance, leading to a drop in both blood volume and blood pressure.
For the exam, it is important to remember that the definitive investigative test to confirm Addison’s disease is the ACTH stimulation (Synacthen) test. Mineralocorticoid replacement is required in this patient. Fludrocortisone is usually used.
Q.69. A 39 year old man has 7 kg unintentional weight loss in the last two months despite having a good appetite. He also complains of palpitations, sweating and diarrhoea. He has a lump in front of his neck which moves on swallowing. What is the most appropriate diagnosis?
Correct Answer : C
He has signs and symptoms of hyperthyroidism. The mass is likely to be a goitre rather than thyroid cancer as thyroid cancers usually do not manifest with symptoms of hyperthyroidism.
HYPERTHYROIDISM CLINICAL FEATURES :
• Hyperactivity, irritability
• Insomnia
• Heat intolerance
• Sweating
• Palpitations
• Fatigue
• Weight loss
• Increased appetite
• Pruritus
• Increased stool frequency
• Oligomenorrhoea or amenorrhoea
Signs :
- Sinus tachycardia, atrial fibrillation
- Fine tremors.
Q.70. A 55 year old man with a history of type 2 diabetes mellitus has been on a trial of lifestyle modifications for the past 3 months. He is not on any medications for his diabetes. He attends his GP surgery for his recent blood results which show: Fasting blood glucose 12.3 mmol/L eGFR 28 He has a BMI of 33. What is the most appropriate treatment to introduce?
Correct Answer : D
The method to answer this question is by going through the answers one by one. Guidelines recommends biguanide (such as metformin) as first-line treatment for patients with type 2 diabetes unless this is contraindicated. Contraindications to metformin include eGFR less than 30 ml/min which is seen in this stem. Sulphonylurea should not be used in renal impairment as there is a risk of hypoglycaemia. Furthermore, this patient has a high BMI.
Sulphonylurea are known to cause weight gain which would not be suitable for this patient. DPP-4 inhibitors are suitable choices among the options. They are weight-neutral and would not cause weight gain.
Alpha-glucosidase inhibitors such as acarbose are used when other oral glucose-lowering medications cannot be used. It works by delaying the absorption and digestion of sucrose and starch.
Since we could potentially use DPP-4 inhibitors which are considered second line, alpha-glucosidase inhibitors would be the wrong answer.
Q.71. A 23 year old woman presents to the female health clinical with secondary amenorrhoea for a duration of 10 months. Her BMI is 30. She has dark pigmentation on her neck and severe acne on her face. She complains of feeling weak and lethargic. Blood tests reveal a serum potassium level of 2.5 mmol/L. What is the most likely diagnosis?
Correct Answer : C
This is a seemingly difficult question because there are lots of conditions that fit this patient’s signs and symptoms. However, in a question like this where you have doubts, look at the clincher in the stem that offers a definitive result. In this question, it is the potassium level. There are many causes of a low potassium level but the two that are considered in this question are Cushing’s syndrome and hyperaldosteronism.
Patients with hyperaldosteronism often present with complaints of polyuria and polydipsia in addition to headaches and lethargy. Upon further investigation, hypertension and hypokalemia will be discovered. Hyperaldosteronism does not present with menstrual abnormalities or an increase in BMI therefore is not the answer.
Q.72. A 6 week old male baby attends the emergency department appearing extremely unwell. Mucous membranes are dry on examintion with sunken eyes and sunken fontanelles. Skin turgor was reduced. His blood rests show: Sodium 124 mmol/L Potassium 2.8 mmol/L. What is the most appropriate initial management?
Correct Answer : A
In this case, the main clinical concern is the profound dehydration of this poor baby. There are multiple possible causes. The emphasis here is to ensure a safe INITIAL option as these cases will likely be cared for in the neonatal intensive care unit. The possible causes include sepsis and diabetic ketoacidosis.
Option A 0.9% sodium chloride with potassium chloride is the correct answer here as it is the safest option and addresses the potassium disturbance.
Option B. 7.5% sodium chloride is incorrect for the same reason as option C.
Option C 0.45% sodium chloride is incorrect as at the level you are expected to be working, you would never be in a position to start this.
Option D. 10% dextrose is incorrect for the same reason as 5% dextrose.
5% dextrose is incorrect as this would likely worsen the electrolyte disturbance by diluting the intravascular space from further electrolytes. Furthermore, if there is diabetic ketoacidosis going on then extra glucose will make this much worse.
Q.73. A 45 year old lady complains of milk discharge from her nipples over the past 2 days. She has been having a low sex drive over the past few months which she finds extremely abnormal. Further history reveals weight gain, low moods and fatigue which have been on going for he past year. Her last menstrual cycle was 2 months ago however, she is not concerned as she has been having irregular cycles for the past 2 years. She takes lactulose for constipation. Her serum prolactin levels are 285 mU/L. What is the most likely cause of her hyperprolactinaemia?
Correct Answer : C
Hypothyroidism can cause hyperprolactinemia and one of the symptoms is galactorrhoea and irregular menstrual periods.
Hypothyroidism would explain her symptoms of weight gain, depression, and constipation. The mechanism of hypothyroidism causing hyperprolactinemia is unclear but research points to thyrotropin-releasing hormone (TRH) being a factor as the overproduction of TRH (due to loss of thyroxine feedback inhibition) would result in secondary pituitary enlargement.
Treating the hypothyroidism often resolves the hyperprolactinemia.
Q.74. A 44 year old man is extremely thirsty despite excessive drinking. Diabetes mellitus and renal failure has been ruled out and a diagnosis of diabetes insipidus is suspected. Fluid deprivation test and an assessment of response to vasopressin was done which was consistent with central diabetes insipidus. What is the most likely laboratory finding that lead to the conclusion?
Correct Answer : A
In diabetes insipidus, one can expect excess fluid loss with urine. Urine osmolality would be low and plasma osmolality would be high. After administration of vasopressin (desmopressin), an increase in urine osmolality is diagnostic for central (cranial) diabetes insipidus.
Q.75. A 45 year old lady presents with diarrhea, vomiting, and severe abdominal pain. Examination reveals that her skin is hyperpigmented. Her blood pressure is 70/55 mmHg. What is the most likely electrolyte abnormality to be found?
Correct Answer : D
Diarrhoea, vomiting, severe abdominal pain, tanned skin (hyperpigmentation), and hypotension point towards Addison’s disease where hyponatremia and hyperkalemia are seen.
Q.76. A 29 year old lady comes to the emergency department with complaints of palpitations, and excessive sweating that has been present for the past 4 days. She also feels warmer than usual. Her heart rate is 154 bpm and has an irregular rhythm. Her temperature is 38.7°C. What is the most appropriate management?
Correct Answer : B
From the symptoms, this patient is likely having a thyroid storm. She is having atrial fibrillation secondary to thyrotoxicosis. Thyroid crisis represents a rare, but life-threatening, exacerbation of the manifestations of thyrotoxicosis.
B-adrenergic blocking agents are essential in the management control of tachycardia, tremor, and other adrenergic manifestations.
Propranolol in divided doses or as an infusion would be given.
Manifestations of hyperthyroidism (all forms)
Symptoms :
• Hyperactivity, irritability, altered mood, insomnia
• Heat intolerance, sweating
• Palpitations
• Fatigue, weakness
• Dyspnoea
• Weight loss with increased appetite
• Pruritus
• Increase stool frequency
• Thirst and polyuria
• Oligomenorrhoea or amenorrhoea, loss of libido, erectile dysfunction
Signs :
• Sinus tachycardia, atrial fibrillation
• Fine tremor, hyperreflexia
• Warm, moist skin
• Palmar erythema
• Hair loss
• Muscle weakness and wasting.
Q.77. A 28 year old female comes in to clinic complaining of a lump on her anterior neck which she has noticed 2 weeks ago. She has difficulty swallowing over the past few weeks. The lump is felt to be hard and it is not tender on palpation. The lump is about 2 cm in size. The lump moves upwards on protrusion of tongue. What is the most appropriate investigation to perform?
Correct Answer : A
Fine-needle aspiration cytology (FNAC) should be performed in any thyroid nodule that is 1 cm and larger.
FNAC is very sensitive for the differential diagnosis of benign and malignant thyroid nodules. Radionuclide imaging and MRI scans also have a role in the investigations of thyroid carcinoma but they should not be used to diagnose cancer.
Investigations usually start with a thyroid ultrasound as they are extremely sensitive to thyroid nodules. This would follow FNAC if there is suspicion of thyroid cancer.
Q.78. A 9 year old boy during operation and immediately after showed glycosuria. A day later his urinalysis was normal. What is the most likely diagnosis?
Correct Answer : D
Glycosuria is fairly common after an operation. Stress during operation can cause transient hyperglycaemia causing glycosuria secondary to the stress-induced rise of cortisol which becomes normal after some time.
Q.79. A 55 year old woman has recently been diagnosed with type 2 diabetes mellitus. Her body mass index is 23 kg/m2. Her last two random blood sugars that were taken were 8 and 7 mmol/L. Her blood pressure is 140/86 mmHg. Her total cholesterol is 4.7 mmol/l. She has no symptoms but has microalbuminuria. What is the most appropriate drug management?
Correct Answer : C
Patients with type 2 diabetes mellitus have a considerably higher risk of cardiovascular morbidity and mortality and are disproportionately affected by cardiovascular disease.
Thus they have a different set of rules when it comes to managing their hypertension. Provide lifestyle advice if blood pressure is confirmed as being consistently above 140/80 mmHg (or above 130/80 mmHg if there is nephropathy, retinopathy, or cerebrovascular damage).
If lifestyle advice does not reduce blood pressure to below these targets, add a drug treatment. First-line antihypertensive drug treatment should be a once-daily ACE inhibitor. This applies to most people.
Q.80. A 46 year old woman complains of tiredness and lethargy. She has noticed a 8 kg weight gain in the last 3 months and is feeling more sensitivity to cold. She has a pulse rate of 55 beats/minute. What is the most likely diagnosis?
Correct Answer : A
Please see Q -12
Q.81. A 39 year old lady presents with gradually worsening headaches, visual disturbance, and lack of energy. MRI shows a 15 mm tumour in the pituitary fossa. She has been on cabergoline treatment for her prolactinoma but has not had any response. What is most appropriate management?
Correct Answer : B
Since dopamine agonists here have been shown to be ineffective, transsphenoidal surgery is appropriate.
Q.82. A 32 year old man has been repeatedly admitted to the hospital for what was described as anxity or panic attacks associated with palpitations. On occasions he is found to be hypertensive and tremulous. What is the most likely diagnosis?
Correct Answer : D
Please see Q-5
Q.83. A 32 year old man has recently had an appendectomy performed. His post-op blood results return with the following values: Glucose 4.5 mmol/L Sodium 129 mmol/L Potassium 5.3 mmol/L. What is the most appropriate management?
Correct Answer : D
There is mild mild hyponatremia with normal to mild hyperkalemia. Glucose is within normal levels. The range for “normal” potassium differs among laboratories but they are usually between 3.5-5.0 mmol/l. There is no universal definition of hyperkalemia but a serum potassium above 5.5mmol/l is widely used.
It is worth knowing the contents of sodium chloride 0.9%. One litre of sodium chloride 0.9% contains:
• 154 mEq of sodium ion = 154 mmol/L .
• 154 mEq of chloride ion = 154 mmol/L
Thus, sodium chloride 0.9% intravenous infusion can be used to treat sodium depletion and in this case, it will correct the electrolyte disbalance. Potassium levels will also be brought down slightly with sodium chloride 0.9% intravenous infusion.
Nebulized salbutamol, insulin-glucose intravenous infusion, and sodium bicarbonate are used in the management of moderate to severe hyperkalemia (usually with potassium values ranging from above 6 mmol/L).
Q.84. A 19 year old man presents with weight loss, increasing thirst and increasing frequency of going to the washroom. His father, grandfather and his 2 sisters have been diagnosed with diabetes mellitus. What is the most likely type of diabetes this man suffers from?
Correct Answer : B
MODY is a rare form of diabetes that is different from both Type 1 and Type 2 diabetes and runs strongly in families. Maturity onset diabetes of the young is estimated to be the underlying cause in 0.5–1% of all patients with diabetes. A typical ‘MODY patient’ has a young age of onset. The need to know so much detail for MODY is not necessary in. But there are three key features that one needs to know :
1. Being young - diagnosed with diabetes under the age of 25
2. Having a strong family history. E.g. a parent with diabetes, with diabetes in two or more generations
3. Manifest as mild hyperglycemia.
Q.85. A 42 year old woman complains of tingling, numbness, paraesthesia, and involuntary spasm of the upper extremities. She has undergone a thyroidectomy for thyroid carcinoma a week ago. What is most likely diagnosis?
Correct Answer : D
Hypoparathyroidism is one of the well-known causes of hypocalcemia. It is seen especially after thyroid surgeries where the surgeon has to work in close proximity to the parathyroid gland.
Q.86. A 35 year old man with a medical history of type 1 diabetes mellitus presents to the hospital with reduced conscious level and feeling unwell. He has dry mucous membranes and a slow capillary refill. He has a blood pressure of 80/50 mmHg and a pulse rate of 105 beats/minute. What is the most appopriate initial investigation?
Correct Answer : A
Signs of dehydration, hypotension, and tachycardia with a medical history of type 1 diabetes mellitus point towards a likely diagnosis of diabetic ketoacidosis. In reality, diabetic ketoacidosis should be part of the differential in anyone with diabetes who is unwell.
From the given options, arterial blood gas is the best response as it would help the medics know the severity of the DKA. If capillary blood glucose was in the options, this would take priority over the other investigations as it is quick and helps us with the differential.
Q.87. A 44 year old woman has recently undergone surgery for a fractured left hip. Her blood tests show a low serum calcium level, low serum phosphate level and raised alkaline phosphatase. What is the most likely diagnosis?
Correct Answer : C
Please see Q-11
Q.88. A 63 year old diabetic patient on oral hypoglycaemics complains of diarrhoea for the past 3 months. His blood sugar levels have been poorly controlled. He has not changed his diabetic medications for the past year. What is the most likely cause for his diarrhoea?
Correct Answer : D
One of the established complications of diabetes mellitus is autonomic neuropathy. Autonomic neuropathy, as the name suggests, affects the autonomic nervous system of both the sympathetic and parasympathetic branches. Diabetes mellitus is a known cause, as is normal aging, alcoholism as well as a whole host of other disease processes that are not specific for the exam.
Autonomic neuropathy can present with:
• Sweating
• Constipation
• Diarrhoea
• Incontinence
The question is fairly straightforward.
There is nothing in the stem to hint at any of the other answer choices. Another way the stem could have been spun is if the patient had recently started on metformin. Remember, one of the common side effects of metformin is diarrhoea. If the patient did start to have diarrhoea on metformin, his doctor would need to review his medications.
Q.89. A 62 year old man presents with symptoms of polyuria and polydipsia. His past medical history is significant for lung cancer, which is now in remission. His blood results show: Urea 6.2 mmol/L Creatinine 182 micromol/L Serum calcium (corrected) 3.0 mmol/L What is the next appropriate biochemical investigation?
Correct Answer : A
We need to dissect this question step by step. Firstly, the diagnosis is quite obviously hypercalcemia. This patient’s hypercalcemia is probably a result of his malignancy. It is not important to understand the mechanism of his hypercalcemia for this question.
Secondly, the examiners have given you a raised corrected calcium level of 3.0 mmol/L. This is important because one needs to follow the following investigative steps. What do we do when we suspect hypercalcemia?
1. Correct calcium level
2. Check albumin: corrected calcium + albumin + urea
3. Check alkaline phosphatase: corrected calcium + ALP = bony metastases, sarcoidosis, or thyrotoxicosis
4. Check serum calcitonin level: corrected calcium + serum calcitonin = B-cell lymphoma.
According to the above, the next investigative step is to do a serum alkaline phosphatase for this patient.
Q.90. A 24 year old man is admitted to the emergency department with abdominal pain and vomiting. He is discovered to have diabetic ketoacidosis. What is the most appropriate immediate management?
Correct Answer : B
It is clear in this question that this man is suffering from diabetic ketoacidosis. Most DKA patients have a depletion of around 5 litres thus initial intravenous normal saline is very important. 0.9% saline is the replacement fluid of choice. Insulin should be infused continuously at 0.1 u/kg/h. Only give a stat dose of insulin if there is a delay in starting the insulin infusion.
Q.91. A 58 year old man who is known to have diabetes mellitus presents to the hospital with drowsiness, blurred vision, tremors, fatigue and confusion. On examination, he is excessively sweaty. Which investigations should be done initially to help with further management?
Correct Answer : D
It is clear in this question that this man is having a hypoglycemic episode. This could be caused by a missed meal or increased activity. The first step should be attaining blood sugars. This does not need to be fasting blood sugars.
Q.92. An 8 month old infant presents with failure to thrive and constipation. On examination, a protruding tongue and widely set eyes are observed. His father and older sister has a history of prolonged neonatal jaundice. What is the most likely diagnosis?
Correct Answer : C
Failure to thrive, constipation, protruding tongue, and widely set eyes are consistent with congenital hypothyroidism. Firstly, routine screening for congenital hypothyroidism is available.
Thyroid-stimulating hormone (TSH) analysis is performed on a single spot from the initial dried blood sample. Screening for congenital hypothyroidism is part of the newborn blood spot test which is offered when the baby is 6 to 8 weeks old.
So it would be unlikely that congenital hypothyroidism would go undiagnosed until the 8 months of life. The reason for the family history of prolonged neonatal jaundice is that 15% of congenital hypothyroidism is caused by thyroid dyshormonogenesis defects transmitted by an autosomal recessive mode of inheritance.
Thyroid hormone dysgenesis is caused by inborn errors in thyroid metabolism.
Congenital hypothyroidism clinical features :
• Physiological jaundice
• Goitre
• Feeding problems, constipation
• Delay in reaching normal milestones of development, short stature
• Coarse features with protruding tongue, broad flat nose, widely set eyes
• Sparse hair and dry skin
• Impaired mental development
Q.93. A 55 year old man with a 4 year history of feeling thirsty and urinating more often than usual presents with a deep painless ulcer on the heel. He also has a history of unexplained weight loss and feels tired all the time. What is the most appropriate investigation?
Correct Answer : B
The patient has a diabetic foot.
Polydipsia, polyuria, fatigue, and unexplained weight loss are symptoms of diabetes. Blood sugars would be the best investigation of choice.
The main symptoms which are common in diabetes are:
• urinating more often than usual, particularly at night
• feeling very thirsty
• feeling very tired
• unexplained weight loss
• itching around the penis or vagina, or frequent episodes of thrush
• cuts or wounds that heal slowly
• blurred vision (caused by the lens of the eye becoming dry).
Q.94. A 45 year old man presents with bitemporal hemianopia and swelling of his hands. He says that his nose has become larger and his voice has become more hoarse. On examination, spade-like hands are seen. What is the most definitive test to confirm the diagnosis?
Correct Answer : B
The clinical symptoms along with the spare-like hands give the suspicion of acromegaly.
Investigations - Growth hormone (GH) levels tend to vary during the day and are therefore unreliable and not recommended.
The best initial test is Insulin-like growth factor.
• It is used as a screening test and occasionally used to monitor disease. The most definitive test is oral glucose tolerance (OGTT) with serial growth hormone measurements.
• In normal patients, growth hormone is usually suppressed with glucose.
• In acromegaly, there is no suppression of growth hormone with glucose.
MRI scan of the pituitary may show a tumour. MRI scan of the pituitary is more sensitive than CT scan.
Q.95. A 41 year old known type 1 diabetic on insulin is brought in by the paramedics to the Emergency Department. She was found unconscious on the floor by her son. She was found to have a capillary blood glucose of 1.8 mmol/L by the paramedics and was administered glucagon intramuscularly. She has a Glasgow Coma Scale of 3. The anaesthetist is present to secure her airways. What is the most appropriate medication to administer?
Correct Answer : D
The most likely cause of her hypoglycemia is an insulin overdose. She should be managed like any other hypoglycaemic patient. Since she is unconscious, the most appropriate medication to administer would be intravenous glucose.
Q.96. A 58 year old woman has tiredness and diarrhoea for the last few weeks. She has noticed that her skin looks tanned. She describes dizziness on standing up and recently started feeling nauseous. What is the most likely electrolyte abnormality to be found?
Correct Answer : A
Diarrhoea, nausea, tanned skin (hyperpigmentation), and postural hypotension in a tired woman points towards Addison’s disease where hyponatremia and hyperkalaemia are seen.
Q.97. 33 year old woman complains of tiredness, lethargy and constipation. On inspection, she has a dry coarse skin, hair loss and cold peripheries. What is the most likely diagnosis?
Correct Answer : D
Please see Q-12
Q.98. A 70 year old man has polyuria and polydipsia. His last two random blood sugar levels were 8 and 9 mmol/L. His blood results show a cholesterol level of 5.8. He has a blood pressure of 135/80 mmHg. He is also noted to have microalbuminuria seen on his urine test. His regular medications include metformin. What is the most appropriate medications to be added on?
Correct Answer : D
This patient likely has type 2 diabetes mellitus. He would be at a higher risk of cardiovascular morbidity and mortality and so a different set of rules apply when managing his hypertension. As his blood pressure is above 130/80 and there is microalbuminuria which is an early sign of kidney damage, an ACE inhibitor would be indicated to slow the progression of kidney disease and reduce the blood pressure.
As he is also having high cholesterol, statins may be added to his drug regimen.
Smoking status and the ratio of total serum cholesterol to high-density lipoprotein cholesterol together with body mass index, ethnicity, measures of deprivation, family history, chronic kidney disease, rheumatoid arthritis, atrial fibrillation, diabetes mellitus, and antihypertensive treatment.
NICE strongly recommends using a Q RISK score when considering starting statins.
Q.99. A type 2 diabetes mellitus is undergoing a major surgery. He is on long acting insulin and gliclazide. What is the most appropriate pre-operative management?
Correct Answer : C
Management of the diabetic patient pre-op :
• Clarify if the patient is oral-controlled, insulin-dependent or brittle insulin-dependent
• Diabetics should be first on operating lists to ensure timings can be as predictable as possible for blood sugar management.
Minor surgery -
• Oral-controlled: Give a normal regimen.
• Insulin-controlled: Omit preoperative insulin on the day of surgery; monitor blood sugar (BS) every 4 hours; restart normal insulin once the oral diet is established.
Major surgery -
• Oral-controlled: Omit long-acting hypoglycaemics preoperatively. Monitor BS every 4 hours.
• Insulin-controlled: Commence on IV insulin sliding scale preoperatively once nil by mouth (NBM) and continue until a normal diet is re-established. Check BS every 4 hours.
Q.100. A 40 year old man complains of thirst and lethargy. He has a blood pressure of 145/95 mmHg. His blood tests show: Serum calcium 3.5 mmol/l Serum potassium 4.5 mmol/l Serum sodium 149 mmol/l. What is the most appropriate initial management?
Correct Answer : A
The first step in the management of hypercalcemia is always rehydration with IV fluids. The given scenario has a slightly high BP. This can be found in hypercalcemia as well.
Q.101. A 74 year old man with a 6 month history of weight loss and worsening cough. He is a chronic smoker, with a 60 pack-year history. He is brougth to the Accident & Emergency department following a fall and confusion. Which electrolyte imbalance is most likely to be found?
Correct Answer : B
This patient most likely has a primary lung malignancy. Small cell lung cancer can produce large amounts of ectopic anti-diuretic hormone (ADH) leading to SIADH.
This in turn leads to hyponatremia, low serum osmolality, and high urine osmolality. The fact that you are given the choice of both hyponatremia and hyperkalemia suggests this is not an adrenal cause (as these are both seen in adrenal insufficiency).
Lung cancer can metastasize to the adrenals but rarely leads to adrenal insufficiency. Adrenal insufficiency in the exam is usually suggested by a postural drop or hypoglycemia.
Q.102. A 33 year old man has attended the GP surgery as he started having white discharge from his nipples yesterday. He states that he has been having difficulty having sexual intercourse with his partner but refuses to describe the problem further. What is the most likely diagnosis?
Correct Answer : C
Galactorrhoea is always a worry for man. In this case, it is due to excessive prolactin. His problems with sexual intercourse are likely related to a lack of libido and erectile dysfunction seen in hyperprolactinemia.
Q.103. A 45 year old man was scheduled for an elective hernioplasty to be done as a day case procedure. His past medical history includes non-insulin dependent diabetes mellitus diagnosed a year ago. He was advised to try diet and lifestyle modifications first and the patient claims to be following a strict diet and exercise regimen. He is not on any medication. His current body mass index (BMI) is recorded to be 23 kg/m2. He was approved for surgery and the hernioplasty was carried out successfully. Three days following the surgery, he was seen by his GP for a routine diabetic follow up. His blood results show: Fastng blood sugar 8 mmol/L (3.5-5.5 mmol/L) Random blood sugar 11 mmol/L (5.0-9.0 mmol/L) HbA1c 60 mmol/mol (below 42 mmol/mol) Urinalysis was negative for glucose and ketones A renal function test was also carried out and the values were found to be within normal limits. What is the next best step in the management of this patient?
Correct Answer : D
Any surgical procedure induces significant neuroendocrine stress. This results in increased insulin resistance and consequent hyperglycemia however you would not expect the hyperglycemia to last for three days. Furthermore, HbA1c represents the overall picture of his glycemic control over the past three months. This is because RBCs survive for three months. Since his HbA1c is high, his average level of glucose during the last three months would be high.
This patient has already attempted lifestyle modification, and while his body mass index (BMI) appears to be within range, his HbA1c is simply too high to allow him to continue with lifestyle modifications alone. Sulfonylureas and thiazolidinediones are suitable for patients in whom metformin is contraindicated or not tolerated.
They can also be used as dual or triple therapy for patients in whom monotherapy with metformin has failed. Insulin is the last option in managing type 2 diabetes mellitus and is only to be considered if all other measures do not keep the HbA1c below 59 mmol/L.
Q.104. A 52 year old male presents to his GP with the complaint of numbness in his lower limbs. He first noticed it in the toes and then on the soles of the feet. It eventually spread to his mid-shin in a symmetrical fashion. He also has the sensation of pins and needles in his hands. His wife persuaded him to visit a doctor after he sustained first degree burns on his feet in the bath due to him being unable to tell if the water was hot enough or not. The patient’s past medical history is significant for non-insulin diabetes mellitus diagnosed ten years ago. He claims to be taking his medication regularly but admits that his glycaemic control is not very good. Physical examination reveals a glove and stocking loss of fine touch and pain bilaterally in his feet. Power and tone are globally intact, and further neurological examination of his limbs reveals no other abnormalities other than a loss of the ankle jerk reflex bilaterally. What is the most likely cause of this patient’s signs and symptoms?
Correct Answer : B
The patient has diabetic neuropathy.
Diabetic neuropathy describes any disorder that damages the nerves in diabetic patients. They are caused by microvascular injury. Symptoms are predominantly sensory peripheral neuropathy that begins in the toes and spreads upwards. In severe cases, like this one, fingers and hands are involved. Absent ankle reflexes are amongst the first features to be seen.
Q.105. A 44-year-old woman has lost weight over 12 months. She has also noticed episodes where her heart beats rapidly and strongly. She has a regular pulse rate of 90 bpm. Her ECG shows sinus rhythm. What is the most appropriate investigation to be done?
Correct Answer : B
This is a probable case of thyrotoxicosis. The patient has paroxysmal atrial fibrillation.
That is why there is no arrhythmia in between attacks. From the given option TFT is the appropriate test as thyrotoxicosis is a leading cause of paroxysmal atrial fibrillation and thyrotoxicosis is the probable cause of weight loss of this lady.
Q.106. A 45-year-old type1 diabetes mellitus patient had an annual checkup. Ophthalmoscopy showed dot and blot hemorrhage, hard exudate and multiple cotton wool spots. What is the next step in management?
Correct Answer : D
Non-urgent referral to an ophthalmologist.
Controlling diabetes and maintaining the HbA1c level in the 6-7% range are the goals in the optimal management of diabetes and diabetic retinopathy. If the levels are maintained, then the progression of diabetic retinopathy is reduced substantially.
Dot and blot hemorrhage + hard exudate and multiple cotton wool spots indicate this is pre-proliferative retinopathy. So non-urgent referral to an ophthalmologist should be done. If proliferative retinopathy (with neovascularization) urgent referral is indicated.
Q.107. A 38-year-old patient presented with tingling, numbness, paraesthesia, respiratory stridor and involuntary spasm of the upper extremities. She has undergone surgery for thyroid carcinoma a week ago. What is the most likely diagnosis?
Correct Answer : D
Hypocalcaemia may be due to accidental parathyroid gland removal during thyroidectomy. Tingling, numbness, paraesthesia, and involuntary spasms of the upper extremities are well-known features of hypocalcemia.
Laryngospasm is also a feature in hypocalcaemia which may cause stridor.
Q.108. A 44-year-old patient has sudden onset of breathlessness and stridor few minutes after extubation for thyroidectomy. The patient had longstanding goiter for which he had the surgery. What is the most likely diagnosis?
Correct Answer : D
Tracheomalacia is a process characterized by flaccidity of the supporting tracheal cartilage, widening of the posterior membranous wall, and reduced anterior-posterior airway caliber. These factors cause tracheal collapse, especially during times of increased airflow, such as coughing, crying, or feeding.
Prolonged pressure over the trachea by goiter is a cause of tracheomalacia and symptoms become evident following thryroidectomy.
Q.109. A 54-year-old woman has presented with episodes of abdominal ache, vomiting and postural hypotension. She also has a dark pigmentation of her skin. A diagnosis of Addison’s disease was made. What is the most likely electrolyte abnormality expected in this patient?
Correct Answer : B
Low Na+, High K+.
In Addison's disease, the sodium, chloride, and carbon dioxide levels are often low, while the potassium level is high.
Q.110. An elderly patient who is known to have DM presents to the hospital with drowsiness, tremors and confusion. What investigation should be done to help in further management?
Correct Answer : A
Blood sugar
Q.111. A 34-year-old woman is referred to the endocrine clinic with a history of thyrotoxicosis. At her 1st appointment she is found to have a smooth goiter, lid lag and bilateral exophthalmos with puffy eyelids and conjunctival injection. She wants to discuss the treatment of her thyroid problem as she is keen to become pregnant. What is the most likely treatment you would advise?
Correct Answer : B
18 months of PTU (propylthyouracil) alone.
Another drug option i.e. Carbimazole is teratogenic.
It can cause :
i. spina bifida
ii. cardiovascular malformations
iii. hypospadias
If become pregnant. PTU is on the other hand relatively safe in pregnancy.
Q.112. A 29-year-old woman presents to her GP with a history of weight loss, heat intolerance, poor concentration and palpitations. Which of the following is most likely to be associated with diagnosis of thyroiditis associated with viral infection?
Correct Answer : C
The diagnosis is De Quervain’s or subacute thyroiditis.
Diagnostic criteria:
i) Features of hyperthyroidism present.
ii) Pain thyroid (not mentioned in given question)
iii) Investigations: high ESR (60-100) (not mentioned in given question)
Reduced uptake of radioactive iodine by the gland.
Q.113. A 67-year-old male presents with polyuria and nocturia. His BMI 33, urine culture negative for nitrates. What is the next diagnostic investigation?
Correct Answer : D
Age at presentation and class 1 obesity favours the diagnosis of type 2 DM.
Q.114. A 29-year-old lady came to the ED with complaints of palpitations that have been there for the past 4 days and also feeling warmer than usual. Examination: HR 154bpm, irregular rhythm. What is the treatment for her condition?
Correct Answer : B
The probable arrhythmia is AF secondary to thyrotoxicosis.
Some of the symptoms of hyperthyroidism such as tremors and palpitations, which are caused by excess thyroid hormone acting on the cardiac and nervous system can be improved within several hours by beta-blockers. So to rapidly control the symptoms of thyrotoxicosis beta blocker should be used which will improve the arrhythmia as well.
Q.115. A 60-year-old man with a 4 years history of thirst, urinary frequency and weight loss presents with a deep painless ulcer on the heel. What is the most appropriate investigation?
Correct Answer : C
The patient probably developed diabetic foot.
Q.116. A patient presents with weight loss of 5kgs despite good appetite. He also complains of palpitations, sweating and diarrhea. He has a lump in front of his neck which moves on swallowing. What is the most appropriate diagnosis?
Correct Answer : D
Goitre
Q.117. A 45-year-old man with colon cancer now develops increased thirst, increased frequency in urination and weight loss. His fasting blood glucose 9mmol/L. what is the most appropriate management?
Correct Answer : A
Increased thirst and increased frequency in urination along with weight loss are suggestive of DM supported by a fasting blood glucose of 9 mmol/L. At the age of 45 most likely type of diabetes is NIDDM or type 2 DM which is treated by oral hypoglycemic agents.
Q.118. A 60-year-old diabetic patient on anti-diabetic medication developed diarrhea. What is the most likely cause for his diarrhea?
Correct Answer : A
In autonomic neuropathy diarrhea can occur when the nerves that control the small intestine are damaged. The diarrhea occurs most often at night.
Q.119. A 79-year-old woman has been diagnosed with T2DM. Her BMI is 22. RBS are 8 and 10mmol/l. HerBP is 130/80mmHg. Her fasting cholesterol is 5.7mmol/l. She is currently symptom-free but hasmicroalbuminuria. What is the most appropriate drug management?
Correct Answer : C
Diabetic patients are advocated statin irrespective of cholesterol levels and diabetic microalbuminuria is best treated by ACEI. Initially, we shall give lifestyle advice to a symptom-free patient and no medicine for diabetes, even then we shall start with statin and ACEI.
Q.120. A 46-year-old woman has weight gain, sensitivity to cold, pulse 50bpm, heart is enlarged with murmur. What is the most likely diagnosis?
Correct Answer : A
The given symptoms like weight gain, cold intolerance, bradycardia and enlargement of the heart are well-known presentations of hypothyroidism.
Q.121. A 27-year-old woman with anxiety and weight loss has tachycardia, tremor and mild proptosis. What mechanism accounts for her weight loss?
Correct Answer : C
The given features are of thyrotoxicosis in which increased metabolism causes loss of patient's weight.
Q.122. A 19-year-old man presents with weight loss, increasing thirst and increasing frequency of going to the washroom. His father, grandfather and 2 sisters have been diagnosed with DM. What is the most likely type of DM this patient suffers from?
Correct Answer : D
Key features of MODY are: Being diagnosed with diabetes under the age of 25 and having a parent with diabetes, with diabetes in two or more generations.
Q.123. A 60-year-old diabetic lady presents with severe peri-anal pain and swelling. What’s the cause?
Correct Answer : D
Anal abscess. Diabetes predisposes infection to occur easily.
Q.124. A 60-year-old woman has tiredness. She has noticed that her skin looks permenantly tanned and she describes dizziness on standing up. What is the most likely electrolyte pattern to be found?
Correct Answer : A
Tanned skin (hyperpigmentation) and postural hypotension in a tired woman points towards Addison’s disease where hyponatremia and hyperkalemia is seen.
Q.125. A 43-year-old woman has been feeling lethargic and tired. Her BP is 160/90mmHg. Bloods test: Na+ 140mmol/L, K+ 3.1mmol/L. What is the most likely diagnosis?
Correct Answer : B
Here potassium is < 3.5mmol/L, sodium is at its high normal and hypertension is present.
The most likely diagnosis is Conn's syndrome. Cushing's syndrome is a D/D but it has typical clinical features which is usually described if the question is for Cushing's syndrome. It can also be Cushing’s syndrome!
So if we like to be sure we have to know aldosterone and rennin levels.
i) Renin low, aldosterone high- Conn’s syndrome (primary hyperaldosteronism)
ii) Renin low, aldosterone low- Cushing’s syndrome
iii) Renin high, aldosterone high- Renovascular disease (secondary hyperaldosteronism)
Q.126. A 68-year-old man with diabetes mellitus and hypertension was noted to have cholesterol level of 3.4mmol/l. He was also noted to have microalbuminuria. What is the best drug to add to his regimen?
Correct Answer : A
ACEI is renoprotective and prevents progression in albuminuria.
Q.127. A female patient with hypertension and serum K+2.7mmol/l. Which hormone would you be looking for?
Correct Answer : A
Hypertension and hypokalemia are seen in hyperaldosteronism. So we should look for aldosterone.
Q.128. A 36-year-old male diagnosed with glioblastoma since last 5 months has cerebral edema and is on dexamethasone. He has diarrhea and vomiting for the last 3 days. He has been suffering from repeated falls today. What could be the possible cause for his falls?
Correct Answer : A
Prolonged dexamethasone use suppresses the adrenal axis and intercurrent illness can lead to adrenal insufficiency (Addisonian crisis) in such cases.
Q.129. A 45-year-old lady complains of expressible galactorrhea, decreased libido and amenorrhea, weight gain and easy fatigue. Her serum prolactin levels are 1100um/l. What is the likely cause of hyperprolactinemia?
Correct Answer : D
Given prolactin level of 1100 IU/L is definitely from a microadenoma (in macroadenoma prolactin level is > 10,000 MU/L)
Q.130. A young girl who is known to have T1DM (type 1 diabetes mellitus) presented with drowsiness and deep breathing. Her sugar level 20. Her BP 120/80mmHg and her mucous membranes are dry. What would be the next appropriate step?
Correct Answer : D
Likely diagnosis is DKA where ABG is done to demonstrate acidosis.
Q.131. A known DM was admitted with sudden LOC (loss of consciousness). What is the initial investigation?
Correct Answer : B
In unconsciousness in diabetics, the first glycemic change should be excluded by doing RBS.
Q.132. A patient was admitted with erectile dysfunction, reduced facial hair and galactorrhea. What is the most probable diagnosis?
Correct Answer : A
Erectile dysfunction, reduced facial hair and galactorrhea are common features of hyperprolactinemia.
Q.133. A 32-year-old man has been repeatedly admitted to hospital for what was described as anxiety or panic attacks and palpitations. On occasions he is found to be tremulous and hypertensive. A persistent weight loss is noted. What is the most probable diagnosis?
Correct Answer : C
There is no heat intolerance that goes against hyperthyroidism panic attack and hypertension favours the diagnosis of pheochromocytoma. Weight loss is seen in phaeochromocytoma also. Catecholamine overproduction in pheochromocytoma affects basal metabolism, resulting in weight loss despite normal food intake.
Q.134. A 35-year-old man with type1 diabetes mellitus is dehydrated with BP of 90/50mmHg. What is the most appropriate initial investigation?
Correct Answer : A
Dehydration with low BP points towards probable DKA (diabetic ketoacidosis).
Diabetic ketoacidosis is typically characterized by hyperglycemia over 250 mg/dL, a bicarbonate level less than 18 mEq/L, and a pH less than 7.30, with ketonemia and ketonuria. In patients with DKA, arterial blood gases (ABGs) frequently show typical manifestations of metabolic acidosis, low bicarbonate, and low pH (less than 7.3).
Q.135. In OGTT what is the glucose venous plasma level 2h after glucose intake which indicates impaired glucose tolerance?
Correct Answer : B
Between 7.8-11.0mmol/l
Q.136. A 62-year-old man diagnosed with type 2 diabetes mellitus with BMI 33. Lifestyle modifications have failed to control blood sugar. Laboratory investigations: urea 3.6mmol/l, creatinine 89mmol/l. What is the next appropriate management?
Correct Answer : A
Patient is obese type 2 diabetic. His BMI is >25 (33 here). So biguanide is the treatment of choice.
Q.137. A 68-year-old woman diagnosed with Type2 DM and BMI 33. Laboratory investigations: GFR 29, urea 13, creatinine 390mmol/L. What is the next appropriate management?
Correct Answer : C
Insulin is devoid of significant side effects than Glitazones (like fluid retention). In renal failure, there is reduced GFR and some fluid retention. It is not desirable that glitazone cause more fluid retention by causing oedema. The oral agents that are thought to be relatively safe in patients with nondialysis CKD include short-acting sulfonylureas (eg, glipizide) and repaglinide.
Some clinicians recommend the use of meglitinide repaglinide (starting with a dose of 0.5 mg) for nondialysis CKD patients since these agents are not cleared. Nondialysis CKD patients with type 2 diabetes may be treated with an oral agent, although many patients end up on insulin therapy because it is more effective. So it may be that we can go for insulin as the answer!!
Q.138. An 80-year-old diabetic lady presents with redness and swelling over her right foot. It is tender to touch, warm and glossy. What are the complications this patient might develop?
Correct Answer : B
All options are possible. Sepsis and gangrene are more common.
Q.139. A 44-year-old obese patient with findings: FBS 6mmol/l, OGTT 10mmol/l, 2 hours after 75 g of glucose. What is the most likely diagnosis?
Correct Answer : A
The World Health Organization (WHO) criteria for impaired glucose tolerance (IGT) is an FPG of less than 126 mg/dL (7 mmol/L), if measured, and venous plasma glucose of 140 mg/dL to just below 200 mg/dL (?7.8 to <11.1mmol/L) 2 hours after a 75-g glucose load with one intervening plasma glucose value at or above 200 mg/dL.
Q.140. A 29-year-old woman presents with lid lag, lid retraction and diplopia. What is the most appropriate next step?
Correct Answer : A
Features are suggestive of Grave’s disease hence TFT.
Q.141. A 72-year-old presents with polyuria and polydipsia. The fasting blood sugar is 8 and 10mmol/l. BP 130/80mmHg and the level of cholesterol 5.7mmol/l. There is microalbuminuria. What is the most appropriate next management?
Correct Answer : D
We shall first consider lifestyle modification and if fail then switch to oral anti-diabetics.
Q.142. A-49-year old woman presents to the OPD. Her oral glucose test after 2hours of glucose intake vs plasma level in 2 different tests are 6mmol/l and 10mmol/l. This situation can be categorized as?
Correct Answer : A
The WHO defines someone as having prediabetes if they have: A fasting blood glucose of less than 7 mmol/L; AND A blood glucose of 7.8 mmol/L or more but less than 11.1mmol/L after a two-hour oral glucose tolerance test.
Q.143. A-54-year old male patient of diabetes mellitus with BMI 33 who has been treated using dietary control up till now presents to his GP with a fasting blood sugar of 14mmol/l and creatinine of 90 micro-mol/l. Urine shows glycosuria. No other abnormalities are found. What is the best next step in management?
Correct Answer : A
Patient is obese type 2 diabetic with normal renal function for whom biguanide is the treatment of choice.
Q.144. A diabetic has been prescribed a long acting hypoglycemic in the morning and short acting in the evening. He takes a regular lunch, but has been having hypoglycemic attacks at around 4pm each day. What is the most appropriate intervention?
Correct Answer : B
As there is hypoglycemic attacks at evening, morning dose needs to be adjusted.
Q.145. A 34-year-old woman presents with truncal obesity, easy bruising, hyperglycemia, high BP and depression. Which of the following investigation will be most helpful in localizing the cause for Cushing’s syndrome?
Correct Answer : C
High dose dexamethasone suppression test can identify whether pituitary adenoma or ectopic ACTH-producing tumour. Suppression is absent in patients with Cushing syndrome due to ectopic ACTH secretion or adrenal abnormalities. Suppression is present in patients with Cushing disease.
Q.146. A 38-year-old female presents with difficult in looking upward and on examination she was found to have lid lag as well. She also complains of her heart racing at times. Which test will help in diagnosis?
Correct Answer : C
Difficulty in looking upwards is due to superior rectus or inferior oblique palsy and palsy of one or more extra-ocular muscles can occur in thyrotoxicosis which is known as Ballett’s sign. There is lid lag in thyrotoxicosis and a racing heart is due to paroxysmal atrial fibrillation caused by hyperthyroidism.
Q.147. A patient was admitted with abdominal pain, diarrhea, pigmented palmar creases and buccal mucosa. What is the most probable diagnosis?
Correct Answer : A
Addison's disease, also known as primary adrenal insufficiency and hypocortisolism is a long-term endocrine disorder in which the adrenal glands do not produce enough steroid hormones. Symptoms generally come on slowly and may include abdominal pain, weakness, weight loss, diarrhea, pigmented palmar creases and buccal mucosa.
Q.148. A 45-year-old man presented to his GP with vague symptoms of headache, proximal muscle weakness and nocturia. Test results show him to be severely hypertensive (230/130mmHg) and hypokalemic. What is the most probable diagnosis?
Correct Answer : B
High BP is often the only presentation of Conn’s syndrome. Loss of K+ in urine leads to hypokalemia which in turn causes muscle weakness and polyuria, particularly nocturia.
Q.149. A 35-year-old man with type 1 DM is dehydrated with BP 90/50mmHg. What is the most appropriate initial investigation?
Correct Answer : A
The likely diagnosis is DKA. Among the given options ABG is the most appropriate investigation to demonstrate acidosis.
Q.150. A patient presents with a lid lag, bulging eyes, opthalmoplegia and thyroid bruit. What investigation will you do?
Correct Answer : A
Diagnosis is Grave’s disease. TFT should be done.
Why not FNAC? Thyrotoxicosis is benign and not malignant.
Malignant cells are never hyper functioning.
Q.151. An 18-year-old lady in her 30th week of pregnancy is brought to the hospital in an altered sensorium. She is taking slow, shallow breaths and her breath has a fruity smell. An ABG: pH 7.20, urine ketones: +ve. What is the most probable diagnosis?
Correct Answer : B
Shallow breath and fruity smell with acidosis in ABG and positive ketone body in urine suggests the diagnosis of DKA.
Q.152. A patient presents with skin pigmentation, diarrhea, vomiting, abdominal pain and postural hypotension. What electrolyte abnormality is likely to occur?
Correct Answer : A
Addison's disease is adrenocortical insufficiency due to the destruction or dysfunction of the entire adrenal cortex.
It affects glucocorticoid and mineralocorticoid function. The disease onset usually occurs when 90% or more of both adrenal cortices are dysfunctional or destroyed. Hyperpigmentation of the skin and mucous membranes often precedes all other symptoms by months to years.
Diarrhea, vomiting, abdominal pain, and postural hypotension are well-known features of acute addiction disease.
In Addison’s disease there is low Na+, low Cl-, low CO2, and raised K+.
Q.153. A 56-year-old male who presented with epilepsy like symptoms has been diagnosed with an intracranial space occupying lesion. He now complains of thirst and mild dehydration. His blood glucose is also increased. What is the most appropriate immediate treatment?
Correct Answer : B
This is stress-induced hyperglycemia and does not always need insulin. As dehydration can cause worsening of hyperglycemia our immediate treatment is IV fluid. Later evaluation will be made on whether insulin should be given or not.
Q.154. A 68-year-old lady with type 2 DM. Which drug should be prescribed?
Correct Answer : A
This is an incomplete question and BMI is needed to decide whether biguanide or sulphonylurea be prescribed. If BMI is >25 biguanides should be prescribed and if BMI is <25 sulphonylurea is prescribed.
Q.155. A man with diabetes mellitus comes to the emergency department after he collapsed at home. His GCS is 10. What should be the next initial investigation for this man?
Correct Answer : A
It may be either hypoglycemic or hyperglycemic coma which can be detected by checking capillary blood sugar.
Q.156. A 60-year-old diabetes mellitus patient presented with easy fatigability, weakness and numbness of hands and swollen feet. Examination: pedal edema, sensory neuropathy and palpable liver and spleen. Urine: proteinuria. Ultrasound abdomen: enlarged kidney. Renal biopsy: amorphous homogenous substance that stained green with congo-red. What is the diagnosis?
Correct Answer : C
Islet amyloid is a characteristic pathological finding in patients with type 2 diabetes mellitus, being present in more than 90 percent. Amyloidosis is a common cause of organomegaly. Also in diabetic nephropathy kidneys may be enlarged.
Q.157. A patient was admitted with increased frequency of passing urine, increased thirst, weakness and muscle cramps. What is the most probable diagnosis?
Correct Answer : A
There is hypokalemia in Conn’s syndrome. Increased frequency of passing urine and increased thirst are from nephrogenic DI resulting from hypokalemia and hypokalemia also cause weakness and muscle cramps.
Q.158. A 46-year-old woman has gained weight. She has sensitivity to cold. Her pulse is regular at 50 bpm and heart is enlarged. What is the most likely underlying mechanism for this condition?
Correct Answer : A
The most common cause of hypothyroidism in the developed countries is autoimmune hypothyroidism. In developing countries, it is often nutritional (iodine deficiency). The diagnosis is autoimmune hypothyroidism (in hypothyroidism heart often gets enlarged).
Q.159. A 15-year-old man presents with bitemporal hemianopia and spade-like hands. What is the definite test to confirm the diagnosis?
Correct Answer : C
The bitemporal hemianopia and spade-like hands point towards acromegaly. The best initial test is insulin-like growth factors but the definitive test that confirms the diagnosis is OGTT with serial growth hormone measurements.
Q.160. You suspect Cushing's disease in a 50-year-old woman who has attended clinic with glycosuria, hypertension and a suggestive body habitus. Initial investigations point you towards a diagnosis of Cushing's disease. Which of the following findings would be against this diagnosis?
Correct Answer : C
Unilateral adrenal enlargement.
Cushing’s disease: Bilateral adrenal hyperplasia from an ACTH-secreting pituitary adenoma. Peak age 30-50 years, male-female ratio 1:1. A low dose dexamethasone test leads to no change in plasma cortisol but 8 mg may be enough.
Q.161. A 23-year-old man with type 1 diabetes presents with 48 hours of increasing confusion and breathlessness. His chest is clear and his blood glucose concentration is 28 mmol/L. What is the most appropriate investigation?
Correct Answer : B
In patients with DKA, arterial blood gases (ABGs) frequently show typical manifestations of metabolic acidosis, low bicarbonate, and low pH (less than 7.3).
Q.162. A 35-year-old man is being investigated for infertility. Which of the following tests would prove that he has complete azoospermia?
Correct Answer : C
Low testosterone may lead to azoospermia. But surprisingly testosterone replacement can improve libido but not help azoospermia as it causes follicle-stimulating hormone suppression. So testosterone rise should be done by natural means to improve fertility!.
Choose a Question
×Choose a Question
×
Trial Access Limit Reached
You’ve reached the limit of free content. Subscribe to continue learning without restrictions.