

Hello,
Dr. Batman
Hello Doctor, Welcome!
Profile

Name: Batman
Email: batman@gotham.com
GASTROENTEROLOGY
(Total Questions - 163)Q.1. A 22 year old man presents with a 2 month history of diarrhoea. He says his bowels have not been right for the past few months and he frequently has to run to the toilet. These symptoms seemed to be improving up until two weeks ago and for the past week, he notices the presence of blood when he passes stool. On examination, there are aphthous oral ulcers. He has not lost any weight and has a good appetite. Examination of his abdomen demonstrates mild tenderness in the left lower quadrant but no guarding. What is the most likely diagnosis?
Correct Answer : C
This is most likely ulcerative colitis. Note that aphthous oral ulcers can be seen in both ulcerative colitis and Crohn’s disease. However, commonly, literature would classify aphthous oral ulcers to be a feature seen only in Crohn’s disease. It is also noted that this patient has blood when he passes stools of which the history points towards ulcerative colitis.
CROHN’S DISEASE VS ULCERATIVE COLITIS :
It is important to know the differences between ulcerative colitis and Crohn’s disease as it is very commonly asked.
These are some key differences that will help you with your exam:
Crohn’s disease:
* Usually non bloody
* Abdominal mass palpable in right iliac fossa
* Increased goblet cells on histology
* Granulomas seen on histology
* Weight loss is more prominent
* Transmural, skip lesions, cobblestone appearance on endoscopy.
Ulcerative colitis:
* Bloody diarrhoea is more common
* Abdominal pain in the left lower quadrant
* Decreased goblet cells on histology
* Granulomas are infrequent in histology
* Primary sclerosing cholangitis is more common
* Loss of haustration, drain pipe colon is seen on barium enema.
Q.2. A 65 year old lady had a urinary tract infection which was treated with broad spectrum antibiotics. A few days later she developed bloody diarrhoea and severe abdominal pain. She has a temperature of 38.6 C and a pulse rate of 90 beats/minute. Her blood tests show: Haemoglobin 119 g/L White blood cells 18 x 109/L CRP 180 mg/L What is the most likely management?

Correct Answer : A
This scenario shows a classical picture of Clostridium difficile. Broad-spectrum antibiotics always have the potential to kill off normal gut flora leaving C. Difficile the chance to grow. Metronidazole is usually used as first-line to manage Clostridium difficile. As this is not an option here, use the second line which is vancomycin.
Vancomycin is usually reserved for more severe colitis with severe bloody diarrhoea, severe abdominal pain, and temperatures above 38.5 C. Woman always want a “strong” antibiotic to treat their urinary tract infections but they are not aware that antibiotics such as cephalosporins and amoxicillin are commonly implicated in C. difficile infections.
This is a very good reason why we should always start with narrow-spectrum antibiotics such as trimethoprim and nitrofurantoin for simple urinary tract infections. In the exam, look out for antibiotic usage like cephalosporins, clindamycin, co-amoxiclav, and amoxicillin as a cause for Clostridium difficile.
CLOSTRIDIUM DIFFICILE :
Clostridium difficile is a Gram-positive rod often encountered in hospital practice. It is transmitted via the fecal-oral route by spores that are resistant to antibiotics. It produces an exotoxin which causes intestinal damage leading to a syndrome called pseudomembranous colitis.
Clostridium difficile develops when the normal gut flora is suppressed by broad-spectrum antibiotics.
The most common antibiotics implicated in Clostridium difficile infections are :
• Clindamycin
• Cephalosporins (in particular second and third-generation cephalosporins)
• Quinolones
• Co-amoxiclav
• Aminopenicllins (amoxicillin and ampicillin)
Features :
• Diarrhoea - may be mild diarrhoea or serious bloody diarrhoea
• Abdominal pain – can sometimes be severe enough to mimic an acute abdomen
• Raised white blood cell count
• Fever
Diagnosis : Clostridium difficile toxin (CDT) detected in the stool
Management :
• Stop the causative antibiotic (if possible)
• First-line therapy is oral metronidazole
• If severe or not responding to metronidazole then oral vancomycin may be used. Another method of treating Clostridium difficile is faecal microbial transplantation but we shall not discuss this in case you are about to eat lunch.
Note: Treatment is not usually needed if the patient is asymptomatic.
Q.3. A 25 year old man presents to his GP with the complaint of diarrhoea for the last seven days. Upon further questioning, he reveals that he opens his bowels in excess of two to six times per day. He describes his stool as being watery in consistency. He has also noticed blood in his stool. When asked about the character of the blood, the patient claims that the blood appeared to be fresh and was bright red in colour. He also complains about abdominal pain and describes his pain as being cramping in nature. He complains about an urgency to visit the toilet all the time. The patient is a bank manager by profession and for the last seven days, has been unable to cope with his situation. He says that it is affecting his work and overall general health as he is feeling very tired and lethargic all the time. He also complains about a lack of appetite. He has not traveled outside of the United Kingdom for the last eight months. The patient has no significant past medical history and does not have any allergies. On examination, he has a blood pressure of 120/80 mmHg and a heart rate of 70 beats/minute. His abdomen is tender with no guarding or rigidity. What most appropriate investigation will you perform to aid in the management of this patient?
Correct Answer : D
The World Health Organisation classification of diarrhoea is as follows:
• Diarrhoea > 3 loose or watery stools per day
• Acute diarrhoea < 14 days
• Chronic diarrhoea > 14 days.
According to the above classification, it is too early to decide in this patient if he is suffering from ulcerative colitis or not because he has had diarhoea for only the last seven days. At this stage, it is best to exclude the infectious causes first by doing a stool microscopy, culture, and sensitivity test. In such cases, the investigations largely depend on the clinical setting.
For example, in primary care, the main aim is to make the diagnosis, and in secondary care, to confirm the diagnosis as well as to assess the severity and extent of the disease. In primary care, the test must include a stool culture and sensitivity to exclude the infectious causes of diarrhoea such as salmonella, shigella, escherichia coli, clostridium difficile, campylobacter, and giardiasis. Once the infectious causes are excluded, further diagnostic tests like colonoscopy with biopsy can be done in secondary care.
Faecal test is not the correct option. A faecal fat test is primarily ordered when a person has signs and symptoms of malabsorption such as steatorrhea, persistent diarrhoea, abdominal pain, bloating, weight loss, and failure to thrive (in children) The faecal antigen test is a stool test that is used to detect helicobacter pylori. It is an irrelevant test to perform on this particular patient.
Q.4. A 70 year old man presents with persistent dysphagia to both solids and liquids for a few months now. There is no associated weight loss. He does not have regurgitation after meals. His medical history includes osteoporosis which he takes alendronate once a week for the past 2 years. What is the most likely diagnosis?
Correct Answer : B
Benign oesophageal strictures – are usually the result of scarring from acid reflux in severe and persistent GORD. It may also follow the ingestion of corrosives. While the area heals, a scar forms, causing the tissue to pull and tighten, leading to difficulty in swallowing. Certain drugs like alendronate and NSAIDs have the potential to cause strictures due to their side effects which worsen GORD.
This is seen in this stem where the patient is taking alendronate. This is the reason that it is so important to advise patients not to lie down for at least 30 minutes after taking alendronate as this will help alendronate reach the stomach faster and prevent irritation of the oesophagus.
Oesophageal carcinoma - The absence of any significant weight loss makes oesophageal carcinoma a less likely diagnosis.
However, it is important to note that any cause of dysphagia can essentially cause weight loss. This includes both benign oesophageal stricture and achalasia.
Barrett’s oesophagus - Would also have a long history of gastro-oesophageal reflux which is seen in this stem however, the symptoms of dysphagia are usually occasional rather than persistent.
Pharyngeal pouch - Usually presents with a history of halitosis and regurgitation of undigested food, a sensation of a lump on the throat, and neck bulge.
Achalasia - While the most common feature is dysphagia, regurgitation is a very common feature of achalasia and occurs in around 80-90% of sufferers. Please note that if this stem did not include the history of taking Alendronate, the answer is still likely to be benign oesophageal stricture given that there is less evidence for any other option.
Q.5. A 33 year old woman presents to the emergency department with right upper quadrant pain for the past 7 days. The pain is constant and gradually worsening over the past few days. The pain radiates to the back and is usually seen to be worse after eating meals. She feels nauseous and has vomited twice today. She has no history of any liver or gallbladder disease. On examination, there is no signs of jaundice. On palpation of the right costal margin at the midclavicular line, her breathing is interrupted due to tenderness. She has a temperature of 37.6 C and a heart rate of 90 beats/minute. Her blood results show: Haemoglobin 120 g/L White cell count 13 x 109/L Platelets 350 x 109/L CRP 30 mg/L Amylase 30 U/L Bilirubin 99 micromol/L Alanine transferase (ALT) 189 U/L Albumin 39 g/L What is the most likely diagnosis?
Correct Answer : A
Acute cholecystitis presents with severe continuous right upper quadrant pain which can be seen to radiate to the right flank and back. A fever like in this stem is also associated with it.
Nausea and vomiting are often seen with cholecystitis. Jaundice can be a feature of obstruction of the biliary tract and can be seen in cholecystitis however, it is often mild or not seen unless there is the presence of gallstones in the common bile duct (choledocholithiasis). In this stem, jaundice is absent.
The examination here shows a positive Murphy’s sign. Remember, the Murphy sign is not just pain, but it is the arrest of inspiration when pressing the right costal margin at the midclavicular line. It is a sign of acute cholecystitis.
It is sensitive, but not specific to cholecystitis. There is an elevation of ALP in this stem which ALP rises much higher than ALT which points towards a form of biliary obstruction with cholestasis. The likely scenario here is that there are gallstones that are obstructing the cystic duct causing acute cholecystitis.
Remember, more than 90% of the time, acute cholecystitis occurs from blockage of the cystic duct by a gallstone.
When this occurs, the patient would experience biliary colic. Chronic cholecystitis is incorrect here as chronic cholecystitis occurs when there are repeated episodes of infection causing thickening and fibrosis of the gallbladder. Acute pancreatitis is incorrect as the amylase is within normal limits in this stem.
Acute cholecystitis follows stone or sludge impaction in the neck of the gallbladder, which may cause continuous epigastric or RUQ pain (referred to the right shoulder), vomiting, fever, local peritonism, or a gallbladder mass.
The main difference from biliary colic is the inflammatory component (local peritonism, fever, and elevated WCC). If the stone moves to the common bile duct (CBD), obstructive jaundice and cholangitis may occur Murphy’s sign is positive when you lay 2 fingers over the RUQ and ask the patient to breathe in which causes pain & arrest of inspiration as an inflamed gallbladder impinges on your fingers.
It is only positive if the same test in the LUQ does not cause pain.
Tests: WCC would be elevated.
Ultrasound shows a thick-walled, shrunken gallbladder
Management: Nil by mouth, pain relief, IV fluids, and antibiotics.
Once symptoms settle, do a laparoscopic cholecystectomy.
Laparoscopic cholecystectomy is the treatment of choice for all patients fit for general anaesthesia. Open surgery is required if there is gall bladder perforation.
Q.6. A 28 year old type 1 diabetic has intermittent diarrhoea and abdominal bloating over the last 6 months. He also complains of feeling tired all the time. His blood results show the following: Haemoglobin 135 g/L (130-180 g/L) Ferritin 30 ng/ml (20-300 ng/ml) Thyroid stimulating hormone (TSH) 2.5 mU/L (0.5-5.7 mU/L) Immunoglobulin A (IgA) tissue transglutaminase positive What is the most appropriate next step in action?
Correct Answer : B
There is an association between type 1 diabetes and coeliac disease. The gold standard to diagnose coeliac disease is a jejunal/duodenal biopsy. In the past, small-bowel biopsies for the diagnosis of coeliac disease were taken from the jejunum, but nowadays most gastroenterologists take endoscopic biopsies from the distal duodenum. Coeliac disease is caused by sensitivity to the protein gluten. Repeated exposure leads to villous atrophy which in turn causes malabsorption.
Signs and symptoms :
• Chronic or intermittent diarrhoea
• Stinking stools / steatorrhoea
• Persistent or unexplained gastrointestinal symptoms including bloating, nausea and vomiting
• Fatigue
• Recurrent abdominal pain, cramping or distension
• Sudden or unexpected weight loss
• Unexplained iron, vitamin B12 or folate deficiency.
Note that the one of them a common presentation of coeliac disease is iron deficiency anaemia. Also, folate deficiency is more common than vitamin B12 deficiency in coeliac disease.
Complications -
• Osteoporosis
• T-cell lymphoma of small intestine (rare) Investigation.
Diagnosis is made by a combination of immunology and jejunal biopsy. Any test for coeliac disease is accurate only if a gluten-containing diet is eaten during the diagnostic process. The person should not start a gluten-free diet until the diagnosis is confirmed. If patients are already taking a gluten-free diet they should be asked, if possible, to reintroduce gluten for at least 6 weeks before testing.
Specific auto-antibodies -
• Tissue transglutaminase (TTG) antibodies (IgA) are first-choice.
• Endomysial antibody (IgA)
Jejunal/duodenal biopsy - A biopsy is still needed to diagnose coeliac disease even if antibody tests confirm the diagnosis of coeliac disease. It shows :
• Villous atrophy
• Crypt hyperplasia
• Increase in intraepithelial lymphocytes
Management -
• Gluten-free diet.
Q.7. A 55 year old woman complains of retrosternal chest pain and difficulty swallowing which is intermittent and unpredictable. She says that food gets stuck in the middle of the chest and she has to clear it with a drink of water. She is then able to finish the meal without any further problem. A barium meal shows a ‘corkscrew patterned oesophagus’. What is the most likely cause of the dysphagia?
Correct Answer : C
The corkscrew pattern gives it away. This can only be an oesophageal spasm.
Diffuse Esophageal Spasm (DES) :
Clinical Presentation - These patients present with intermittent chest pain and dysphagia. The pain can simulate that of a myocardial infarction, but it bears no relationship with exertion.
The pain can be precipitated by drinking cold liquids.
Diagnosis - Barium studies may show a "corkscrew" pattern at the time of the spasm. The most accurate test is manometric studies, which will show high-intensity, disorganized contractions. Because the contractions are disorganized, they do not lead to the forward flow of food and peristalsis.
Treatment - Calcium-channel blockers, such as nifedipine, and nitrates.
Q.8. A 36 year old lady has diarrhoea for the last 2 months. She has lost 8 kg in that time period. A colonoscopy was performed which showed fistulas. Perianal fistulas are also noticed. What is the most likely diagnosis?
Correct Answer : B
The diagnosis of Crohn’s disease is quite clear here. Fistulas help differentiate between ulcerative colitis and Crohn’s. Since fistulas are present, it can only be Crohn’s disease.
Q.9. A 33 year old lady who has been traveling around Europe for a few months now returns home with lethargy, abdominal pain, loose watery diarrhoea and bloating. She has lost a few kilograms since coming back from the trip. Her physical examination remains unremarkable with abdominal examination having mild generalized tenderness. What is the most likely organism causing her symptoms?
Correct Answer : B
As the patient has watery diarrhoea instead of bloody diarrhoea, think of giardiasis. Many cases of giardiasis are associated with recent foreign travel. Giardiasis can present as a traveler's diarrhoea with symptoms lasting more than ten days. Symptoms of giardiasis include bloating, flatulence, abdominal pain, loose stool, and explosive diarrhoea. The symptoms may begin after returning from travel and may be associated with weight loss.
Giardiasis can cause both acute and chronic diarrhoea. In this stem, it is likely chronic diarrhoea as there is a history of weight loss.
The clinical features of giardiasis are slightly different compared to campylobacter enteritis.
In campylobacteriosis, clinical features usually include a prodromal illness of headache and myalgia with fevers as high as 40°C.
This is followed by abdominal pains and profuse diarrhoea. The stool is often bloody. The reason many choose campylobacter as the answer is because campylobacter is the most common bacterial cause of infectious intestinal disease. But this is incorrect for this stem.
Important keynotes :
• Campylobacter, Shigella, Salmonella usually cause bloody diarrhoea.
• Giardiasis causes non-bloody diarrhoea
• Giardiasis can cause chronic diarrhoea associated with weight loss
• Campylobacter has a prodrome of headache, myalgia, and fever.
Q.10. A 52 year old man who underwent a partial gastrectomy 10 months ago presents with increasing fatigue. A yellow tinge is noted on his skin and he has a red sore tongue. What is the most likely diagnosis?
Correct Answer : B
Findings on examination for B12 deficiency may include lemon tinge to the skin and glossitis. These findings together with a history of gastric resection whereby malabsorption of B12 could occur, point towards the diagnosis of B12 deficiency.
B12 DEFICIENCY Vitamin B12 is found in meat, fish, and dairy products, but not in plants.
Body stores are sufficient for 4 years. B12 then binds to intrinsic factors in the stomach, and this complex is absorbed in the terminal ileum.
Clinical presentation
• Symptoms are those of chronic anemia, i.e. fatigue, dyspnoea on effort
• Neurological symptoms may also be present ? Classically peripheral paresthesia and disturbances of position and vibration sense
• If uncorrected, the patient may develop subacute combined degeneration of the spinal cord leading to permanent ataxia Causes of B12 deficiency:
• Pernicious anaemia ?Commonest cause. It is due to autoimmune gastric atrophy resulting in a loss of intrinsic factor production required for the absorption of B12.
It is usually associated with other autoimmune problems e.g.hypothyroidism
• Dietary (e.g. vegans)
• Following total gastrectomy
• Ileal disease ? Resection of ileum, Crohn’s disease
• Malabsorption disorders ? Coeliac disease, tropical sprue. One distinction that may help you choose between B12 and folate deficiency is the diet. Good food sources of folate include broccoli, brussels sprouts, asparagus, and peas(basically vegetables). Thus if the given scenario is a vegetarian, it is unlikely that he is suffering from folate deficiency. In that case, pick B12 deficiency. Haematological abnormalities of B12 deficiency
• Macrocytic anaemia and the MCV is usually >110fL
• Hypersegmented neutrophils
• Serum B12 is low Management: Hydroxocobalamin IM.
Q.11. A 55 year old man with no past medical history comes to your office for the evaluation of “difficulty swallowing” foots. He has had this problem for almost a year, and finds it difficult for him to swallow both solids and liquids. A barium meal shows gross dilatation of the oesophagus with a smooth narrowing at the lower end of the oesophagus. What is the most likely diagnosis?
Correct Answer : A
Achalasia is the idiopathic loss of the normal neural structure of the lower oesophageal sphincter. The lower oesophageal sphincter is usually contracted to prevent the acidic gastric contents from refluxing backward into the oesophagus. For swallowing to occur, there is normally a relaxation process of the lower oesophageal sphincter to allow food to pass into the stomach. Inhibitory neurons are stimulated, blocking the impulses that cause constriction. In achalasia, these inhibitory neurons have been lost, as well as the ability to relax the lower oesophageal sphincter.
Presentation:
• Progressive dysphagia to both solids and liquids simultaneously and can have regurgitation several hours after eating
• There can also be weight loss
• Achalasia has no relationship with alcohol or tobacco use
• Note: This is different from oesophageal cancer, which usually not only presents with dysphagia to solid foods that progresses to difficulty swallowing liquids, but also is more common in older patients with a long history of alcohol and tobacco use.
Investigations:
• Barium swallow shows dilation of the esophagus, which narrows into a "bird beak" at the distal end
• The most accurate test overall is esophageal manometry.
Manometry shows increased lower oesophageal resting pressure
Management:
• Dilatation of the lower oesophageal sphincter
Q.12. A 35 year old male presents to his GP with the complaint of diarrhoea. He complains that he has been having recurrent, chronic diarrhoea for the past 5 months now. He claims to not have noticed any discernible pattern. Her does not smoke and is a teetotaler. Upon examination, the patient’s clothing appears to be ill-fitting. A blood test was subsequently done and revealed the following: Haemoglobin 118 g/L (130-180 g/L) Mean cell volume (MCV) 106 fL (76-96 fL) A peripheral blood film is significant for a diamorphic picture of red cells. Following the results of the blood tests, the patient was booked for an endoscopy. A few tissue samples were taken during the endoscopy and sent for histology evaluation. What is the most likely pathology to be seen on histology?
Correct Answer : C
This man is suffering from coeliac disease. Malabsorption typically presents with diarrhoea and weight loss. The malabsorption from coeliac disease can result in either iron deficiency, folate, or B12 deficiency anemias. In this case, since the MCV is high, it is likely folate or B12 deficiency (more often folate deficiency). The term dimorphic red blood cells is used when one observes two types of distinct morphology in the circulating red cell population.
It is seen in B12 and folate deficiencies, sideroblastic anemias, post-transfusions, myelodysplasia, and iron deficiencies. Coeliac disease is confirmed by finding villous atrophy on small bowel biopsy (usually duodenum) by endoscopy.
The GP would likely have sent off specific auto-antibodies, such as tissue transglutaminase (TTG) antibodies (IgA) to investigate for coeliac disease when ordering the initial blood test. This information was omitted as the answer would then be too obvious.
Q.13. A 50 year old man comes to A&E with abdominal pain that began suddenly about 1 hour ago. The pain is now generalized, constant, and extremely severe. He lies motionless on the stretcher, is diaphoretic, and has shallow, rapid breathing. His abdomen is rigid, very tender to deep palpation, and has guarding. X-rays show free air under the diaphragm. What is the most likely diagnosis?
Correct Answer : B
An acute abdomen. The X-ray which shows free air under the diaphragm is classical for a perforation. Lying motionless and having a rigid, tender abdomen with signs of guarding is typical for a perforated peptic ulcer. Perforated peptic ulcer Perforation of a gastric or duodenal ulcer is usually a severely painful sudden event. It may occur in those without known peptic ulcer disease, as well as those with previously diagnosed problems.
However, close questioning may reveal recent symptoms attributed to ‘indigestion’. Sudden localized epigastric pain spreads to the remainder of the abdomen the pain is worse on coughing or moving and may radiate to the shoulder tip Examination Although distressed, the patient often prefers to lie still, rather than roll about.
Absent bowel sounds, shock, generalized peritonitis, and fever develop as time passes. Investigations An erect chest X-ray will demonstrate free gas under the diaphragm In those cases where the diagnosis is suspected, but not proven by X-ray, a contrast CT scan may help.
Treatment;
• Provide IV analgesia
• Give an antiemetic (eg IV metoclopramide 10mg).
• Resuscitate with IV 0.9 % saline.
• Refer to the surgeon and give IV antibiotics.
Q.14. A 61 year old man presents with fatigue and palpitations. His past surgical history includes an ileal resection which was performed one year ago. CBC was requested and the results are as follows: Haemoglobin 93 g/L Mean cell volume (MCV) 111 fL What is the most likely diagnosis?
Correct Answer : D
High MCV and low Hb – Macrocytic anaemia These findings together with a history of ileal resection whereby malabsorption of B12 could occur, point towards the diagnosis of B12 deficiency.
COMPARISON OF CAUSES BETWEEN VITAMIN B12 AND FOLATE DEFICIENCY
Vitamin B12 deficiency
- Malabsorption
-Pernicious anaemia
- Medical conditions of small intestine (coeliac disease, tropical sprue, Crohn’s disease)
- Gastric resection (for reasons of obesity or cancer)
- Inadequate dietary intake
- Low intake of cobalamin-rich foods.
Folate deficiency :
- Malabsorption
- Poor bioavailability
- Medical conditions
- Inflammation of small intestine (coeliac disease, tropical sprue, Crohn's disease)
- Inadequate dietary intake
- Low intake of folate-rich foods (usually vegetables).
In exam, one distinction that may help you choose between B12 and folate deficiency is the diet.
Good food sources of folate include broccoli, brussels sprouts, asparagus, and peas (basically vegetables). Thus if the given scenario is a vegetarian, it is unlikely that he is suffering from folate deficiency. In that case, pick B12 deficiency.
Q.15. A 35 year old man presents to his doctor with a history of dyspepsia intermittently for the past 3 months. Serum antibodies for Helicobacter pylori which were performed a month ago for his symptoms were negative. There has been no improvement with his symptoms despite taking a proton pump inhibitor for the past 1 month. He reports no weight loss or blood in his stools. There is no previous history of non-steroidal anti-inflammatory drug (NSAID) use. He does not smoke and drinks a cup of coffee a day. An abdominal examination reveals slight tenderness at the epigastric region without any mass felt. What is the most appropriate next step?
Correct Answer : B
This patient is less than 55 years old and does not have any red flags. As his initial antibodies for Helicobacter pylori are negative and his symptoms have not resolved, it would be appropriate to refer this patient for an endoscopy. On the other hand, if his serum antibodies for Helicobacter pylori were initially positive, then a urea breath test would be appropriate.
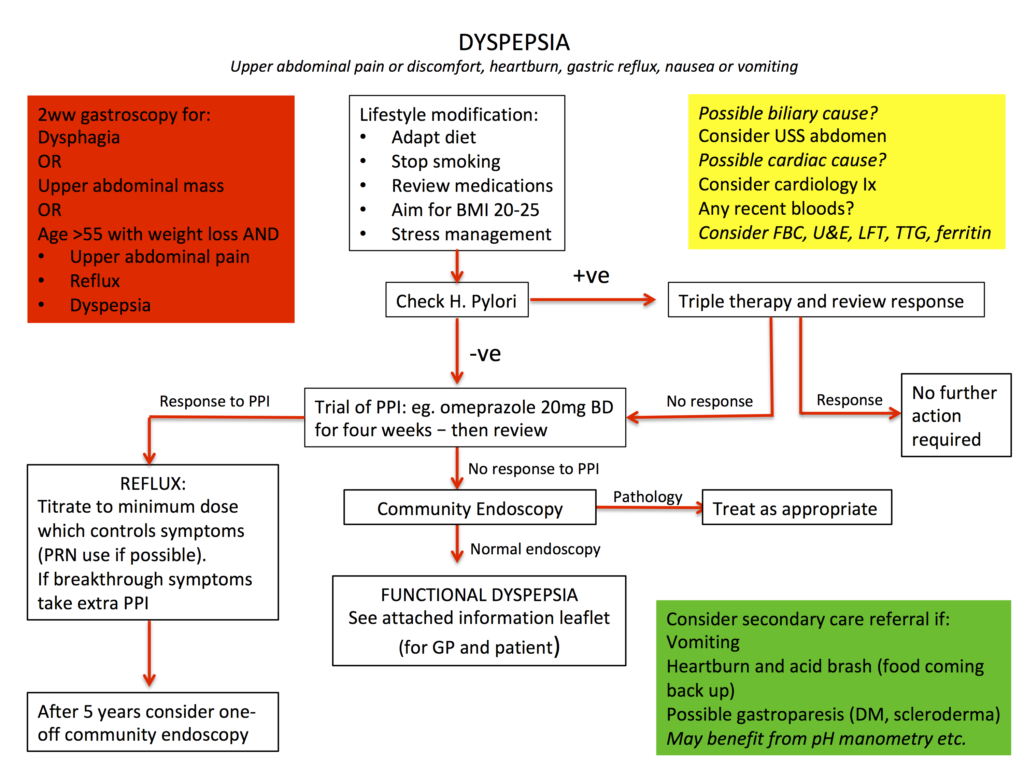
GENERAL MANAGEMENT FOR DYSPEPSIA, HELICOBACTER PYLORI TESTING :
Whilst we have put in this diagram to use H. pylori antibody testing if no response to lifestyle modifications and antacids, NICE recommends any locally validated test for H. pylori which includes the carbon-13 urea breath test, stool antigen test, or serum antibody testing.
In practice, if the patient is taking proton pump inhibitors, remember to stop it for 2 weeks before performing a urea breath test or stool antigen test.The only test that you need to remember for re-testing for H. pylori is the carbon-13 urea breath test as NICE recommends this as there is still insufficient evidence to recommend stool antigen test as a test for eradication.
Serological tests have no value in confirming successful eradication because the antibodies persist after successful eradication.
Q.16. A 45 year old man had an endoscopy earlier in the day for investigations for chronic abdominal pain. The next day evening, he returns to the hospital with complaints of chest pain and shortness of breath. The pain is seen worse at the epigastric area and radiates to the inter scapular region of the back. His abdomen is soft and nontender. His respiratory rate is 29 breaths/minute, pulse rate is 110 beats/minute, a temperature of 37.8 C and blood pressure is 120/70 mmHg. A chest X-ray reveals mediastinal widening. What is the most likely diagnosis?
Correct Answer : D
Mediastinitis may occur after oesophageal perforation or rupture, due to a variety of reasons with endoscopy being one of them. Oesophageal perforation or rupture should not be taken lightly as it is a life-threatening condition. Often air along the subcutaneous planes or into the mediastinum would cause chest pain, dyspnoea, and fever. This patient should be considered critically ill and require management in the intensive care unit. It may be difficult to catch the diagnosis early in the course of mediastinitis as the signs and symptoms may be subtle.
However, as the condition progresses, patients would experience increasing chest pain, respiratory distress, and odynophagia. The most prominent symptom of mediastinitis is chest pain and this is localized depending on the portion of mediastinum involved. In anterior mediastinitis, pain is located at the substernal region while in posterior mediastinitis, the pain is localized to the epigastric region with radiation to the interscapular region.
A chest X-ray may show a widened mediastinum or air in the mediastinum. Water-soluble contrast can be added if needed. If there is diagnostic uncertainty, a direct visualization using endoscopy is used to confirm the diagnosis. The principles of managing mediastinitis due to oesophageal perforation include repairing the defect and treatment with antibiotics.
Q.17. 42 year old obese woman presents to the emergency department with a 12 hour history of severe epigastric pain. The pain started suddenly and radiates to her back. It is relieved when sitting forward. She is nauseous and has vomited twice since the pains started. She drinks one and a half glasses of wine per day. She has no significant past medical history. She has a pulse rate of 110 beats/minute and is tender in the epigastric region. What is the most appropriate investigation?
Correct Answer : C
The likely diagnosis is acute pancreatitis. The most useful investigation is a serum lipase, looking for an elevation of more than 3 times the upper limit of normal. While abdominal X-rays are not useful in the diagnosis of pancreatitis, they are routinely ordered to exclude other potential causes of abdominal pain such as perforation or bowel obstruction. Ultrasound is useful to detect the presence of gallstones but it is not a good diagnostic test for acute pancreatitis.
The pancreas is poorly visualized in 25-50% of cases. Urea and electrolytes and liver function tests do not directly aid the diagnosis of pancreatitis however, they help assess the severity of the disease (e.g. showing the degree of leucocytosis or hypovolaemia) or give clues of the aetiology of pancreatitis (e.g. gallstone pancreatitis). Acute pancreatitis Aetiology The vast majority of cases are caused by gallstones and alcohol.
A popular mnemonic to remember is " GET SMASHED "
• Gallstones
• Ethanol
• Trauma
• Steroids
• Mumps (other viruses include Coxsackie B)
• Autoimmune (e.g. polyarteritis nodosa), Ascaris infection
• Scorpion venom
• Hypertriglyceridaemia, Hyperchylomicronaemia, Hypercalcaemia, Hypothermia
• ERCP
• Drugs (azathioprine, mesalazine*, didanosine, bendroflumethiazide,furosemide, pentamidine, steroids, sodium valproate)
Clinical features :
• Gradual or sudden severe epigastric or central abdominal pain (radiates to back, sitting forward may relieve it)
• Vomiting is prominent
• Tachycardia
• Fever,
• Jaundice
• Shock
• Rigid abdomen with local or general tenderness
• Periumbilical bruising (Cullen’s sign)
Investigation :
• Raised serum amylase (>1000U/mL or around 3-fold upper limit of normal).However, lipase levels are more sensitive and more specific.
• CT scan with contrast enhancement may be diagnostic where clinical and biochemical results are equivocal on admission.
Q.18. A 21 year old female presents to the Emergency Department with the complaint of severe diarrhoea. She says that she opens her bowels in excess of eight times a day for the past week and that she has noticed that her stool is covered in blood yesterday. She is extremely anxious and scared about the fact that she has bloody stools as she is afraid that she could have colon cancer. On further questioning, she reveals that her grandfather passed away five years ago from colorectal carcinoma. She also complains of colicky abdominal pain and an urgency to visit the toilet. Her medical history is significant for ulcerative colitis which she takes sulfasalazine for. On physical examination, the patient appears pale. Examination of her abdomen reveals a tender abdomen with no palpable masses or distention. Her heart rate is 100 beats/minute and temperature is 38 C. What is the next best step in this patient’s management?
Correct Answer : B
This patient is suffering from an acute flare of ulcerative colitis. The stem gives multiple clues that allude to the severity such as bloody diarrhea (which is the hallmark of the disease), several bowel motions a day, tachycardia, and pyrexia. Intravenous corticosteroids are used for the treatment of acute and severe ulcerative colitis. This patient displays signs and symptoms of a severe exacerbation and should be referred to the medical team.
Topical aminosalicylates and oral corticosteroids have their place in the management of mild to moderate exacerbation of the disease but not in severe flare-ups like this.
It is also worth mentioning that if the question had asked for an appropriate investigation, an abdominal X-ray would be very appropriate in this setting to look for features suggestive of toxic megacolon.
ULCERATIVE COLITIS MANAGEMENT - Inducing remission
• First line – topical aminosalicylates e.g. Rectal mesalazine o Rectal aminosalicylates are better than rectal steroids and also better than oral aminosalicylates alone
• If not responding, then add 5-ASA (e.g. oral mesalazine)
• If still not responding, then add oral prednisolone If severe colitis, treat in the hospital with IV steroids as first-line In the exam, how do you know if this is severe colitis?
It is severe if the following are present:
• More than 6 bowel movements
• Visible blood in large amounts
• Pyrexia more than 37.8 C
• Tachycardic
• Anaemic
• ESR more than 30
Maintaining remission -
• Oral aminosalicylates e.g. mesalazine
• If remission is not well maintained, consider oral azathioprine or mercaptopurine.
Q.19. A 31 year old female presented with complaints of chest pain and difficulty in swallowing liquids and solids. She has also been suffering from recurrent chest infection for the past few months. What is the most likely diagnosis?
Correct Answer : D
The diagnosis here is achalasia. In achalasia, dysphagia is often with both fluids and solids and in fact, solids are affected more than soft food or liquids. It can sometimes present as chest pain or with recurrent chest infections. Chest infections or aspiration pneumonia results from untreated achalasia that leads to nocturnal inhalation of material lodged in the oesophagus and aspiration pneumonia.
Q.20. A 54 year old woman, known case of pernicious anaemia refuses to take hydroxocobalamin intramuscularly as she needle shy. She is asking for medication. What is the best reason that describes why oral medications will not be effective?
Correct Answer : C
Pernicious anaemia is caused by autoimmune atrophic gastritis, leading to achlorhydria and a lack of gastric intrinsic factor secretion. Injections are required. Note: if the cause of B12 deficiency is not due to pernicious anaemia (e.g. dietary), then oral B12 can be given after the initial acute course.
Q.21. While performing an appendectomy, a surgeon found a mass in the caecum of a patient. The mass was removed and sent for analysis. Analysis revealed a transmural infiltration with lymphocytes and granulomas without necrosis. What is the most probable diagnosis?
Correct Answer : A
This is a difficult question to answer as there is not much background information in terms of patient history or signs and symptoms in terms of patient presentation. Based on the histology, we would be tempted to choose Crohn’s disease as a diagnosis as Crohn's disease is known to have histopathology of:
· Abdominal mass palpable in right iliac fossa
· Increased goblet cells on histology
· Granulomas seen on histology
· Transmural, skip lesions, cobblestone appearance on endoscopy
· Kantor's string sign, rose thorn ulcers and fistulae are seen on a small bowel enema.
Based on the histopathology ALONE the correct answer is D.
In reality, the patient presents with the classical signs and symptoms of Crohn’s disease i.e:
· diarrhoea (which may be bloody and become chronic - if present for more than six weeks)
· abdominal pain and/or weight loss
· periods of acute exacerbation, interspersed with remissions or less active disease.
· Systemic symptoms of malaise, anorexia, or fever
· Abdominal tenderness or distension, palpable masses.
· Anal and perianal lesions (pendulous skin tags, abscesses, fistulae) are characteristic.
· Mouth ulcers.
Some additional points to remember to diagnose UC or CD:
1. Fecal calprotectin
2. Abdominal X Ray - to exclude colonic dilatation
3. Stool exam
4. Barium fluoroscopy
5. Sigmoidoscopy/colonoscopy + biopsy
Ulcerative Colitis Management - Inducing remission
Topical * Rectal Mesalazine is better than rectal steroids 1st line
* 5-ASA (e.g. oral mesalazine) 2nd line.
* Oral Prednisolone - If severe colitis, is treated in the hospital with IV steroids as the first line. Maintaining remission oral aminosalicylates e.g. mesalazine
Management of Crohn’s disease Inducing remission :
1st line * Oral Prednisolone 2nd line *5-ASA drugs (e.g. mesalazine) azathioprine or mercaptopurine may be used as an add-on medication to induce remission but is not used as monotherapy metronidazole is often used for isolated perianal disease. Maintaining remission 1st line * azathioprine or mercaptopurine.
Q.22. An 8 year old child presents with recurrent abdominal pain. He has three episodes of abdominal pain within the last 3 months and it is severe enough to affect his activity in school. The abdominal pain is intense and located periumbilically lasting for a few hours and is associated with nausea and episodic headaches. He maintains a good appetite and is an appropriate weight for his age. On examination, there were no significant findings. Full blood count, urea and electrolytes are found to be normal. What is the most appropriate next step in management?
Correct Answer : D
Recurrent abdominal pain with episodic headaches in a child with no abnormal findings examination and investigation points towards a diagnosis of Abdominal Migraine.
Abdominal migraines are a type of functional pain. It is usually characterized by having:
• Paroxysmal episodes of intense, acute periumbilical pain lasting for one or more hours
• Pain is dull or "just sore" quality
• Intervening periods of usual health, lasting weeks to months
• The pain interferes with normal activities
• The pain is associated with two or more of the following: anorexia, nausea, vomiting
• Not attributed to another disorder Reassurance is all that is needed.
Q.23. A 52 year old alcoholic presents to the Emergency Department with complaints of worsening epigastric and back pain. The pain is episodic and there are times that he is pain-free. He also complains of having loose pale, offensive stools. He has lost weight over the past few months which he attributes due to the fear of eating as the pains often worsen after eating. On examination, he has epigastric tenderness. An x-ray of the abdomen was performed which showed diffuse calcifications in the abdomen. What is the most likely diagnosis?
Correct Answer : C
Chronic pancreatitis often presents with abdominal pain. Classically, the pain is located at the epigastrium and radiates to the back.
The pain is worse after eating leading to a dislike of eating with consequent weight loss. The second most predominant feature is malabsorption which is represented here by steatorrhoea. Malabsorption again contributes to weight loss.
Alcohol is one of the significant risk factors for chronic pancreatitis but it is not a good hint to pick chronic pancreatitis as the answer based on an alcohol history as alcohol also contributes to acute pancreatitis, gastro-oesophageal reflux, oesophagitis, and indirectly to pancreatic cancer.
One might consider “Carcinoma of the head of the pancreas” as the answer given the similar symptoms of weight loss, epigastric pain, and history of alcohol. In reality, it is difficult to differentiate the two hence the importance of imaging modalities such as ultrasounds and CT scans.
In chronic pancreatitis, plain abdominal films of the pancreas can show diffuse calcifications which indicate significant damage to the pancreas. X-rays of the abdomen are not one of the main imaging modalities of the pancreas, and it is usually done for other reasons such as to exclude bowel perforation in A&E. Again to stress that ultrasound and CT scans would be better imaging modalities for pancreatic diseases.
Q.24. A 44 year old male was admitted to the medical ward with complaint of diarrhoea, abdominal pain and weight loss for the last few months. The examination notes finger clubbing, perianal skin tags and abdominal tenderness. A colonoscopy reveals transmural granulomatous inflammation involving the ileocaecal junction. What is the most likely diagnosis?
Correct Answer : A
Transmural granulomatous inflammation involving the ileocaecal junction is one of the features seen in Crohn’s disease.
Q.25. A 35 year old female presents with secondary amenorrhoea. Her blood tests show the following: Serum bilirubin 42 micromol/L Alanine transferase (ALT) 115 iu/L Aspartate transaminase (AST) 89 iu/L Alkaline phosphatase (ALP) 189 iu/L What is the most likely diagnosis?
Correct Answer : B
The combination of deranged LFTs combined with secondary amenorrhoea in a young female strongly suggests autoimmune hepatitis. In autoimmune hepatitis, serum aminotransferases: aspartate aminotransferase (AST) and alanine aminotransferase (ALT) are usually elevated at initial presentation.
Serum alkaline phosphatase is normal or only mildly raised. A more than two-fold elevation suggests an alternative or additional diagnosis. Occasionally, the stem would include a form of another autoimmune disease such as Addison’s disease, vitiligo, or an autoimmune thyroid disorder as this may be present with autoimmune hepatitis.
Autoimmune hepatitis (AIH) is a chronic disease of unknown cause, characterized by continuing hepatocellular inflammation and necrosis, which tends to progress to cirrhosis.
• Predominantly affects young or middle-aged women
• Up to 40% present with acute hepatitis and signs of autoimmune disease, eg fever, malaise, urticarial rash, polyarthritis, pleurisy, pulmonary infiltration, or glomerulonephritis. The reminder present with gradual jaundice or are asymptomatic and diagnosed incidentally with signs of chronic liver disease.
Amenorrhoea is common and the disease tends to attenuate during pregnancy.
Investigations:
The diagnosis rests on a combination of compatible biochemical, immunological and histological features together with the exclusion of other liver diseases. Associated diseases : Concurrent autoimmune disorders occur in approximately 40% of patients, particularly autoimmune thyroid disorders.
Q.26. A 46 year old woman presents with sudden episode of abdominal pain which started about 5 hours ago. The pain is located in the epigastrium and radiates to her back. She has vomited twice since the onset of attack. The pain is made worse by lying flat on her back and she is more comfortable sitting up and bending forwards. She was informed of the presence of gallstones in her gallbladder four weeks earlier when she reported pain in the right hypochondrium. Her temperature is 38.4 C, blood pressure is 120/85 mmHg, and pulse rate is 115 beats/minute. There is no presence of jaundice but there is marked tenderness in epigastrium. What is the most appropriate investigation?
Correct Answer : D
The likely diagnosis is acute pancreatitis. Serum amylase and lipase are appropriate investigations, looking for an elevation of more than 3 times the upper limit of normal.
While abdominal X-rays are not useful in the diagnosis of pancreatitis, they are routinely ordered to exclude other potential causes of abdominal pain such as perforation or bowel obstruction. Ultrasound is useful to detect the presence of gallstones but it is not a good diagnostic test for acute pancreatitis. The pancreas is poorly visualized in 25-50% of cases.
Urea and electrolytes and liver function tests do not directly aid the diagnosis of pancreatitis however, they help assess the severity of the disease (e.g. showing the degree of leucocytosis or hypovolaemia) or give clues of the aetiology of pancreatitis (e.g. gallstone pancreatitis).
Q.27. A 56 year old man comes for a routine checkup. He is noted to have increased skin pigmentation, spider angioma and a heart murmur. He has mild joint pain particularly in those of the hands. He rarely drinks alcohol. On examination, his liver is firm and has a span of 10 cm. On further investigations of the heart murmur, he was given the diagnosis of restrictive cardiomyopathy. What is the condition that he is most likely at risk of?
Correct Answer : B
Hepatoma (more often called hepatocellular carcinoma) is a primary malignancy of the liver. The given scenario has features of hemochromatosis which is among the causes of restrictive cardiomyopathy. It is a very well-known fact that. patients with hemochromatosis have an increased risk of developing hepatocellular carcinoma. The liver is a primary storage area for iron and will naturally accumulate excess iron. Over time the liver is likely to be damaged by iron overload causing cirrhosis.
Cirrhosis and hemochromatosis together will increase the risk of hepatocellular carcinoma.
HAEMOCHROMATOSIS :
Hereditary haemochromatosis (HHC) is an autosomal recessive genetic disease in which increased intestinal absorption of iron causes accumulation in tissues, especially the liver, which may lead to organ damage. Other organs that may be affected by iron deposits include the pancreas, joints, heart, skin, and gonads.
Presentation :
• Early diagnosis is difficult because HHC is often asymptomatic until the latest of disease.
• Symptoms usually start between ages 40-60
• Initial symptoms are usually vague and nonspecific - eg, fatigue, weakness heart problems
• HHC may be diagnosed incidentally - eg, following abnormal serum ferritin or lifts
• Symptoms of advanced disease include:
o Diabetes
o Bronzing of the skin
o Hepatomegaly
o Cirrhosis
o Arthropathy
o Cardiac disease - arrhythmias or cardiomyopathy
o Neurological or psychiatric symptoms
- impaired memory, mood swings, irritability, depression
Remember the triad of diabetes, hepatomegaly, and bronze pigmentation. This is seen in 30% of patients with hemochromatosis and is a common presentation given in the questions.
Q.28. A 15 year old child complains of right iliac fossa pain worsening over the past few weeks. He also has bouts of diarrhoea coming in episodes for more than a year. He has lost 7 kg in the last 5 months. On examination, perianal skin tags were seen. He was subsequently referred on to the gastroenterology team. A colonoscopy was performed which showed deep ulcers and skip lesions on the colonic mucosa. What is the most appropriate management??
Correct Answer : B
The diagnosis of Crohn’s disease is quite clear here. Skip lesions are a give away that this is Crohn’s disease. This is also supported by the weight loss and the perianal skin tags.
Q.29. A 36 year old bodybuilder presents with sudden onset of severe abdominal pain. He was previously fit and well and only suffers from indigestion occasionally. He has been taking ibuprofen for a long term knee injury. On examination, he has a rigid abdomen, lies motionless on the bed and has no bowel sounds. His pulse rate is 115 bpm and blood pressure is 100/60 mmHg. What is the most likely diagnosis?
Correct Answer : A
The diagnosis here is a perforated peptic ulcer induced by NSAIDs. The sudden onset, rigid abdomen, silent and no bowel sounds are all hints that point toward perforated peptic ulcer.
Q.30. A 69 year old smoker has had increasing dysphagia when eating solid food which has been on going for the past 3 months. He has noticed a drop of 8 kg in weight in the past few months. What investigation is most likely to lead to a diagnosis?
Correct Answer : D
The likely cause is oesophageal cancer where a malignant stricture or mass has resulted in difficulty in swallowing. An endoscopic biopsy is the definitive investigation. Oesophageal cancer Adenocarcinoma has now overtaken squamous cell carcinoma as the most common type of oesophageal cancer
Risk factors :
• Smoking - risk factor for both adenocarcinoma and squamous cell carcinoma, but associated with a much higher risk for squamous cell carcinoma than adenocarcinoma.
• Alcohol
• GORD
• Barrett's oesophagus - which is a precursor of adenocarcinoma
• Achalasia - Chronic inflammation and stasis from any cause increase the risk of oesophageal squamous cell carcinoma Very often in the stem, there would be a patient with a history of gastro-oesophageal reflux disease (GORD) or Barrett's oesophagus. Sometimes, they would give a history of increasing dysphagia and weight loss.
Diagnosis :
• Upper GI endoscopy with brushings and biopsy of any lesion seen is the first line test
• CT or MRI scan of the chest and upper abdomen is performed for staging purposes.
Q.31. A 70 year old woman is reviewed following a course of oral clindamycin for a right lower limb cellulitis. She was initially admitted in the hospital for 3 days for the management of her cellulitis as she was unable to weight bear. She was discharged 2 days ago and quickly developed bloody diarrhoea and abdominal pain. She has a temperature of 38.8 C. Her blood tests show: Haemoglobin 125 g/L White blood cells 18 x 109/L CRP 160 mg/l What is the most likely management?
Correct Answer : A
The scenario shows a classical picture of Clostridium difficile for which oral metronidazole is a treatment.
The two risk factors here are:
• Clindamycin – increased risk of Clostridium difficile infections
• Recently been in hospital – likely where she may have picked up C. diff In the exam, look out for antibiotic usage like cephalosporins, clindamycin, co-amoxiclav, and amoxicillin as a cause for Clostridium difficile.
Q.32. A 60 year old man presents with a lump in the left supraclavicular region. He complains that he does not eat as much anymore because he does not have the appetite. He has also lost 10 kg in the last 3 months. What is the most probable diagnosis?
Correct Answer : C
The lump in the left supraclavicular region is known as a Virchow’s node. It is indicative of carcinoma of the stomach. The weight loss and decreased appetite support the diagnosis of gastric cancer.
Q.33. A 43 year old male alcoholic presents after a large haematemesis. He has some other spidernaevi on his chest. His blood pressure is 100/76 mmHg and pulse rate is 110 beats/minute. On examination, a swollen abdomen with shifting dullness is seen. What is the most likely diagnosis?
Correct Answer : C
Spidernaevi and ascites are suggestive of liver disease. It is likely that with the history of alcohol, and his signs and symptoms, he has a diagnosis of chronic liver disease which has resulted in portal hypertension and bleeding from oesophageal varices.
Oesophageal varices :
• Dilated sub-mucosal veins in the lower third of the oesophagus. This can lead to variceal haemorrhage which occurs from the dilated veins (varices) at the junction between the portal and systemic venous systems. The bleeding is often severe and life-threatening. The majority of the patients would have a history of chronic liver disease.
Presentation:
• Haematemesis (most commonly), melaena
• Signs of chronic liver disease
Investigation:
• Endoscopy at early stage Acute management of variceal bleeding
• Always start with ABC
• Correct clotting: FFP, vitamin K
• Vasoactive agents like terlipressin Terlipressin should be offered to patients suspected variceal bleeding at presentation
• Antibiotic prophylaxis reduces mortality in patients with acute upper GI bleeding in association with chronic liver disease
• Endoscopic variceal band ligation If band ligation is not available, emergency sclerotherapy as first-line
• Sengstaken-Blakemore tube if uncontrolled haemorrhage
• Transjugular Intrahepatic Portosystemic Shunt (TIPSS) if still unable to control bleeding
Prophylaxis of variceal haemorrhage :
• Propranolol is often given at discharge to reduce portal pressure to decrease the risk of repeat bleeding.
Q.34. A 21 year old man has been brought to A&E by his friends as he is having a yellow sclera and yellowing of the skin. He has recently been having flu-like symptoms and a nonproductive cough. A urine dipstick was performed and was normal. His blood results show: Haemoglobin 129 g/dl Reticulocytes 1.2% Bilirubin 44 ?mol/L Alkaline phosphatase (ALP) 88 Alanine transferase (ALT) 24 Albumin 42 What is the most likely diagnosis?
Correct Answer : B
Gilbert's syndrome is usually an autosomal recessive disorder and is a common cause of unconjugated hyperbilirubinemia due to decreased UGT-1 activity which is the enzyme that conjugates bilirubin with glucuronic acid. It may go unnoticed for many years and usually presents in adolescence with intermittent jaundice occurring during illness, physical exertion, stress, or fasting. In this stem, the jaundice was precipitated by infection.
Investigations usually show a mildly raised serum bilirubin but the other LFTs remain within normal ranges as seen in this stem.
FBC would show normal reticulocyte count -this helps distinguish Gilbert’s syndrome from other types of haemolysis.
Urine dipsticks would be seen as normal as it is the unconjugated bilirubin that is high (not the conjugated bilirubin as would be seen in Dubin-Johnson syndrome). Remember, viral infections are common triggers for a rise in bilirubin in patients with Gilbert's syndrome.
Q.35. A 33 year old pregnant woman develops severe epigastric pain, nausea and vomiting at 35 weeks gestation. She was diagnosed with pre-eclampsia 2 weeks ago. On examination, she has yellow sclerae. Laboratory investigations show a deranged liver function, low platelets, low serum glucose, raised serum ammonia. What is the most likely diagnosis?
Correct Answer : D
Acute fatty liver of pregnancy (AFLP) and HELLP (Haemolysis, Elevated Liver enzymes, Low Platelets) syndrome both have low platelets and deranged liver function as part of the clinical picture. However, low serum glucose and/or raised serum ammonia are more suggestive of AFLP. Vomiting is also more commonly seen in AFLP than HELLP syndrome.
Acute fatty liver of pregnancy Acute fatty liver pregnancy (AFLP) is a rare form of jaundice in pregnancy. It occurs late in pregnancy and may be life-threatening.
The aetiology of AFLP is unknown. It is part of the spectrum of disorders related to pre-eclampsia. Differentiation from HELLP(Haemolysis, Elevated Liver enzymes, Low Platelets) syndrome can be difficult as signs and symptoms can overlap.
Risk factors ;
• Pre-eclampsia - There is associated pre-eclampsia in 30–60% of AFLP
• First pregnancies
• Multiple pregnancy
Presentation :
• Presents acutely with: o Nausea o Vomiting o Abdominal pain o Fevers o Headache o Pruritus o Jaundice
• Begins typically after 30 weeks of gestation
• It also may appear immediately after delivery. Severe hypoglycaemia and clotting disorder may develop causing coma and death
Investigations :
• Liver transaminases are elevated (ALT is typically elevated more than 500 U/L)
• Raised serum bilirubin
• Hypoglycaemia
• Abnormal clotting with coagulopathy (prolongation of prothrombin and partial thromboplastin times)
• Biopsy would be diagnostic
Management :
• Treat hypoglycemia
• Correct clotting disorders
• N-acetylcysteine (NAC)
• Consider early delivery
A DIFFERENTIATING AFLP FROM HELLP :
Acute fatty liver of pregnancy vs Haemolysis, Elevated Liver Enzymes, Low Platelets syndrome.
HELLP AFLP Epigastric pain ++ + Vomiting ++ Hypertension ++ + Proteinuria ++ + ALT/AST + + Hypoglycaemia ++ Hyperuricaemia + ++ DIC + ++ Thrombocytopenia ++ + WBC + ++ Ammonia ++ Acidosis ++ Haemolysis ++
Q.36. A 28 year old man has intermittent diarrhoea, fatigue and weight loss over the last 6 months. He has excluded gluten from his diet in the last 2 months and his symptoms have resolved. He wants to be tested to confirm the diagnosis of coeliac disease. What is the most appropriate next step in action?
Correct Answer : B
If patients are already taking a gluten-free diet they should be asked, if possible, to reintroduce gluten for at least 6 weeks before testing. Serology tests and jejunal biopsies may come back negative if the patient is currently on a gluten-free diet.
Q.37. A 22 year old female comes to the doctor with complaints of diarrhoea for several months which have been worsening over the past week. She says that she opens her bowels in excess of five times in a day for the past week. She also has recurrent bloating that makes her very uncomfortable, with right sided abdominal pain. The pain is mild and does not interfere with her daily activities, but she is quite concerned about the blood in stools which she noticed this morning. She leads a busy lifestyle, holding down two jobs and has had some recent weight loss which she attributes to stress and poor nutrition. She smokes a pack of cigarettes a day to deal with her stress. There is no significant past medical history. On physical examination, the patient appears pale. Her body mass index is 17 kg/m2. On further oral examination, she is noted to have multiple ulcers in her mouth. Abdominal examination reveals distended abdomen, tenderness on right lower quadrant with no palpable masses. What is the most likely cause of her condition?
Correct Answer : A
The patient is suffering from Crohn’s disease. In this scenario, we have multiple clues which point towards Crohn’s disease such as diarrhoea with the location of abdominal pain. The common site of the pain in Crohn’s disease is the lower right side of the abdomen due to the involvement of the small intestine (ileum). Other common features are weight loss and mouth ulcers. Another subtle hint is the smoking history.
Smoking increases the risk of developing Crohn’s by about three to four times. While ulcerative colitis also can present as chronic diarrhoea, it more often involves the other part of the colon (left-sided colitis) In coeliac disease, the diarrhoea is mainly due to malabsorption, which leads to abnormally high levels of fat in stools termed steatorrhoea, which is not the case in this patient.
Colon cancer is the last thing that you should be thinking of in a patient in this age group. Medications are not the right option as there is no significant past medical history in this patient.
Q.38. A 26 year old young man presents to the surgeon with a history of passing loose stools for the past 2 months. He says his stools contain a small amount of blood and mucous and are associated with abdominal pain. He has around 4 to 5 bowel movements a day. A colonoscopy was organized and performed which he was started on treatment. What is the most appropriate treatment for his condition?
Correct Answer : B
The clinical features and treatment after colonoscopy suggest a diagnosis of ulcerative colitis for which the initial treatment of mild to moderate symptoms is mesalazine.
Q.39. A 33 year old female has intermittent diarrhoea and abdominal bloating which is usually exacerbated by consumptiion of wheat and eggs. She has been feeling more tired in the past few months. She has no significant weight loss. What is the SINGLE most likely diagnosis?
Correct Answer : A
The best answer here is coeliac disease. Whilst coeliac disease indeed causes malabsorption which accounts for intermittent diarrhoea and abdominal bloating, the more specific answer is still Coeliac disease since there is a history of wheat in the diet. Eggs do not exacerbate coeliac disease as it is not gluten however her meals which contain wheat is likely the cause of her malabsorption symptoms.
Q.40. A 42 year old man with type 2 diabetes presents with fatigue and shortness of breath. He is noted to have a bronze tinge to his skin. Abdominal examination reveals hepatomegaly. His blood test show a high ferritin level. A diagnosis has been made but he is refusing all treatment. Which organ is the most likely to be at risk of developing cancer?
Correct Answer : C
The diagnosis here is haemochromatosis. The liver is a primary storage area for iron and will naturally accumulate excess iron. Over time, the liver is likely to be damaged by iron overload causing cirrhosis. Cirrhosis and hemochromatosis together will increase the risk of hepatocellular carcinoma.
Q.41. A 42 year old female presents to her GP following a staging CT for her recently diagnosed renal cell carcinoma. On the CT scan, gallstones were noticed in the gallbladder. She has no history of abdominal pain or jaundice and is otherwise well. A left sided nephrectomy for her renal cell carcinoma has been scheduled. What is the most appropriate course of action?
Correct Answer : D
Reassurance is the correct option here. It is reserved for patients who are asymptomatic and have stones in their gallbladder. Stones that are found incidentally, as a result of imaging investigations unrelated to gallstone disease in asymptomatic patients do not require any intervention. But be aware that if the gallstones were found in the common bile duct instead of the gallbladder, then a laparoscopic cholecystectomy may be needed regardless if they are symptom-free or have symptoms.
Q.42. A 45 year old man had his head of pancreas removed due to malignancy. 10 days later, he complains of worsening abdominal pain. On examination, he has a rigid abdomen which is tender. He has a temperature of 37.5 C, a blood pressure of 95/55 mmHg and a pulse rate of 125 bpm. His past medical history includes peptic ulcer disease. What is the most appropriate next action?
Correct Answer : C
This is a case of perforated peptic ulcer with the features of shock, abdominal rigidity, and raised temperature. Perforation of a peptic ulcer causes an acute abdomen with epigastric pain that may progress to generalized rigidity. The stress of an operation may cause the body to produce higher amounts of acid, which can irritate preexisting ulcers leading to easy perforation. A diagnosis is made by taking an erect abdominal/chest X-ray (seeking air under the diaphragm).
Q.43. A 48 year old female presents with tiredness and painless dysphagia. She complains of a feeling of something stuck in her throat. A full blood count shows microcytic, hypochromic anaemia. On examination, glossitis is noted. An oesophageal web is found at the post cricoid region. What is the most likely diagnosis?
Correct Answer : A
When someone presents with dysphagia, glossitis, and iron deficiency anaemia, Plummer-Vinson syndrome is your answer. Plummer Vinson syndrome • A condition where iron deficiency is associated with a post-cricoid oesophageal web The syndrome most often affects middle-aged women.
Presentation:
• Painless, intermittent dysphagia due to oesophageal webs
• Symptoms of iron-deficiency anaemia
Management:
• Iron supplements
• Dilation of the webs
Q.44. A 49 year old female presents with right hypochondrial pain. An ultrasound shows a large gallstone. Her BP is 120/85 mmHg; respiratory rate 18/min; Heart rate 90 bpm; Temperature 37.6 C; WBC 15 x 109/L. What is the most appropriate treatment?
Correct Answer : C
As she is symptomatic, reassurance is out of the question. The two remaining options are laparoscopic cholecystectomy and emergency laparotomy. Laparoscopic cholecystectomy is the preferred option here as there are no signs of gallbladder perforation. Laparotomy has a higher risk as it is much more invasive.
Q.45. A 41 year old man has had a liver biopsy as part of investigations for abnormal liver function test. The pathology report states: special stains demonstrate the presence of a very large amount of iron pigment within hepatocytes. Which condition is identified by the pathology report?
Correct Answer : B
In haemochromatosis, characteristically, the iron is found predominantly in a periportal distribution (acinar zone 1) within the hepatic lobule, with virtually all iron deposited in parenchymal hepatocytes and none in Kupffer cells. By contrast, iron overload in haemosiderosis causes to accumulation of iron granules predominantly in kupffer cells and more in the central area rather than peripheral hepatocytes. Since the question gives a pathology report of a large amount of iron pigment in hepatocytes rather than Kupffer cells, the diagnosis is haemochromatosis.
Q.46. A 51 year old man has become increasingly fatigued over the past 10 months. His medical history includes having a gastrectomy a year ago. His physical examination is unremarkable. His blood tests show: Haemoglobin 85 g/L White cell count 7 x 109/L Platelets 240 x 109/L Mean cell volume 129 fL What is the most likely finding on a blood smear?
Correct Answer : A
These findings together with a history of a gastric resection whereby malabsorption of B12 could occur, point towards the diagnosis of B12 deficiency. Mean cell volume is also increased which supports that diagnosis. Hypersegmented neutrophils are seen on blood smears in megaloblastic anaemias.
Q.47. A 50 year old man has severe pain on defecation. On examination, a tender, reddish blue swelling is seen near the anal verge. What is the SINGLE most likely diagnosis?
Correct Answer : B
Perianal haematoma strictly speaking, it is a clotted venous saccule. It appears as a 2-4mm ‘dark blueberry’ (purple color) under the skin at the anal margin. It is seen as swollen and acutely tender perianal lumps.
Management: It may be evacuated under local anaesthesia or left to resolve spontaneously.
• Incision and drainage of the clot relieve pain but the thrombosis often recurs and there may be persistent bleeding.
• Conservative treatment includes analgesia, ice packs, and stool softeners. A topical calcium antagonist may help to relieve pain. If managed conservatively, symptoms usually settle within 10-14 days.
Q.48. A 28 year old female presents with 1 week history of jaundice, fever and malaise. She was diagnosed with hypothyroidism for which she is receiving levothyroxine. Her blood tests show: Serum bilirubin 40 ?mol/L Alanine transferase (ALT) 120 iu/L Aspartate transaminase (AST) 90 iu/L Alkaline phosphatase (ALP) 200 iu/L Prothrombin time (PT) 25 sec What is the most likely diagnosis?
Correct Answer : A
In autoimmune hepatitis, serum aminotransferases: aspartate aminotransferase (AST)and alanine aminotransferase (ALT) are usually elevated at initial presentation. Serum alkaline phosphatase is normal or only mildly raised. A more than two-fold elevation suggests an alternative or additional diagnosis.
Hypoalbuminaemia and prolongation of prothrombin time are markers of severe hepatic synthetic dysfunction. These lab tests do not rule out other liver diseases but given the combination of the presence of another autoimmune disease like hypothyroidism, the most likely diagnosis here is autoimmune hepatitis.
Q.49. A 35 year old man presents with burning retrosternal pain for the past few days. He has recently completed a course of treatment for H. pylori. Endoscopy shows multiple ulcers along the lower esophagus, stomach and duodenum. What is the next most appropriate investigation?
Correct Answer : C
The gastrin levels need to be checked to rule out a gastrinoma. A gastrinoma is a neuroendocrine tumor usually found in the pancreas or duodenum. These tumours secrete gastrin which stimulates parietal cells of the stomach to secrete hydrochloric acid into the stomach cavity leading to intractable peptic ulcerations. Gastrinomas are suspected when peptic ulcers occur at unusual sites, such as the second part of the duodenum or the jejunum, or ulcers recur after adequate surgery.
One-third of patients have watery diarrhea due to high gastric output. Diagnosis is made by measurement of fasting gastrin levels or secretin stimulation test.
ZOLLINGER-ELLISON SYNDROME :
Zollinger-Ellison syndrome is characterized by gastric acid over-secretion due to excessive levels of gastrin secreted from tumours found in the duodenum or pancreas. It presents as severe peptic ulcer disease, gastro-oesophageal reflux, and diarrhoea. When to suspect Zollinger-Ellison syndrome Suspect in those with:
• Multiple peptic ulcers resistant to drugs
• If associated with diarrhoea or steatorrhoea
• Associated with a family history of peptic ulcers.
Q.50. A 47 year old woman diagnosed with coeliac at the age of three has recently developed diarrhoea and weight loss for the past three months. What is the SINGLE most likely reason for this?
Correct Answer : D
One must remember the cancer risk associated with coeliac disease. Intestinal lymphoma is one of them.
Q.51. A 58 year old man has been having frequent episodes of secretory diarrhea for the past 2 weeks. His diarrhoea is extremely watery with large amounts of mucus. A diagnosis of villous adenoma was made after performing an endoscopy. What is the SINGLE most likely electrolyte abnormality?
Correct Answer : A
This is a very high-yield question and you need to remember that villous adenoma is one of the causes of hypokalaemia.
Q.52. A 45 year old smoker has suspected oesophageal carcinoma with a mass seen within the middle third of the oesophagus with metastasis to the liver. He has severe dysphagia. What is the most appropriate management to treat his symptoms?
Correct Answer : A
Dysphagia from inoperable oesophageal cancer is a complex issue with little consensus on the ideal management approach. For advanced cases of oesophageal cancer that are causing dysphagia, insertion of a stent into the oesophagus may be recommended.
The stent expands once in place and holds the oesophagus open to manage symptoms of dysphagia. Although radiotherapy also provides symptom relief (long-term relief), the waiting times for initiation of radiotherapy are long, and there are long lag times between initiation of treatment and relief of symptoms. Endoluminal stents provide more rapid and effective early relief for symptomatic patients.
Percutaneous endoscopic gastrostomy (PEG) is an endoscopic medical procedure in which a tube is passed into a patient’s stomach through the abdominal wall to provide a means of feeding when oral intake is not adequate. This is usually in stroke patients who are at risk of aspiration pneumonia or decompressing the stomach in cases of gastric volvulus.
OESOPHAGEAL STENT : An oesophageal stent is a tube placed in the oesophagus to keep a blocked area open so that the patient can swallow soft food and liquids. Oesophageal stents may be self-expandable metallic stents, or made of plastic, or silicone. They are used primarily in palliative cancer treatment.
Q.53. A 76 year old man is on treatment for prostate cancer and bone metastasis. He complains of only passing stool once every four to five days. He drinks adequate fluids and describes his stool as being soft. What is the SINGLE most appropriate management for his constipation?
Correct Answer : D
Since this patient is on treatment for prostate cancer and bone metastasis, logic dictates that he would also be taking a large amount of opioid medication.
One of the side effects of opioid-based medication, such as morphine, is constipation. Since he is only complaining of constipation and not hard stool, stool softeners are incorrect. He has no evidence of having impacted stool and therefore, phosphate enema is incorrect. A low-residue diet is a low fibre diet.
This is the blatantly incorrect answer in the choices. So we are left with two choices: senna and lactulose.
1. High fibre diet
2. Stimulatant laxative (senna)
3. Osmotic laxative (lactulose/macrogol)
4. Add on a prokinetic agent such as metoclopramide, domperidone, or erythromycin
5. Consider the use of a dantron-containing laxative
6. Seek specialist advice if the patient is still experiencing constipation.
Q.54. A 58 year old man presents with a lump in the left supraclavicular fossa. It has been present for the last 6 months. He also complains of dyspepsia and weight loss which he accounts for due to his reduced appetite. What is the most likely term for the lump?
Correct Answer : B
The lump in the left supraclavicular region is known as a Virchow’s node. It is indicative of carcinoma of the stomach. The weight loss and decreased appetite support the diagnosis of gastric cancer.
Q.55. A 35 year old man presented to his GP with the complaint of heartburn. This first occurred four weeks ago when he noticed epigastric pain with acid-reflux causing a sore throat in his mouth following a meal. At the time of presentation, he claimed that the only discomfort that he experienced was tenderness and pain in his epigastric region. He complained of no altered bowel habits, sweating, dysphagia or generalised weakness. There was no history of non-steroidal anti-inflammatory drug (NSAID) use or recent infections. A neighbour advised him to try a popular heartburn remedy so he went to his local pharmacy and tried an over-the-counter medication (Gaviscon ®). This only improved his symptoms minimally. The patient’s past medical history is significant for hypertension, diagnosed two years ago which is now well controlled with medication. He used to drink around two to four cups of coffee per day which he claims he has now reduced to one cup per day. He has no history of smoking and only drinks socially. Following his consultation, the patient was subsequently further investigated for a Helicobacter pylori infection, and the test returned with a positive result. He was started on triple therapy to eradicate his Helicobacter pylori infection and his treatment regimen was successfully completed. He has now returned for a review and states that he is still suffering from heartburn and indigestion. What is the most appropriate test to ensure the eradication of Helicobacter pylori?
Correct Answer : C
It is only necessary to check for the eradication of Helicobacter pylori in patients whose symptoms return. In this case, the patient tested positive for Helicobacter pylori and started on triple therapy. His history shows that his compliance was good and that he successfully finished his treatment.
However, he still complains of indigestion. So the issue in this question is to choose the single best test that will confirm the eradication of Helicobacter pylori.
We know that the answer is a urea breath test as that is the only test that NICE recommends post-eradication, but is the answer a C13 urea breath test or a C14 urea breath test.
The urea breath test is the only current valid method for detecting eradication of Helicobacter pylori infection. Urea can be labeled with two different carbon isotopes: C14 and C13.
The main difference between them is that the former is radioactive, whereas the latter is stable. The C13 urea breath test is the recommended test to perform. This is because it is a non-radioactive isotope that can be used safely for repeated testing, which is frequently required in clinical practice. Endoscopy is only required if H. pylori is completely eradicated, as shown by urea breath testing, to further investigate the cause of dyspepsia.
Q.56. A 54 year old man presents with a worsening history of intermittent dysphagia over a period of 3 months. He has not experienced any weight loss and complains of sometimes regurgitating food, after which he says he experiences a feeling of great relief. He has a history of recurrent respiratory tract infections over the past few years. He is a non smoker. What is the most likely diagnosis?
Correct Answer : A
Note that in achalasia the symptoms can also be intermittent. It usually presents with gradually progressive, intermittent dysphagia. The dysphagia associated with oesophageal carcinoma is more rapid than achalasia. In achalasia, they may have a history of recurrent respiratory tract infections like in this stem.
Q.57. A 39 year old woman is admitted with central abdominal pain radiating through to the back. She has vomited several times in the last 24 hours. She denies any diarrhoea. Bending forward helps alleviate the pain. On examination, there is epigastric tenderness associated with guarding. She has a blood pressure of 100/70 mmHg, a respiratory rate of 20 breaths/minute, a pulse rate of 106 beats/minute and a temperature of 37.9 C. Her blood test show: Amylase 1335 U/mL (Elevated) CRP 214 mg/L White cell count (WCC) 19.6 x 109/L What is the best step in management?
Correct Answer : A
The likely diagnosis is acute pancreatitis given the elevated amylase. The initial treatment for acute pancreatitis is supportive and includes early fluid resuscitation, analgesia, and nutritional support. Parenteral nutrition is only used when the enteral route is not tolerated, or if it is not meeting specific caloric requirements. Surgical debridement may be required where there is proven infection and necrosis.
Note that laparoscopic surgical debridement has largely been replaced by newer minimally invasive techniques such as transgastric endoscopy and video-assisted translunar retroperitoneal necrosectomy followed by closed lavage of infected pancreatic necrosis so urgent laparoscopy is not the answer here. Also, remember that there needs to be some evidence of necrosis before surgical debridement is considered.
Intravenous antibiotics (e.g. IV imipenem) can be started in moderate to severe cases even without evidence of infected necrosis. This should preferably follow percutaneous aspiration of peritoneal fluid for culture however in this case, fluid resuscitation, analgesia and nutritional support are more important than just antibiotics. 60% of acute pancreatitis in adults are due to gallstones and thus cholecystectomy can be considered but should only be considered after the initial symptoms of acute pancreatitis have resolved.
Q.58. A 38 year old man complains of “crushing” chest discomfort for 1 hour that started when he drank a cold drink. He has no significant medical history. ECG shows sinus rhythm. He is given sublingual nitroglycerin in the emergency room that improves his chest pain almost immediately. He has a pulse of 70 beats/minute, a blood pressure of 130/80 mmHg and a respiratory rate of 18 breaths/minute. Cardiac enzymes came back negative. What is the most likely diagnosis?
Correct Answer : B
The pain started when he drank a cold drink. The most likely answer here is an oesophageal spasm.
Q.59. A 28 year old female presents with a 4 month history of diarrhoea, lethargy and weight loss. She complains of abdominal discomfort and passing stools more than 6 times a day. An endoscopy was performed which shows cobblestone mucosa. What is the most likely diagnosis?
Correct Answer : C
The diagnosis of Crohn’s disease is quite clear here. Lethargy and weight loss are nonspecific signs that can occur in Crohn’s disease. The giveaway here is the cobblestone mucosa that is seen on endoscopy which is pathognomic for Crohn’s disease.
Q.60. A 64 year old man presents to the clinic with lethargy and a dull pain in the right hypochondrium that has been worsening over the past for a few months. He has significant weight loss over the last several weeks. On examination, he is noted to have a slight yellow tinge of his skin and whites of his eyes. Abdominal palpation reveals a tender right upper quadrant with a firm, enlarged liver. Further investigations were performed over the next few weeks. The histology of his liver biopsy returns with the report showing evidence of adenocarcinoma and immunostaining of Thyroid transcription factor 1 (TTF-1) which indicates a primary pulmonary tumour. What is the most likely route of metastases in this patient?
Correct Answer : C
Haematogenous spread to the liver from the lung is the most common route of metastases. TTF-1 is a protein seen by immunostaining which is used as a clinical marker of lung adenocarcinoma.
Q.61. A 39 year old patient was recently diagnosed with coeliac disease and has been treated with a gluten free diet for 2 years. He now has an exacerbation of the classic symptoms of coeliac disease such as abdominal pain, diarrhoea, and has loss significant weight. The biopsy of the small intestine shows lymphomatous infiltrates. What is the most likely diagnosis?
Correct Answer : A
Enteropathy-associated T-cell lymphoma (EATL) is a celiac disease (CD) complication. This tumor derives from the neoplastic transformation of aberrant intraepithelial T lymphocytes emerging in coeliac patients unresponsive to a gluten-free diet.
The biopsy may show lymphomatous infiltrates accompanied by a prominent mixed-inflammatory infiltrate composed of histiocytes, small lymphocytes, plasma cells, and eosinophils, which may obscure the neoplastic cells. Just keep in mind that lymphoma should be at the top of the list of answers when you see a patient with coeliac disease in the exam.
Q.62. A 41 year old man with type 2 diabetes mellitus presents to the clinic with complaints of pain in his joints and an unusual increase in breast size. He feels increasingly fatigued over the past few months. On examination, there is a deep tan color of his skin and his liver is enlarged on palpation. What is the most likely diagnosis?
Correct Answer : A
The deep tan color of the skin with the combination of diabetes is termed “bronze diabetes”: and it is seen in haemochromatosis. Iron overload can also cause symptoms of arthropathy and gynaecomastia.
Q.63. A 56 year old woman has had severe abdominal pain for 24 hours radiating to her back and is accompanied by nausea and vomiting. She denies any diarrhoea or fever. She appears to be tachycardia and in shock. She has a history of gallstones. What is the most likely investigation to confirm the diagnosis?
Correct Answer : A
Please see Q-17
Q.64. A 60 year old man presents with weight loss and complains of mild abdominal pain, bloating and diarrhoea for the past 6 months. A recent blood test shows a haemoglobin of 7 g/dl. What is the most appropriate investigation?
Correct Answer : D
A colonoscopy would be able to diagnose the majority of the causes of changes in bowel habits and weight loss. The likely diagnosis here is colorectal cancer although inflammatory bowel disease could also present with similar features (e.g. weight loss, abdominal pain, and anaemia). Whatever the cause, a colonoscopy and biopsy is the gold standard to give us a diagnosis. Colonoscopy is still the preferred diagnostic investigation.
Alternatives to colonoscopy include barium enema and CT colonography. If a patient is without major comorbidities, a colonoscopy should be offered to diagnose colorectal cancer.
If a lesion suspicious of cancer is detected, a biopsy sample should be sent for histology. Flexible sigmoidoscopy, then barium enema can be used as an alternative to colonoscopy for patients with major comorbidity. Barium enema may also be used if a colonoscopy fails to visualize the caecum or if the patient is unable to tolerate the colonoscopy procedure.
Computed tomographic (CT) colonography can also be used as an alternative if the local radiology service can demonstrate competency in this technique. If a lesion suspicious of cancer is detected on CT colonography, a colonoscopy with biopsy to confirm the diagnosis should be performed. The tumour marker Carcinoembryonic Antigen (CEA) is of no use for diagnosis or staging but can be used to monitor disease relapse if raised at diagnosis and falls to normal after resection.
Q.65. A 38 year old man has just returned from Kenya a few days ago. Since his return, he has developed watery diarrhoea with crampy abdominal pain. What is the most likely causative organism?
Correct Answer : C
The most common organism that causes traveler’s diarrhoea is E. coli. It will usually cause mild self-limiting diarrhoea for less than 72 hours.
Q.66. A 44 year old man who has attended the Emergency Department multiple times in the past several months with complaints of upper abdominal pain. He develops episodes of pain lasting for weeks. There has been a gradual rise in his amylase on every visit. He has had a variety of investigations to explore the cause during his previous visits. These included gastroscopy and an ultrasound which was found to be normal. On examination, his abdomen is soft and mildly tender at the epigastrium. What is the most likely cause of his abdominal pain?
Correct Answer : B
Around 80% of chronic pancreatitis results from alcohol excess in developed countries. Given his recurrent presentation over several months, we can say this is chronic. Patients with chronic pancreatitis usually have constant and relapsing episodes of upper abdominal pain lasting for days or weeks. He would likely go on to have a CT scan of his abdomen as the CT of the pancreas is often the imaging modality of choice. Cystic fibrosis is incorrect.
This is a genetic disorder that affects people from birth and is associated with respiratory complications. Furthermore, sadly most sufferers will not live beyond the age of 30 years.
CHRONIC PANCREATITIS :
• Alcohol - seen in the majority of cases
• Smoking
• Autoimmune
Clinical features :
• Classically presents with epigastric pain radiating into the back
o Pain is relieved when sitting forward
o Pain is the most common presentation of chronic pancreatitis
o Pain is episodic with short periods of severe pain
o Eating may exacerbate the pain
• Steatorrhoea
o Steatorrhoea occurs due to the malabsorption of fats from the lack of pancreatic lipase secretion which could subsequently cause weight loss
o Occasionally, the question writers may use words like “offensive stools which are difficult to flush” which in other words represent the term steatorrhoea.
o This is a later presentation due to obstruction of the common bile duct when the head of the pancreas becomes fibrosed. Remember, patients with chronic pancreatitis seek medical attention mainly because of symptoms of abdominal pain or maldigestion and weight loss.
Investigations :
• Serum lipase and lipase
o May be slightly elevated however in contrast to acute pancreatitis, the serum amylase and lipase levels are not strikingly elevated
• Transabdominal ultrasound scans
o Often as part of the initial assessment
• Contrast-induced spiral CT scan
o Remains the gold standard for imaging technique for pancreatic disease
o Shows evidence of pancreatic calcification
Management - Think of the individual clinical features and how to manage them
• Pain – analgesia
• Steatorrhoea or malabsorption – Pancreatic enzymes supplements and fat-soluble vitamins
• Diabetes – oral hypoglycaemics and insulin
Q.67. A 27 year old woman comes to the hospital with pain and distension of her abdomen. The pain started a few days ago and it has been worsening over the past 24 hours. She gives a history of recent bloody diarrhoea. She has been suffering with chronic diarrhoea and abdominal cramping for a few months associated with fever and malaise. Her diarrhoea is often episodic with periods where she has normal stool consistency for a few days however she feels greatly inconvenient during episodes where she has increased frequency of defecation. An erect abdominal X-ray was requested and performed which shows mucosal oedema and a dilated transverse colon. Her temperature is 38.5 C. She has a pulse rate of 105 beats/minute and a blood pressure of 100/60 mmHg. Her blood results show: White cell count (WCC) 16.3 (4-11 x 109/L) CRP 125 mg/L (< 10 mg/L) Haemoglobin 100 g/L (115-160 g/L) What is the most likely diagnosis?
Correct Answer : D
Ulcerative colitis is often episodic and presents with chronic diarrhoea that can be bloody. Systemic symptoms include fever and malaise. In moderate to severe attacks, blood tests would show raised white blood cells and CRP with anaemia (iron deficiency anaemia).
The features that she presents within the hospital are consistent with a toxic megacolon. This is characterized by a very dilated colon accompanied by abdominal distension, abdominal pain, and in some cases shock. Toxic megacolon is one of the well-known complications of ulcerative colitis.
Q.68. A 32 year old woman complains of brief episodes of severe shooting pain in the rectum that usually occur at night. Rectal examination and flexible sigmoidoscopy detect no abnormalities. What is the most probable diagnosis?
Correct Answer : B
A normal rectal examination and flexible sigmoidoscopy exclude the other options. Only proctalgia fugax is left.
Proctalgia fugax - Severe recurrent rectal pain in the absence of any organic disease. Attacks may occur at night, after bowel actions, or following ejaculation. Anxiety is said to be an associated feature.
Q.69. A 43 year old lady presents with jaundice. Skin excoriations were seen on physical examination. Blood test reveals a raised alkaline phosphatase with mildly raised alanine transaminase. Antimitochondrial antibodies are found to be positive. What is the most likely diagnosis?
Correct Answer : C
The diagnosis here is primary biliary cirrhosis. The classic presentation is itching in a middle-aged woman as we see here. Often asymptomatic and diagnosed after finding alkaline phosphatase on routine LFT. Lethargy, sleepiness, and pruritus may precede jaundice. There is an association with Sjögren syndrome.
Antimitochondrial antibodies (AMA) are the hallmark of this disease.
To help remember: Think of the M rule for Primary biliary cirrhosis.
• IgM
• anti-Mitochondrial antibodies
• Middle-aged females
PRIMARY BILIARY CIRRHOSIS VS PRIMARY SCLEROSING CHOLANGITIS :
Primary Biliary Cirrhosis :
• Autoimmune, idiopathic
• Association - Sjogren
• Pruritus, raised ALP
• Antimitochondrial antibody (AMA) positive
• Management involves ursodeoxycholic acid, cholestyramine
Primary Sclerosing Cholangitis :
• Autoimmune, idiopathic
• Association - IBD (especially UC)
• Pruritus, raised ALP
• ERCP is the most specific test
• Management involves ursodeoxycholic acid, cholestyramine
Q.70. A 12 year old child complains of right iliac fossa pain and diarrhoea. On colonoscopy, a transmural, cobblestone appearance mucosa is seen near the ileo-caecal injection. What is the most appropriate management?
Correct Answer : D
The diagnosis of Crohn’s disease is quite clear here. A transmural, cobblestone appearance mucosa is a giveaway that this is Crohn’s disease.
Q.71. A 25 year old woman has diarrhoea and abdominal bloating over the last 4 months. On examination, she has blistering rash over her elbows. Her blood test show: Haemoglobin 105 g/L Mean cell volume (MCV) 79 fL On jejunal biopsy, there is shortening of the villi and lymphocytosis. What is the most likely diagnosis?
Correct Answer : A
The blistering rash over her elbows is called dermatitis herpetiformis. Dermatitis herpetiformis, is a skin condition linked to coeliac disease.
Typical symptoms of dermatitis herpetiformis are red, raised patches, often with blisters and severe itching. The low haemoglobin is another clue towards coeliac as one of the most common presentation of coeliac disease is iron deficiency anaemia. Folate and B12 deficiency can also occur.
The shortening of villi (villous atrophy) and lymphocytosis on jejunal biopsy is provides us with the diagnosis of coeliac disease. One may be thinking of tropical sprue as a diagnosis as it also has villous atrophy on jejunal biopsy and has a similar presentation.
But tropical sprue does not present with dermatitis herpetiformis and it is also much rarer as compared to coeliac disease.
Q.72. A 40 year old woman complains of dysphagia when eating solids and drinking liquids. She sometimes suffers from severe retrosternal chest pain. Barium swallow reveals a dilated oesophagus which tapers to a fine distal end. What is the most appropriate management?
Correct Answer : C
Please see Q No-11
Q.73. A 25 year old woman complains of diarrhoea, and abdominal cramps for the past 8 months. She says that her diarrhoea has recently become bloody. A biopsy was performed and the colonic mucosa shows crypt abscesses. What is the most likely diagnosis?
Correct Answer : A
Crypt abscesses (Crypts of Lieberkühn) are typical of ulcerative colitis, though not diagnostic. They are mucosal crevices that are seen in the normal gastrointestinal tract. In ulcerative colitis, these get clogged up with neutrophilic exudates, forming “crypt abscesses.” These are not “real” abscesses and do not require surgical drainage. It is important to know the differences between ulcerative colitis and Crohn’s disease as it is very commonly asked.
Q.74. What is the pathological change in Barrett's esophagus?
Correct Answer : D
Barrett’s oesophagus results from prolonged exposure of normal oesophageal squamous epithelium to the refluxate of GORD. This causes mucosal inflammation and erosion, leading to the replacement of the mucosa with metaplastic columnar epithelium. The most significant associated morbidity is oesophageal adenocarcinoma.
Q.75. A 48 year old woman is admitted to A&E with a productive cough and moderate fever. She complains of central chest pain and regurgitation of undigested food. She finds it difficult to swallow both food and liquids. These symptoms of swallowing have been present for the last 4 months. A chest X-ray shows megaesophagus. What is the most likely diagnosis?
Correct Answer : B
The diagnosis here is Achalasia. It can sometimes present as chest pain. The productive cough in this question points towards aspiration pneumonia secondary to retained food and fluid in the oesophagus. Regurgitation of undigested food and difficulty swallowing both food and liquids are classic for achalasia.
A chest X-ray would also show a large oesophagus in Achalasia.
While some might argue that the answer here could potentially be the pharyngeal pouch due to the regurgitation of undigested food and aspiration pneumonia. Question would provide other hints if a pharyngeal pouch was the answer such as halitosis which may occasionally be seen in a pharyngeal pouch. Furthermore, the megaesophagus points towards achalasia as being the answer to this question.
Q.76. A 58 year old man has a history of moderate to severe recurrent epigastric pain at night for the past month. He has no history of peptic ulcers diagnosed previously and has no previous investigations for dyspepsia. He is not on any regular medications. What is the most appropriate investigation that would lead to a diagnosis?
Correct Answer : D
In previous recommendations, patients aged 55 years or older with unexplained and persistent recent-onset dyspepsia should be referred urgently for endoscopy. In recent years, the recommendations have changed to consider routine endoscopic investigations in patients over the age of 55 where symptoms persist despite Helicobacter pylori testing and acid suppression. Since this question is asking for an investigation that would lead to a diagnosis, endoscopy is the best answer to investigate a peptic ulcer.
Q.77. A 75 year old man living in a nursing home is taken to the hospital by his nurse. He has been suffering from longstanding constipation and has been having difficulty in passing stools for the past 7 days. He appears mildly confused and agitated. He has a heart rate of 110 beats/minute and a respiratory rate of 30 breaths/minute. On rectal examination, faecal impaction is noted. What is the most appropriate management?
Correct Answer : A
If constipation is not treated and is left to manifest for a long period, it can result in the development of faecal impaction whose symptoms may be seen as dehydration, tachycardia, tachypnoea, agitation, and confusion if severe. A person with faecal impaction may require emergency treatment or hospitalization.
For rapid action, phosphate enema is preferred. Phosphate enemas contain sodium acid phosphate and sodium phosphate. The osmotic activity of the former increases the water content of the stool so that rectal distension follows and it is thought that this induces defecation by stimulating rectal motility. It has a very quick onset of action which makes enemas useful for when a rapid evacuation of a stony dull faecal impaction is required.
Q.78. A 23 year old woman has abdominal bloating, weight loss and intermittent diarrhoea. She describes her stools as “frothy” and difficult to flush down the toilet. Her blood test show: Haemoglobin 105 g/L White cell count 7.1 x 109/L Platelets 350 x 10 9/L Ferritin 11 ng/ml Vitamin B12 225 ng/L Folate 1.9 mcg/L Endomysial antibodies were tested positive. What is the most likely diagnosis?
Correct Answer : C
The anaemia and low ferritin and folate levels are characteristic of coeliac disease. This is in combination with the endomysial antibodies. A jejunal biopsy should be done to confirm this diagnosis.
Q.79. A 44 year old male is admitted with repeated attacks of pancreatitis. He has peripheral paraesthesia and loss of proprioception in the legs. He is having memory loss and difficulties with thinking. What is the most appropriate management?
Correct Answer : B
Inadequate vitamin B12 absorption can be due to chronic pancreatitis. Neuropsychiatric features of B12 deficiency include dementia which is why he is having memory loss and difficulties with thinking. Peripheral paraesthesia and disturbances of position and vibration sense are classically seen in B12 deficiency. Treat with hydroxocobalamin.
Q.80. A patient complaints of lethargy, weight loss and history of bloody diarrhoea. He underwent endoscopy that showed skip lesions & deep ulcers. What is the diagnosis?
Correct Answer : A
The diagnosis of Crohn’s disease is quite clear here. Lethargy and weight loss are nonspecific signs that can occur in Crohn’s disease. The giveaway here is the deep ulcers, and skip lesions that are seen on endoscopy which is pathognomic for Crohn’s disease. Note that although Crohn’s disease usually has non-bloody diarrhoea, it occasionally may present with bloody diarrhoea.
Q.81. A 55 year old man develops fatigue and palpitations. He had a gastrectomy a years ago. Recent blood tests were ordered which show: Haemoglobin 98 g/L Mean cell volume (MCV) 110 fL On neurological examination, loss of proprioception and vibration sense were noted. What is the most likely diagnosis?
Correct Answer : C
High MCV and low Hb – Macrocytic anaemia.
These findings together with a history of ileal resection whereby malabsorption of B12 could occur, point towards the diagnosis of B12 deficiency.
Q.82. A 59 year old man has multiple liver metastasis with the primary tumour originating from the large bowel. He has abdominal pain, and jaundice. On general inspection, he looks cachexic and drowsy. He has significant ascites and oedema seen on both ankles. His family have concerns that he is not having sufficient fluids orally. His urine output is slow. He currently takes regular haloperidol 1.5 mg three times a day and lactulose 10mltwice a day. His blood test show: Serum urea 6.2 mmol/L Serum creatinine 85 ?mol/L Sodium 129 mmol/L Calcium 2.42 mmol/l Potassium 3.6 mmol/l Albumin 18 g/L Bilirubin 105 mol/L Alkaline phosphatase (ALP) 411 U/L What is the most appropriate management?
Correct Answer : C
This patient has hypoalbuminaemia. When plasma proteins, especially albumin, no longer sustain sufficient colloid osmotic pressure to counterbalance hydrostatic pressure, oedema, and ascites develops. Intravenous albumin may be used to increase a colloid osmotic pressure to draw fluid back into the intravascular compartment to reduce oedema and ascites.
It restores intravascular plasma volume with less exacerbation of salt and water overload than isotonic solutions. Albumin infusion produces only a transient effect but it is useful in cases like this where surgery may not be an option and treatment of intravascular fluid deficit and oedema is required. It is also useful to obtain diuresis in hypoalbuminaemia patients. Haloperidol has no role in causing hypoalbuminaemia.
Q.83. A 34 year old man presents with slow progressive dysphagia. He has been using H2blockers for the last year because of retrosternal discomfort. He has not noticed any weight loss. A haemoglobin level was done a month ago which reads 13.3g/dL. What is the most likely diagnosis?
Correct Answer : A
Peptic strictures have an association with gastro-oesophageal reflux disease and can cause dysphagia. The fact that there is no weight loss and haemoglobin is normal points towards a benign cause. Esophageal cancer in this age group is also uncommon.
Q.84. A 30 year old lady complains of intermittent diarrhoea, chronic abdominal pain and tenesmus. Sometimes she notices blood in her stool. What is the most likely cause of her symptoms?
Correct Answer : C
Inflammatory bowel disease remains the best choice among the rest. All the symptoms stated in the question including tenesmus can occur in inflammatory bowel disease. The answer is unlikely to be diverticulosis as diverticulosis is defined as the presence of asymptomatic diverticula. This patient has symptoms. Blood in stools is not seen in irritable bowel disease. Remember, passing blood is not a symptom of IBS. The symptoms are not at all consistent with adenomyosis or endometriosis.
Q.85. A 35 year old woman has sudden onset epigastric pain, chills and nausea. She gave birth to a health baby 2 days ago. Her blood pressure was normal throughout pregnancy. Her temperature is 37.3°C and her blood pressure is 139/90 mmHg. Urinalysis reveals no proteins. Her blood test show: Alkaline phosphatase (ALP) 420 U/L Alanine transferase (ALT) 650 U/L Bilirubin 25 ?mol/L International normalized ratio (INR) 1.0 Haemoglobin 101 g/L Platelets 350 x 109/L White cell count (WCC) 13.5 x 109/L What is the most likely diagnosis?
Correct Answer : D
The history of sudden onset epigastric pain, chills, and nausea in the postpartum period with a likely history of an uneventful pregnancy make cholecystitis the most likely diagnosis. Symptomatic gallstone disease is the second most common abdominal emergency in pregnant women. Pregnancy alters bile composition and gallbladder emptying slows in the second trimester, increasing the risk of gallstones. The raised ALT is of something to note. The causes of raised liver enzymes in the postpartum period is endless.
They include:
• Pregnancy-related liver diseases such as:
o Obstetric cholestasis
o Pre-eclampsia, eclampsia,
o HELLP syndrome
o Acute fatty liver of pregnancy
o Viral hepatitis
o Autoimmune liver disease
o Wilson’s disease
o Budd-Chiari syndrome
o Acute cholecystitis
o Drug-induced hepatotoxicity
As there is no protein in the urine and blood pressure has been normal throughout pregnancy, pre-eclampsia is unlikely. As haemoglobin levels and platelet levels are within a normal range for someone who has just delivered a baby, HELLP syndrome is unlikely. Obstetric cholecystitis may have aminotransferase levels as high as 20 times the normal limits, but the raised bile acids would cause significant pruritus which would be the main presenting feature rather than epigastric pain. Biliary colic occurs when a stone temporarily occludes the cystic duct. There is a colicky pain in the right upper quadrant radiating to the right shoulder.
The episode is usually self-limiting. Ultrasound establishes the diagnosis of gallstones. The diagnostic accuracy of ultrasound for detecting gallstones is 95%. The main difference between biliary colic and acute cholecystitis is the inflammatory component. In acute cholecystitis, there is local peritonism, fever, and elevated WCC.
Q.86. 55 year old man comes to the Emergency Department with 3 episodes of haematemesis and epigastric pain and is currently waiting for investigations. He has a history of rheumatoid arthritis for which he takes non-steroidal anti-inflammatory drugs. He has a pulse rate of 70 beats/minute and his blood pressure is 120/80. What is the most appropriate management?
Correct Answer : B
This man has a peptic ulcer disease which is causing his upper GI bleeding. Part of the management involves resuscitation with intravenous fluids, intravenous analgesia, antiemetics, and intravenous PPI if known peptic ulcer disease. Intravenous antibiotics are only considered prophylactically if we are considering upper GI bleeding from varices or a perforated peptic ulcer. There is no reason to administer fresh frozen plasma or intravenous steroids in this stem.
Q.87. A 23 year old female presents with an 8 week history of bloody diarrhoea. She says her bowels have not been right for the past few months and she frequently has to run to the toilet. A diagnosis of ulcerative colitis is made. What is the most likely sign to be seen on a barium enema?
Correct Answer : A
Loss of haustration is pathognomonic for Ulcerative Colitis. Cobblestone appearance is seen on an endoscopy for Crohn’s disease. Kantor's string sign rose thorn ulcers, and fistulae are seen on a small bowel enema in Crohn’s disease.
Q.88. A 43 year lady had endoscopic retrograde cholangiopancreatography for gallstone disease. Twenty-four hours after the procedure she returns to the emergency department with severe right upper quadrant pain. On examination, she appears generally unwell with a pyrexia of 38.9 C. She looks yellow and she is extremely tender in the right upper side of her abdomen. What is the most likely diagnosis?
Correct Answer : C
The correct answer is option C. Ascending cholangitis.
This is a classical presentation with Charcot’s triad of fever, RUQ pain, and jaundice. Abdominal sepsis is one of the three most common types of sepsis, particularly as this lady recently had a procedure at the time of presentation and is most suspicious of an infective pathology.
Acute pancreatitis is incorrect as this typically / classically presents with profuse vomiting and central (umbilical) abdominal pain that radiates under the ribs.
This distribution of pain relates to the embryonic origins of the pancreas which is the midgut. Acute cholecystitis is incorrect as although it is a good differential given the presentation, it is not the single best answer given the history of jaundice. Jaundice is not typically present in cholecystitis.
Cancer of the head of the pancreas is incorrect as there is nothing in the question to suggest a malignant pathology such as weight loss.
Furthermore, the classic presentation of cancer of the head of the pancreas is ‘painless jaundice’.
Option E. Upper GI perforation is incorrect as this usually presents with generalized abdominal tenderness with guarding and the patient will typically be much more unwell. This is a good differential to keep in mind as the patient did just have a recent endoscopy.
However, if a perforation had occurred, the patient would have become unwell immediately at the time of the event, not twenty-four hours later!
Q.89. A 41 year old lady attends the clinic complaining of a long history of mild pruritus and fatigue. She looks jaundiced. Alkaline phosphatase was raised on routine liver function test. She was diagnosed with Sjögren syndrome a few years back. What is the most appropriate test to perform to help make a diagnosis?
Correct Answer : A
The diagnosis here is primary biliary cirrhosis. The classic presentation is itching in a middle-aged woman as we see here. Often asymptomatic and diagnosed after finding alkaline phosphatase on routine LFT. Lethargy, sleepiness, and pruritus may precede jaundice. There is an association with Sjögren syndrome. Antimitochondrial antibodies (AMA) are the hallmark of this disease.
Q.90. An 83 year old woman who is a resident in a nursing home is admitted to a hospital with a 4 day history of chronic constipation. She has had no weight loss or change in appetite. She has been on analgesics for 3 weeks for her back pain. She is in obvious discomfort. Rectal examination reveals faecal impaction with hard stools. What is the most appropriate immediate management?
Correct Answer : D
This is an example of overflow diarrhoea. Medications such as opioid pain relievers reduce intestinal movement and may cause faecal matter to become too large, hard, and dry making it difficult to expel. Subsequently, faeces become so hard that they cannot be expelled and faecal fluid will flow around the block.
Phosphate enemas contain acid phosphate and sodium phosphate. The osmotic activity of the former increases the water contact of the stool so that rectal distension follows and it is thought that this induces defecation by stimulating rectal motility.
It has a very quick onset of action which makes enemas useful when a rapid evacuation of a stony dull faecal impaction is required. Phosphate enema is the clear answer here as the question addresses the immediate management. It is important to remember the relation between elderly, bedridden individuals and faecal impaction.
Fecal impaction is a fairly common complication of long-term constipation in the elderly and bedridden, occurring in about 30% of all nursing home residents. Hence in the exam, it is likely they would have the words, “Nursing home” in the stem.
Faecal impaction If the patient has faecal impaction, try:
• Bisacodyl suppositories
• Arachis oil retention enema to soften
• Phosphate enema
• An alternative is polyethylene glycol, Movicol taken for three days
• Manual removal (with midazolam, morphine, or caudal anaesthesia)
• Once successful it is imperative to start regular oral measures to prevent recurrence of the problem.
Q.91. A 33 year old woman has severe upper abdominal pain with radiation to the back within 24 hours of removing gallstones by endoscopic retrogradecholangiopancreatography (ERCP). The pain is eased when she leans forward. She reports some nausea and vomiting but denies any diarrhoea. Jaundice is noted and the epigastric region is tender on palpation. Her blood pressure is 120/80 mmHg, and temperature is 37.3°C. What is the most likely reason for his signs and symptoms?
Correct Answer : A
The likely cause is acute pancreatitis. Pancreatitis is one of the most frequent post-ERCP complications. The incidence of this is around 20%. Ascending cholangitis may have a similar presentation but given that she is apyrexial, the likely cause is acute pancreatitis. Note that even in acute pancreatitis, mild pyrexia is common.
Q.92. A 21 year old woman complains of diarrhoea, and abdominal cramps for the past 5 months. She says that her diarrhoea has recently become bloody. A rectal biopsy was performed and histology was reported as “decreased amounts of goblet cells”. What is the most likely diagnosis?
Correct Answer : C
The diagnosis of ulcerative colitis is quite clear here. Decreased goblet cells on histology points towards ulcerative colitis.
Q.93. A 60-year-old man presents with dysphagia and pain on swallowing both solids and liquids. A barium meal shows gross dilatation of the esophagus with a smooth narrowing at the lower end of the oesophagus. What is the most likely cause of dysphagia?
Correct Answer : A
Achalasia Cardia is a primary motility disorder of the esophagus characterized by peristalsis and defective lower esophageal sphincter relaxation.
The pathogenesis of achalasia cardia is poorly understood. However recent evidences indicate that it is an autoimmune process triggered by some virus (e.g. herpes virus) in a genetically predisposed individual resulting in degeneration of myenteric neurons.
Dysphagia for both solid and liquid or prominently liquid suggests achalasia whereas dysphagia to solid suggests stricture. Also, gross dilatation of oesophagus with smooth narrowing at the lower end is seen in achalasia.
In achalasia, dysphagia is usually described as progressive. The standard of care in patients with achalasia has been pneumatic balloon dilatation and laparoscopic Heller's myotomy. Per oral endoscopic myotomy (POEM) is a novel minimally invasive treatment option for all types of achalasia cardia.
Q.94. A 64-year-old patient has been having frequent episodes of secretory diarrhea, which is extremely watery, with large amounts of mucus. A diagnosis of villous adenoma was made after endoscopy. What electrolyte abnormality is most likely in this patient?
Correct Answer : D
Villous adenoma can cause both hyponatremia and hypokalemia but out of these, better to choose D.
Q.95. A 32-year-old man presented with slow progressive dysphagia. There is past history of retro-sternal discomfort and he has been treated with prokinetics and H2 blockers. What is the probably diagnosis?
Correct Answer : C
Progressive dysphagia (to mostly solid) is suggestive of peptic stricture which is supported here by the use of prokinetic drugs and H2 blockers which are used for reflux oesophagitis.
Q.96. A woman who returned from abroad after 3 weeks of holiday complains of severe diarrhea of 3 weeks. She also developed IDA (Iron Deficiency Anaemia) and folic acid deficiency. What condition best describes her situation?
Correct Answer : C
Acute gastroenteritis (may be due to bacteria, virus or parasite) may cause transient malabsorption, probably as a result of temporary, superficial damage to the villi and microvilli.
Q.97. A 55-year-old man has had severe pain in the right hypochondrium for 24 hours. The pain comes in waves and is accompanied by nausea. Nothing seems to relieve the pain. He feels hot and sweaty but has normal temperature. What is the most appropriate next investigation?
Correct Answer : A
The features like :
i) severe right hypochondrial pain
ii) colicky nature of the pain (comes in waves)
iii) nausea
iv) absence of fever
iv) absence of jaundice favours diagnosis of biliary colic and the most appropriate next investigation is the US abdomen.
Q.98. A 48-year-old woman is admitted to emergency department with a productive cough and moderate fever. She has often central chest pain and regurgitation of undigested food most times but doesn’t suffer from acid reflux. These symptoms have been present for the last 3.5 months which affects both food and drink. A CXR shows an air-fluid level behind a normal sized heart. What is the most likely diagnosis?
Correct Answer : D
Points in favour of achalasia:
Aspiration pneumonia due to retained food and fluid in oesophagus. In achalasia usually, there is no acid reflux.
Dysphagia for both food and drink. Air-fluid level behind the heart.
This is not a hiatus hernia because
i) In a hiatus hernia usually you will get associated GORD
ii) Also in a hiatus hernia there may be nausea or vomiting.
This is not a pharyngeal pouch as there is no halitosis.
Q.99. A 35-year-old man presents with history of dyspepsia. H.Pylori antibodies are negative. No improvement is seen after 1 month of treatment. What is the next step?
Correct Answer : B
Not responding to treatment D/D is:
i) Zollinger Elison syndrome
ii) Ca stomach.
Indications of gastroscopy in a 35 yo man (for men of age <50) :
i) Acute symptoms with H/O previous episode (PUD)
ii) Alarm features : weight loss, anaemia, vomiting, hematemesis and melaena, dysphagia, palpable abdominal mass), fear of cancer, evidence of organic disease.
Q.100. A 79-year-old lady who is otherwise well recently started abdominal pain. She is afebrile and complains that she passed air bubbles during urination. A urethral catheter showed fecal leakage in the urinary bag. What is the likely pathology?
Correct Answer : B
D/D is rectosigmoidal tumour. As there are no constitutional features of cancer like anorexia, weight loss, or fever rectosigmoid tumour is unlikely.
Crohn’s disease can occur at any age but is most frequently diagnosed in people ages 15 - 35. About 10% of patients are children under age 18.
So Crohn’s disease can occur in this age also and the feature like fistula is a common association of CD.
Q.101. A young woman complains of diarrhea, abdominal cramps and mouth ulcers. Abdominal X-ray shows distended transverse colon with globet cell depletion on rectal biopsy. What is the most probable diagnosis?
Correct Answer : B
In UC there is goblet cell depletion and less mucous production in contrast with CD where there may be goblet cell hyperplasia and mucous secretion is not reduced. Please note aphthous ulcers can develop in both CD and UC.
Q.102. A 28-year-old female presents with a 3 months history of diarrhea. She complains of abdominal discomfort and passing stool 20 times/day. Examination: febrile. Barium enema shows cobblestone mucosa. What is the most likely diagnosis?
Correct Answer : D
History of diarrhea, abdominal discomfort, and patient being febrile indicate gut inflammation and cobblestone appearance on barium enema is diagnostic of CD.
Q.103. A-60 year-old woman presented to OPD with dysphagia. No history of weight loss or heartburn. No change in bowel habits. While doing endoscopy there is some difficulty passing through the LES (lower esophageal sphincter), but no other abnormality is noted. What is the most useful investigation?
Correct Answer : D
Diagnosis is achalasia.
Characteristic manometric findings are: Lower esophageal sphincter (LES) fails to relax upon wet swallow (<75% relaxation) Pressure of LES <26 mm Hg is normal,>100 is considered achalasia, > 200 is nutcracker achalasia.
Q.104. What is the pathological change in Barret’s esophagitis?
Correct Answer : A
Both A and D are the correct answer as Barrett’s oesophagus is a change known as metaplasia.
Q.105. A 55-year-old woman complains of retrosternal chest pain and dysphagia which is intermittent and unpredictable. The food suddenly sticks in the middle of the chest, but she can clear it with a drink of water and then finish the meal without any further problem. A barium meal shows a ‘corkscrew esophagus’. What is the most likely cause of dysphagia?
Correct Answer : C
Chest pain, unpredictable intermittent dysphagia and food suddenly sticks in the middle of the chest which can be cleared with a drink of water indicates uncoordinated irregular esophageal peristalsis which is characteristic of esophageal spasm! Also “cork-screw esophagus” seen in barium swallow is diagnostic of esophageal spasm.
Q.106. A 46-year-old man is being investigated for indigestion. Jejunal biopsy shows deposition of macrophages containing PAS (Periodic acid-schiff) +ve granules. What is the most likely diagnosis?
Correct Answer : D
Whipple’s disease.
Periodic acid-Schiff +ve granules containing macrophages in jejunal biopsy is diagnostic of Whipple's disease. Whipple disease is a systemic disease most likely caused by a gram-positive bacterium, Tropheryma whippelii.
Although the first descriptions of the disorder described a malabsorption syndrome with small intestine involvement, the disease also affects the joints, central nervous system, and cardiovascular system.
Q.107. A patient presents with dysphagia and pain on swallowing. He has sore mouth and soreness in the corners of the mouth. What is the most likely diagnosis?
Correct Answer : D
Candida and CMV infection both can be the answer but Candida is more common than CMV.
Q.108. A child complains of RIF (right iliac fossa) pain and diarrhea. On colonoscopy, granular transmural ulcers are seen near the ileo-cecal junction. What should be the management?
Correct Answer : A
Pain in RIF, diarrhea, granular transmural ulcers near the ileocecal junction points towards the diagnosis of Crohn’s disease (predominantly ileocecal type).
We know for Crohn’s disease treatment options are -
i) Corticosteroids
ii) Immunosuppressants like azathioprine, mercaptopurine, and methotrexate, and
iii) Biological agents like adalimumab, infliximab, vedolizumab and ustekinumab.
However, if the patient is a child (steroid causes growth hamper) or can not tolerate corticosteroid alternate option used is 5-aminosalicylate as Salfasalazine. As the given patient is a child answer for him is A. Salfasalazine.
Q.109. A 30-year-old lady complains of intermittent diarrhea, chronic abdominal and pelvic pain and tenesmus. Sometimes she notices blood in her stool. Select the most likely cause leading to her symptoms?
Correct Answer : A
In diverticulosis there is usually constipation and diarrhea is less common. But in IBD there is usually diarrhea. Occasional blood in stool excludes irritable bowel disease. Adenomyosis can cause menstrual cramps, lower abdominal pressure, and bloating before menstrual periods and can result in heavy periods. UTI does not present like this.
The answer is IBD (Inflammatory bowel disease).
Q.110. A 40-year-old woman complains of dysphagia for both solids and liquids. She sometimes suffers from severe retrosternal chest pain. Barium swallow reveals a dilated esophagus which tapers to a fine distal end. What is the best management strategy?
Correct Answer : C
Dysphagia for both solids and liquids suggests neuromuscular dysphagia while dysphagia only for solids suggests mechanical obstruction. Here features are consistent with achalasia for which lower oesophageal sphincter dilation (balloon dilatation) is a treatment modality.
Q.111. A 38-year-old female G4 at 32wks of pregnancy presented with thick white marks on the inside of her mouth for 3 weeks. Her mouth including her tongue appeared inflamed on examination. She smokes 20 cigarettes/day despite advice to quit. She attends her ANC regularly. What is the most probable diagnosis?
Correct Answer : D
Lichen planus may have a lace-like appearance and not a thick white mark. The aphthous ulcer has a yellowish floor and is surrounded by an erythematous halo.
Smoking may cause tongue coating but not like thick white marks on the inside of the mouth. Leukoplakia with raised edges / Bright white patches and sharply defined and cannot be rubbed out like a candida patch; here also inflamed tongue points towards infection. So candidiasis is the most probable option.
Q.112. An 83-year-old woman who is a resident in a nursing home is admitted to hospital with a 4days history of diarrhea. She has had no weight loss or change in appetite. She has been on analgesics for 3 weeks for her back pain. She is in obvious discomfort. On rectal examination: fecal impaction. What is the most appropriate immediate management?
Correct Answer : D
In feacal impaction oral laxative is not the choice but phosphate enema is the best option here.
Q.113. A 72-year-old man presents with intermittent difficulty in swallowing with regurgitation of stale food materials. Sometimes he wakes up at night with a feeling of suffocation. Choose the most likely cause of dysphagia?
Correct Answer : D
In benign stricture, esophageal carcinoma, and systemic sclerosis there is persistent dysphagia not intermittent. In oesophageal spasm, there may be intermittent dysphagia but there will be no regurgitation of stale food material and no nocturnal regurgitation in recumbency. The clinical picture described is a well-known feature of the pharyngeal pouch.
Q.114. A 36-year-old patient came with diarrhea, bleeding, weight loss and fistula. What is the most likely diagnosis?
Correct Answer : B
Fistula is commonly seen in Crohn’s disease.
Q.115. A 25-year-old woman is presenting with diarrhea and abdominal bloating over the last 4 months. Examination: she has blistering rash over her elbows. Biochemistry: low serum albumin, calcium and folate concentration. On jejunal biopsy, there is shortening of the villi and lymphocytosis. What is the most likely diagnosis?
Correct Answer : A
Celiac disease.
Diarrhea, abdominal bloating, blistering skin rash over the elbow (Dermatitis herpetiformis), low serum albumin, calcium, and folate conc. Supported by shortening of villi and lymphocytosis on jejunal biopsy is a classic presentation of celiac disease.
Q.116. A 56-year-old woman has had severe abdominal pain for 24 hours radiating to her back and is accompanied by nausea and vomiting. She appears to be tachycardic and in shock. She was found to have gallstones, 2 years ago. What is the most likely investigation to confirm diagnosis?
Correct Answer : C
The likely diagnosis is pancreatitis. A normal lipase level can range from 0-160 U/L depending on the lab. When the pancreas is damaged, these digestive enzymes can be found in the blood at higher levels than normal. Amylase or lipase results more than three times normal levels are likely to mean pancreatitis.
Q.117. A young man has diarrhea, loss of weight and flatulence for 3 days. What is the most important treatment?
Correct Answer : A
Mainly colonic anaerobic bacterias produce most of the gas and treated with metronidazole.
Q.118. A 64-year-old male was admitted to the medical ward with complaint of diarrhea, abdominal pain and weight loss for few months. Examination: clubbing, perianal skin tags and abdominal tenderness. Colonscopy reveals transmural granulomatous inflammation involving ileocecal junction. He was diagnosed with what?
Correct Answer : A
Diagnosis is Crohn’s disease.
Crohn's disease is a type of inflammatory bowel disease (IBD) that may affect any segment of the gastrointestinal tract from the mouth to the anus. Symptoms often include abdominal pain, diarrhea (which may be bloody if inflammation is severe), fever, and weight loss.
Clubbing, perianal skin tags, and aphthous ulcers can also be seen. Transmural granulomatous inflammation on colonoscopy is diagnostic of Crohn’s disease.
Q.119. A 77-year-old woman suffered diarrhea 4 days ago. What would be her blood gas result?
Correct Answer : B
Diarrhoea causes metabolic acidosis and in response there occurs respiratory compensation [hyperventilation] leading to respiratory alkalosis and low PaCO2 (due to CO2 washout).
Q.120. A 60-year-old man presents with weight loss and Hb 6. History reveals that he has abdominal pain and diarrhea for the past 6months. What is the most appropriate investigation?
Correct Answer : B
The likely diagnosis is IBD. So Colonoscopy should be done.
Q.121. 66-year-old male presents with painful swallowing. What is the most likely diagnosis?
Correct Answer : C
Oropharyngeal and/or esophageal candidiasis
Q.122. An 80-year-old woman suffering from rheumatoid arthritis presents with severe epigastric pain and vomiting. She also complains of shoulder tip pain. What is the most discriminatory investigation?
Correct Answer : D
Elderly patients with RA are usually on NSAIDs which may lead to perforated peptic ulcer which presents as severe epigastric pain, vomiting, and shoulder tip pain. Diagnosis is made by seeing a free gas shadow under the diaphragm on erect CXR.
Q.123. A 2-year-old with atrophy of the buttocks, distended abdomen with frequent offensive smelly stool. Choose the most appropriate investigation?
Correct Answer : B
Endomyseal/alpha-gliadin antibody. [Atrophy of the buttock due to fat malabsorption and distended abdomen (sometimes with everted umbilicus) with frequent offensive smelly stools are seen in coeliac disease. Hence endomyseal/alpha gliadin antibody should be done.
Q.124. A 29-year-old young man presents with complaints of recurrent attacks of diarrhea. He says his stools contain blood and mucous. Sometimes he has low grade fever. What is the most appropriate investigation for his condition?
Correct Answer : D
Features are suggestive of IBD (inflammatory bowel disease), so barium enema is the most relevant investigation among the given options. Barium contrast dye allows an evaluation of the intestines. This is more commonly used in severe IBD to rule out serious complications like a perforated colon.
Q.125. A 26-year-old young man presents with history of passing loose stools for the past 2 months. He says his stools contain blood and mucus and are associated with abdominal pain. He undergoes a colonscopy after which he was started on treatment. What is the most appropriate treatment for his condition?
Correct Answer : A
Features and treatment after colonoscopy suggest diagnosis of ulcerative colitis for which the initial treatment option is mesalazine.
Q.126. A 28-year-old female presented with complains of difficulties in swallowing liquids only. She also suffers from recurrent chest infection in the past few months. What is the most probable diagnosis?
Correct Answer : C
Dysphagia to both solid and liquid or mostly to liquid is a common feature of achalasia. In the early stages of achalasia there may occur aspiration due to regurgitation during lying down to sleep which may result in recurrent chest infection and cough.
Q.127. A previously healthy 23-year-old presented with a week’s history of bloody diarrhea and abdominal pain with cramps and fever. Examination: tenderness in lower abdomen. What is the most appropriate diagnosis?
Correct Answer : D
A short history (one week) of bloody diarrhea, abdominal pain with cramps, fever, and tenderness in the lower abdomen is indicative of gastroenteritis.
Q.128. A 45-year-old male with epigastric discomfort has been given triple therapy. He has now returned after 4 weeks of epigastric discomfort. What investigation would you do for him?

Correct Answer : B
H. pylori breath test
Q.129. A 56-year-old male presents with persistent watery diarrhea. What is the most likely diagnosis?
Correct Answer : C
Cryptosporidiosis mainly affects children. It can affect adults as well. It causes a self-limited diarrheal illness in otherwise healthy adults. However, it is also recognized as a cause of prolonged and persistent diarrhea which can result in malnutrition. Cryptosporidiosis can manifest as chronic severe diarrhea in persons with acquired immunodeficiency syndrome (AIDS).
Q.130. A 26-year-old man is referred for gastroscopy because of a history of several months of dyspepsia. He has routine bloods checked and is found to have a serum calcium level=3.2mmol/l with a venous bicarbonate level of 33mmol/l. Renal and LFT are both normal. CXR is normal. What is the most likely cause of his hypercalcemia?
Correct Answer : C
In medicine, the milk-alkali syndrome is characterized by high blood calcium caused by taking in too much calcium and absorbable alkali; common sources of calcium and alkali are dietary supplements taken to prevent osteoporosis and antacids. If untreated, milk-alkali syndrome may lead to kidney failure or death.
Q.131. A patient admitted due to repeated attacks of pancreatitis presents with dementia and loss of proprioception in the legs. What is the most appropriate treatment?
Correct Answer : C
Pancreatic insufficiency can lead to malabsorption and B12 (cobalamin) deficiency. Dementia and diminished vibratory sensation and proprioception in the lower extremities were the most common objective findings of cobalamin deficiency.
The damage to the myelin due to cobalamin deficiency results in a condition known as subacute combined degeneration of the spinal cord (SCDSC). This condition affects various parts of the spinal cord, including the dorsal columns, the lateral corticospinal tracts, and the spinocerebellar tracts, resulting in a loss of proprioception, ataxia, the development of peripheral neuropathy, and dementia.
Q.132. A 38-year-old man presented to the emergency department with severe pain in upper abdomen. He has already taken course of triple therapy and now had elective endoscopy 2 days ago. He is in shock. What is the most probable diagnosis?
Correct Answer : C
Mediastinitis usually results from an infection. It may occur suddenly (acute), or it may develop slowly and get worse over time (chronic). It most often occurs in a person who recently had an upper endoscopy or chest surgery. A person may have a tear in their esophagus that causes mediastinitis.
Q.133. A 36-year-old patient came with diarrhea, bleeding, weight loss and fistula. What is the most likely diagnosis?
Correct Answer : C
The key is C. CD. [Bloody diarrhea can occur in both CD & UC. Also, weight loss is common! but fistula formation is a well-recognized complication of CD].
Q.134. A 26-year-old man presented with abdomen distension and pain. His stools have been mucoid and sometimes blood stained. What is the most appropriate investigation?
Correct Answer : D
Probable diagnosis is Crhon's disease.
Q.135. A 28-year-old man with recent onset of dyspepsia after eating spicy food and alcohol consumption. H. pylori fecal antigen was negative. He returns after 1month with similar symptoms despite being given omeprazole 40mg. What is the best initial investigation?
Correct Answer : B
Gastrosopy
Q.136. A 48-year-old woman is admitted to the emergency department with a productive cough and moderate fever. She often has central chest pain and she regurgitates undigested food most of the time but doesn’t suffer from acid reflux. These symptoms have been present for the last 3.5 months which affects her daily food intake. CXR: air-fluid level behind a normal sized heart. What is the most likely diagnosis?
Correct Answer : D
Usually in hiatus hernia there is acid reflux.
Q.137. A 34-year-old man has an intermittent epigastric pain for 3 weeks. It is worse by food but helped by some tablets he obtained from the pharmacy. He had a similar episode 3 years ago and his doctor gave him a course of 3 types of tablets at the time. What is the most appropriate next investigation?
Correct Answer : D
Patient was all right for 3 years after eradication therapy. Now symptoms again may indicate a recurrence of H. Pylori infection which can be demonstrated by a C13 urea breath test. Serum antibodies persist (IgG) for long and are not reliable for recheck.
Q.138. A 48-year-old man has intermittent left sided lower abdominal pain and feels generally unwell. He has lost his appetite and has lost weight. Temperature 38.3C and he has BP 190/100mmHg. What is the investigation most likely to lead to diagnosis?
Correct Answer : A
Probable diagnosis is diverticulitis and the preferred investigation from the given list is colonoscopy. Colonoscopy: It views the colon's interior to see the inflamed, infected pouches. Ultrasound images lack the detail of CT images and cannot evaluate the intestines as well as CT.
Q.139. A 40-year-old woman on chemotherapy for metastatic breast carcinoma now presents with painful swallowing. Examination: she has white plaques on top of friable mucosa in her mouth and more seen on esophagoscopy. What is the most effective treatment for this patient?
Correct Answer : D
Features are consistent with oesophageal candidiasis which is treated with Oral fluconazole (200-400 mg daily) or IV fluconazole for 14-21 days (here iv fluconazole as the patient is immunocompromized due to chemotherapy).
Q.140. A 50-year-old man complains of dysphagia after eating bread. Barium swallow reveals a lower esophageal ring. What is the most appropriate treatment?
Correct Answer : C
Patients with recurrent symptoms from esophageal rings and webs require repeat esophageal dilation. Repeat esophageal dilation is safe and can relieve symptoms in the long term.
Q.141. A patient presents with increasing retrosternal pain and dysphagia for both solids and liquids over 18 months but denies weight loss. Chest is clear. What is the most likely diagnosis?
Correct Answer : C
Esophageal spasm.
Q.142. A 46-year-old woman presents with sudden episode of abdominal pain which started about 2 hours ago. The pain is located in the epigastrium and radiates to her back. She has vomited twice since the onset of attack. The pain is made worse by lying flat on her back and she is more comfortable sitting up and bending forwards. She was informed of the presence of gallstones in her gall bladder four weeks earlier when she reported pain in the right hypochondrium. The oral temperature is 39C, BP 120/80mmHg and the radial pulse 118/min. There is no jaundice but there is marked tenderness in the epigastrium both on deep and superficial palpations. Which is the most appropriate investigation for the cause of the patient’s pain?
Correct Answer : B
Epigastric pain radiating to back, worse on lying flat and comfort on bending forward are classic presentation of acute pancreatitis in which serum amylase is increased.
Q.143. An elderly male patient with prior history of hematemesis is having history of long term use of aspirin and other drugs, now presents with severe epigastric pain, dysphagia and vomiting. He was connected to vital monitors which were not reassuring. What is the management?
Correct Answer : D
Long-term use of a nsaid predisposes to peptic ulcers. This may cause considerable bleeding leading to shock.
Q.144. A 14-year-old boy has had recurrent abdominal pains, malaise and weight loss over 6 months. He has had a vague mass in the right iliac fossa. Colonoscopy and biopsy of the caecal area shows transmural inflammation and granulomata. What is the most appropriate management?
Correct Answer : A
Recurrent abdominal pains, weight loss, and transmural inflammation and granulomata points towards the diagnosis of Crohn’s disease which is treated with sulphasalazine.
Q.145. An 8-year-old has had recurrent abdominal pain for 2 months. His appetite is reduced and he has faecal soiling. There are pitting masses throughout the abdomen. He has a dilated rectum. What is the most appropriate management?
Correct Answer : C
Pitting masses throughout the abdomen with dilated rectum indicates retained faecal matter. Enema and laxatives are the treatment.
Q.146. A 12-year-old has recurrent abdominal pain which is worse when he is hungry. The pain is relieved by food or meal. He is tender in the epigastrium. Test has revealed Helicobacter pylori infection. What is the most appropriate management?
Correct Answer : A
As the patient has H. pylori infection the most appropriate management is triple therapy. But as it is not in the given options Proton pump inhibitor is the next answer.
Q.147. A 29-year-old lady who is a bank manager is referred by the GP to the medical OPD due to a long history of tiredness and pain in the joints. An autoimmune screen result showed smooth muscle antibodies positive. What is the most appropriate next investigation?
Correct Answer : C
A case of autoimmune hepatitis. Autoimmune hepatitis is an uncommon cause of chronic hepatitis which if untreated can lead to cirrhosis. However, the treatment outlook is very good. Smooth muscle antibody is positive in autoimmune hepatitis. The definitive investigation is a liver biopsy. Treated with steroid [start with high dose prednisolone]. Azathioprine is commonly added with steroids to reduce its dose as steroid has more side effects than azathioprine.
Q.148. A young male whose sclera was noted to be yellow by his colleagues has a history of taking OTC (over the counter) drugs for some pain. Tests showed raised bilirubin, ALT and AST normal. The provocation test with IV nicotinic acid is positive and produces further rise in the serum bilirubin levels. What is the most likely diagnosis?
Correct Answer : C
Only bilirubin is increased but not the liver enzymes. Also, positive nicotinic acid provocation test is in favour of Gilbert’s syndrome.
Q.149. A man post-cholecystectomy presented with jaundice, fever and dark urine. What is the most diagnostic investigation?
Correct Answer : A
Post operative US will not give good results. We shall not go for ERCP first as it has complications like injury and pancreatitis. Acceptable options are CT, MRI and MRCP among which most appropriate is MRCP! But as the Question is most diagnostic it is ERCP. The diagnosis here is choledocolithiasis with cholangitis.
Q.150. A 45-year-old woman has had severe epigastric and right hypochondrial pain for a few hours. She has a normal CBC, serum ALP is raised, normal transaminase. 3 months ago she had a cholecystectomy done. What is the most appropriate investigation?
Correct Answer : C
Post-operative US of the abdomen does not give good results for the hepatobiliary system. ERCP is an invasive procedure and it has considerable complications like cholangitis, injury, pancreatitis, etc. Among the given options MRCP is most appropriate. We shall go for ERCP after confirming the diagnosis confirmed. For this MRCP is preferred.
Q.151. A lady comes in severe liver disease and hematemesis. Her INR is >10. What should she be given?
Correct Answer : A
FFP
Q.152. An alcoholic 56-year-old man had ascitic fluid analysis done which was found to be yellow color. What is the most appropriate cause?
Correct Answer : B
If the patient experiences serious problems described below his disease has progressed from compensated cirrhosis to decompensated cirrhosis:
1. Bleeding varices (internal bleeding)
2. Ascites (fluid in the belly)
3. Encephalopathy (confusion)
4. Jaundice (yellowing of eyes and skin)
Q.153. A child presents with increasing jaundice and pale stools. Whats the most appropriate test?
Correct Answer : A
This is a picture suggestive of obstructive jaundice. LFT can give clues like much-raised bilirubin, AST, and ALT not that high and raised alkaline phosphatase but still USG is diagnostic in case of obstructive jaundice.
Q.154. A 28-year-old female presents with 1 week history of jaundice and 2 days history of altered sleep pattern and moods. She was diagnosed with hypothyroidism for which she is receiving thyroxine. TFT showed increased TSH. PT (prothrombin time) 70s. What is the most probable diagnosis?
Correct Answer : C
Autoimmune hepatitis may present as acute hepatitis, chronic hepatitis, or well-established cirrhosis. Autoimmune hepatitis rarely presents as a fulminant hepatic failure. One-third may present as acute hepatitis marked by fever, hepatic tenderness, and jaundice.
Non-specific features are anorexia, weight loss, and behavioural change (here altered sleep pattern and moods).
There may be coagulopathy (here PT 70s) leading to epistaxis, gum bleeding, etc. The presence of another autoimmune disease like hypothyroidism supports the diagnosis of autoimmune hepatitis.
Q.155. A 42-year-old female who is obese comes with severe upper abdominal pain with a temperature 37.8C. She has 5 children. What is the most probable diagnosis?
Correct Answer : D
Fat, female, fair, forty, and fertile are the pnemonic for cholecystitis! Here the presentation of severe upper abdominal pain with fever along with the pnemonic features points towards the diagnosis of cholecystitis.
Q.156. A child with increasing jaundice and pale stools. Choose the appropriate test:
Correct Answer : D
This is obstructive jaundice where the US may show dilatation of common bile duct or stones.
Q.157. A patient presented with jaundice, fever and upper abdominal pain within 24 hour after removal of gallstone by ERCP. The cholangiography was done and it was patent. What is the possible cause of his complaints?
Correct Answer : B
Though biliary infection is possible but acute pancreatitis is a more common complication of ERCP and the absence of any obstruction (stone or tumour which helps biliary infection to occur) makes cholangitis less likely.
Q.158. A 64-year-old alcoholic who has been diagnosed with liver cirrhosis presents with a massive ascites. What is the mechanism of fluid accumulation in a patient with liver disease?
Correct Answer : B
Ascites in patients with cirrhosis is the result of portal hypertension and renal salt and water retention. Similar mechanisms contribute to ascites formation in heart failure. Portal hypertension signifies elevation of the pressure within the portal vein. According to Ohm’s law, pressure is the product of resistance and flow. Increased hepatic resistance occurs by several mechanisms. First, the development of hepatic fibrosis, which defines cirrhosis, disrupts the normal architecture of the hepatic sinusoids and impedes normal blood flow through the liver. Second, activation of hepatic stellate cells, which mediate fibrogenesis, leads to smooth-muscle contraction and fibrosis. Finally, cirrhosis is associated with a decrease in endothelial nitric oxide synthetase (eNOS) production, which results in decreased nitric oxide production and increased intrahepatic vasoconstriction. The development of cirrhosis is also associated with increased systemic circulating levels of nitric oxide (in contrast to the decrease seen intrahepatically), as well as increased levels of vascular endothelial growth factor and tumor necrosis factor, that result in splanchnic arterial vasodilation. Vasodilation of the splanchnic circulation results in pooling of blood and a decrease in the effective circulating volume, which is perceived by the kidneys as hypovolemia. Compensatory vasoconstriction via release of antidiuretic hormone ensues; the consequences are free water retention and activation of the sympathetic nervous system and the renin-angiotensin-aldosterone system, which lead in turn to renal sodium and water retention.
Cause of edema in cirrhosis:
The condition of Hepatic Cirrhosis is characterized, in part, by hepatic venous outflow obstruction, which in turn expands the splanchnic blood volume, and hepatic lymph formation. Intrahepatic hypertension acts as a stimulus for renal sodium retention and causes a reduction of effective arterial blood volume. These alterations are frequently complicated by hypoalbuminemia secondary to reduced hepatic synthesis, as well as peripheral arterial vasodilation. These effects reduce the effective arterial blood volume, leading to activation of the sodium- and water-retaining mechanisms. The concentration of circulating aldosterone often is elevated by the failure of the liver to metabolize this hormone. Initially, the excess interstitial fluid is localized preferentially proximal (upstream) to the congested portal venous system, causing ascites. In later stages, particularly when there is severe hypoalbuminemia, peripheral edema may develop. A sizable accumulation of ascitic fluid may increase intraabdominal pressure and impede venous return from the lower extremities and contribute to the accumulation of the edema.
Q.159. A 68-year-old man who is a known case of liver cirrhosis has developed ascites. What is the mechanism for the development of ascites?
Correct Answer : A
In liver cirrhosis ascites (not generalized oedema which is caused by hypoalbuminemia and other mechanisms though they may have roles) is caused by portal hypertension (portal hypertension is invariable in cirrhosis) along with other factors.
Q.160. A 45-year-old male alcoholic presents after a large hematemesis. He has some spider naevi on his chest, BP 100/76mmHg, pulse 110bpm. He has a swollen abdomen with shifting dullness. What's the diagnosis?
Correct Answer : D
Spider nevi and ascites suggest advanced liver disease. Here an alcoholic middle-aged man having large hematemesis with the above-mentioned features are very suggestive of bleeding from esophageal varices secondary to portal hypertension in liver cirrhosis.
Q.161. A 45-year-old woman presents with pruritis. Examination: skin pigmentation. Investigation: raised ALP and presence of anti-mitochondrial antibodies. What is the most likely diagnosis?
Correct Answer : D
Primary biliary cirrhosis, is an autoimmune disease of the liver. It results from a slow, progressive destruction of the small bile ducts of the liver, causing bile and other toxins to build up in the liver, a condition called cholestasis.
Further slow damage to the liver tissue leads to scarring, fibrosis, and eventually cirrhosis.
Pruritus, skin pigmentation (increased amounts of melanin, widely dispersed throughout both epidermis and dermis), raised ALP, and the presence of AMA is diagnostic of primary biliary cirrhosis.
Q.162. A 42-year-old female who is obese comes with severe upper abdominal pain and right shoulder tip pain with a temperature of 37.8C. She has 5 children. What investigation should we do for diagnosis?
Correct Answer : D
The diagnosis is cholecystitis. The diagnosis of cholecystitis is suggested by the history (abdominal pain, nausea, vomiting, fever) and physical examinations in addition to laboratory and ultrasonographic testing.
Boas's sign which is pain in the area below the right scapula, can be a symptom of acute cholecystitis. The pnemonic for cholecystitis is 5 “f”. Fat, female, fair, forty, fertile = cholecystitis.
Q.163. An 18-year-old male works in a company where lunches are often catered. One day, the water at the company facility is not working, but they manage to have the lunch anyway. 2wks later, he becomes sick. He develops anorexia, nausea, malaise and jaundice. During the course of the next 4wks, 7 people who shared in the lunch become ill with similar symptoms. After a few wks, each of the 7 people completely recovers and they replace their caterer. What is a likely diagnosis?
Correct Answer : D
Symptoms of Hepatitis : A range from mild nausea to liver failure (very rare). Spread is normally by the faecal-oral route although there are occasional outbreaks through food sources.
Hand washing and good hygiene around food and drink prevent the spread of infection. Increasing age is a direct determinant of disease severity.
Choose a Question
×Choose a Question
×
Trial Access Limit Reached
You’ve reached the limit of free content. Subscribe to continue learning without restrictions.