

Hello,
Dr. Batman
Hello Doctor, Welcome!
Profile

Name: Batman
Email: batman@gotham.com
GENERAL SURGERY
(Total Questions - 214)Q.1. A 65 year old man has right upper quadrant discomfort. He has lost 12 kg in the last 5 months. On examination, a palpable liver with nodularities was found. Three years ago,he had a right hemicolectomy for a colorectal cancer. What is the most appropriate tumour marker to investigate?
Correct Answer : D
Carcinoembryonic antigen (CEA) is especially important to monitor response to treatment and identify relapse in tumours showing raised CEA at diagnosis (e.g.colorectal cancers).
The history of the right upper quadrant discomfort and the examinations of a palpable liver are descriptions of tumour metastasis to the liver. CEA raises with a metastatic tumours from colon whereas alpha-fetoprotein (AFP) is elevated in primary hepatocellular carcinoma.
So do not get confused and pick AFP where there is a clear history of colorectal carcinoma.
Carcinoembryonic antigen (CEA) is vital for monitoring treatment response and detecting tumor relapses, especially colorectal cancers, that initially present with elevated CEA levels.
Signs of right upper quadrant discomfort and a palpable liver indicate potential metastasis of the tumor to the liver. CEA levels rise in colorectal cancer metastases, whereas alpha-fetoprotein (AFP) is specific to primary hepatocellular carcinoma.
It’s important not to confuse the two; prioritize CEA when there’s a history of colorectal carcinoma.
Q.2. A 30 year old woman presents to her family physician with the complaint of a lump in her left breast. She first noticed the mass two weeks ago in the shower and the patient says that she has not noticed whether the mass appears and disappears with the occurrence of her menses. The patient’s past medical history was insignificant and she claims that she is on no long term medication. Further questioning reveals that the patient has no further complaints of night sweats, weight loss or a fever and this is the first breast mass that she has noticed. She has no family history of breast cancer. On physical examination, it was revealed that a 2.5 cm x 1.5 cm mass is present in the left lower quadrant of her left breast. The mass was regular and firm in consistency and was non-tender and mobile. The skin over her left nipple appeared to be normal and no discharge from her left nipple could be appreciated. The rest of the breast examination was unremarkable with no enlarged lymph nodes palpated in her neck or axillary region. Examination of her right breast was unremarkable. Fine needle aspiration cytology (FNAC) was subsequently done. The results show duct-like epithelium surrounded by fibrous bridging. What is the most likely diagnosis?
Correct Answer : A
The woman in this scenario has the classical picture of a fibroadenoma.
Fibroadenomas are the most common type of breast lesion in young women. Although this women is not very young, based on her past medical history, family history and examination results, a fibroadenoma is the single most likely diagnosis for her.
Fibroadenomas arise in breast lobules and are composed of fibrous and epithelial tissue. They present as firm, nontender and highly mobile masses.
Fibroadenosis is less likely because the hallmark of these lumps is that the lump appears just before menstrual periods and disappears afterwards.
Also, the biopsy of fibroadenosis reveals fibrosis, adenosis, epitheliosis and cyst formation.
The usual presentation of fibroadenosis is a breast lump or pain in the breast.
Breast carcinoma is the most common cause of a breast mass in postmenopausal patients. In malignancy, there is an abundant pure population of tumour cells, singly and in clusters.
Q.3. A 36 year old man is about to undergo an elective inguinal hernia surgery. His blood tests show: Haemoglobin 82 g/L, Mean cell volume 70 fL, White cell count 5 x 109 /L, Platelets 180 x 109 /L. What is the most appropriate next action?
Correct Answer : A
For elective procedures, proceed only if the haemoglobin is above 100 g/L (10 g/dL).
If haemoglobin is lower than that, defer the operation and investigate first. If haemoglobin was below 80 g/L (8 g/dL) and the patient was symptomatic, then transfuse with blood.
Q.4. A 62 year old man presents to the emergency department with acute onset of severe, persistent abdominal pain. The pain started two hours ago. On examination, his abdomen is distended and has generalised tenderness. There is no bowel sounds on auscultation. He has a heart rate of 110 beats/minute and a blood pressure of 100/60 mmHg. A venous blood gas was performed which shows a lactate of 6.4. And ECG taken shows evidence of atrial fibrillation. Analgesia, intravenous fluids and broad spectrum antibiotics were started. What is the diagnosis?
Correct Answer : D
In acute mesenteric ischaemia, VBG typically shows a high lactate. If an ABG had been performed, it would have revealed severe metabolic acidosis with a high lactate.
Atrial fibrillation is the likely cause of the embolism that has caused the ischaemic even in the gut. We should have a high suspicion of embolization to the superior mesenteric artery with any patient with atrial fibrillation who complains of severe abdominal pain.
Please remember that ischaemic colitis is different from acute mesenteric ischaemia.
Mesenteric ischaemia is acute with an abrupt cessation of blood supply to the gut whilst ischaemic colitis has a chronic presentation over hours which occurs due to a transient disruption of blood supply to the colon.
In the Emergency Department, if mesenteric ischaemia is suspected, resuscitation with oxygen and intravenous fluids should be commenced. Also administer intravenous analgesia and broad spectrum intravenous antibiotics. These patients need to be referred to the surgeons urgently.
Mesenteric ischaemia is the abrupt cessation of blood supply to a large portion of the bowels resulting to irreversible gangrene. Usually occurs in the middle-aged or elderly patients.
Causes:
• Mesenteric arterial embolism (seen in patients with atrial fibrillation)
• Decreased mesenteric arterial blood supply (seen in patients with hypertension secondary to myocardial ischaemia)
Clinical features :
• Severe sudden onset of abdominal pain
• Severity of pain exceeds the physical signs
• Absent bowel sounds
• Abdominal distension and tenderness
Q.5. A 55 year old man presents with a lump in the left supraclavicular region. He complains of reduced appetite and he has lost 7 kg in the last two months. What is the most probable diagnosis?
Correct Answer : B
The lump at the left supraclavicular region known as Troisier’s sign (an enlarged left supraclavicular node – Virchow’s node), it is indicative of gastric cancer.
Q.6. A 44 year old woman had a total abdominal hysterectomy and bilateral salpingooophorectomy 5 days ago. She now has increasing abdominal discomfort and is now bloating. She was encouraged to stay well hydrated but she is still unable to pass gas. No bowel sounds are heard. What is the most appropriate next step?
Correct Answer : A
The likely diagnosis here is paralytic ileus and an x-ray can help with diagnosis.
Prolonged surgery is one of the major causes of paralytic ileus and it occurs due to overhandling of the bowel.
Paralytic ileus is to be expected in the first few days after abdominal surgery. Bowel sounds are absent and there is no passage of gas. There may be mild distension, but there is usually minimal pain.
PARALYTIC ILEUS -
Clinical features :
• Abdominal distension, tympanic or dull on percussion.
• Abdominal X-ray - Shows air/fluid-filled loops of small and/or large bowel
• Intestinal ileus usually settles with appropriate treatment.
Treatment : Pass an NGT to empty the stomach of fluid and gas if the patient is nauseated or vomiting.
Small volumes of tolerated oral intake may help mild ileus to resolve.
• Ensure adequate hydration by IV infusion (‘drip and suck’).
• Reduce opiate analgesia and encourage the patient to mobilize.
Q.7. A 60 year old woman has lower abdominal discomfort and mild abdominal distension. On pelvic examination, a nontender, solid irregular right adnexal mass is felt. Her Pap smear done a year ago was normal. What is the most appropriate tumour marker to request for?
Correct Answer : A
A pelvic mass that is identified after menopause should raise the suspicion of ovarian cancer.
Remember that in post menopausal women, the ovaries should normally be atrophic so if they are felt, think of ovarian carcinoma.
Q.8. A 39 year old woman has been having tingling and numbness of her thumb, index and middle fingers for a while. She has been treated with local steroids but there was no improvement. She has planned to undergo a surgical procedure. What is the most likely structure to be incised?
Correct Answer : B
During open carpal tunnel release surgery, the transverse carpal ligament is cut, which releases pressure on the median nerve and relieves the symptoms of carpal tunnel syndrome.
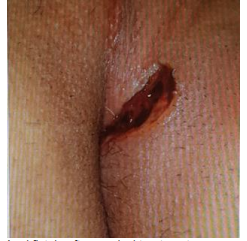
Q.9. A 41 year old man has a painful palpable mass near his anus for the past one week. The pain is described as throbbing and worse when sitting down. On examination, the lump is warm, erythematous, and tender. He has a history of diabetes mellitus type 2. What is the most likely diagnosis?
Correct Answer : B
This is a very straightforward question. Although many of the options could be very well correct, the history of diabetes should point you towards an infective cause.
Hence, the perianal abscess is the answer.
It is one of the common causes of anorectal pain.
Perianal abscesses have a gradual onset, usually with constant localized perianal pain.
Throbbing and severe are good ways to describe a perianal abscess especially if the patient describes the pain as worse when sitting down.
Tenderness and swelling is common and occasionally with discharge. Other symptoms also include constipation or pain associated with bowel movements.
Q.10. A 32 year old man has undergone an open appendectomy earlier today. In theatre, a gangrenous appendix was found. What is the most appropriate pain relief to administer postoperatively?
Correct Answer : A
This is a case of an open surgery. Patient controlled analgesia with morphine would be the best to start off and this could be weaned off when the patient is in less pain.
Q.11. A 54 year old man presents to the Emergency Department with abdominal pain which started 18 hours ago. The pain had gradual onset which initially started at the left abdomen associated with nausea. His medical history includes heart failure, diabetes and hypertension. On examination, his abdomen has generalised tenderness. A digital rectal examination shows blood per rectum. He has a heart rate of 80 beats/minute, blood pressure of 150/80 mmHg and a temperature of 37.9 C. What is the most likely diagnosis?
Correct Answer : C
Ischaemic colitis is caused by transient disruption of blood supply to the colon which leads to mucosal ulceration, inflammation and haemorrhage hence the PR bleeding is mentioned in this stem.
A low grade pyrexia, tachycardia and abdominal tenderness would also fit with symptoms of an ischaemic colitis.
The aetiology is often multifactorial involving either thrombotic events or hypoperfusion (such as shock, heart failure or a myocardial infarction).
In this stem, heart failure was the cause.
Please remember that ischaemic colitis is different from acute mesenteric ischaemia.
Mesenteric ischaemia is acute with an abrupt cessation of blood supply to the gut whilst ischaemic colitis has a chronic presentation over hours which occurs due to a transient disruption of blood supply to the colon.
Q.12. A 48 year old man complains of rectal bleeding and loss of weight. He has a mass in left iliac fossa. What is the most likely diagnosis?
Correct Answer : B
The position of the mass in combination of the symptoms of change of bowel habit and weight loss can only be from a carcinoma of sigmoid colon.
Q.13. A 27 year old woman presents to Accident & Emergency with the complaint of right upper quadrant pain. She has no other complaints and is experiencing no other symptoms. Her past medical history is significant for gallstone disease as confirmed on ultrasound. Her last episode of biliary colic was three years ago, for which she received analgesia. Each episode of pain that she has presented with in the past has been managed successfully with morphine and has resolved completely after treatment with analgesia. Her medical notes show that the last ultrasound that she had shows an increased common bile duct diameter. What is the best investigation to perform now for this patient?
Correct Answer : C
The fact that this patient already has confirmed gallstones seen on ultrasound with an increased common bile duct diameter means that it is highly likely that she is having a repeat episode of biliary colic or perhaps even cholangitis. The next best investigation would be to confirm the diagnosis on a repeat ultrasound.
ERCP is used primarily to diagnose and treat conditions of the bile ducts and main pancreatic duct.
Newer modalities such as MRCP produce detailed images of the hepatobiliary and pancreatic systems. This means that ERCP is now rarely performed without therapeutic intent.
BILIARY COLIC :
Occurs when a stone temporarily occludes the cystic duct. There is a colicky pain in the right upper quadrant radiating to the right shoulder. The pain can also radiate to the back in the interscapular region.
Nausea and vomiting are common which often accompanies the pain. The episode is usually self-limiting.
Ultrasound establishes the diagnosis of gallstones.
Contrary to its name “Biliary colic”, the pain usually does not fluctuate but instead is consistent and can last anywhere between 15 minutes up to 24 hours where the pain gradually subsides spontaneously or with the help of analgesia.
The main difference between inflammatory component biliary colic and acute cholecystitis is the inflammatory component.
In acute cholecystitis, there is local peritonism, fever, and elevated WCC.
Management includes:
• Analgesia (usually opioids such as morphine)
• Rehydrate
• Nil by mouth.
• Elective laparoscopic cholecystectomy is usually indicated.
Q.14. A 27 year old woman visits the GP for a routine annual examination. She has had a lump in her breast for two years but has not sought any medical advice. The mass has remained the same size for the past two years. On examination, the mass is located on the right upper quadrant and it is felt as a firm 3 cm by 2 cm mass. It is nontender and mobile. What is the most likely diagnosis?
Correct Answer : D
Fibroadenomas are the most common breast tumors found in adolescence and young women. Clinically, fibroadenomas are firm, non-tender, highly mobile palpable lumps.
It is important to remember that the most distinctive feature of fibroadenomas that distinguishes them from other breast lumps is the fact that they are highly mobile. In fact, some small lumps may slip away from the examining hand during palpation because they are extremely mobile, giving rise to their description “breast mice”.
Most fibroadenomas are found in the upper outer quadrant of the breast.
They are thought to result from an increased sensitivity to oestrogen.
Diagnosis is usually made with a combination of clinical assessment, ultrasonography and fine needle aspiration cytology.
Q.15. A 58 year old lady with a medical history of type 1 diabetes mellitus has a tender lump near the anal opening which has been increasing in size for the last 3 weeks. She complains of constipation and throbbing pain when she sits down. She has a temperature of 38.1 C. The mass is seen to be swollen, erythematous and tender at the edge of the anus. What is the most appropriate management?
Correct Answer : A
This is a case of anorectal abscess.
Diabetes, immunocompromised patients or patients with Crohn’s disease are likely candidates for an anorectal abscess.
Fever and pain are typical for an anorectal abscess.
The perianal pain is sometimes worse when sitting and can be associated with constipation.
Management would include surgical drainage.
Antibiotic use is necessary if there is a history of diabetes or immunosuppression.
Q.16. A 29 year old woman presents with a single 2 cm x 2 cm lump in the breast. The lump is mobile and hard in consistency. On examination, the mass is painless and there is also palpable lymph node in the axilla. An ultrasound was performed which shows a mass with hypoechoic, ill-defined, spiculated and microlobulated margins. A mammogram shows ill-defined, spiculate borders. A fine needle aspiration cytology was performed which results came back as normal. What is the most appropriate investigations to confirm the diagnosis?
Correct Answer : D
Breast fine needle aspirations are not 100% accurate. The lump is suspicious.
The most appropriate investigation to confirm the diagnosis is a core biopsy. A core biopsy uses a hollow needle to take one or more samples of breast tissue from the area of concern. Because tissue is taken rather than cells, it gives more detailed information compared to a fine needle aspiration.
A fine needle aspiration (FNA) involves taking one or more samples of breast cells using a fine needle and syringe.
The sample of fluid or cells is smeared on a glass slide and sent to a pathology laboratory to be examined. It is usually done under ultrasound guidance or occasionally mammogram guidance.
Fine needle aspirations only take a small amount of cells and thus they cannot be used to definitely rule out cancer as sometimes the cells that are taken may have arisen from normal tissue.
A punch biopsy may be done when there is a change to the skin of the breast or nipple.
It involves taking a very small cylindrical piece of tissue from the changed area.
Q.17. A 31 year old woman has undergone a removal of a 4 cm breast lump on the upper outer quadrant of her left breast. The histology report states: “A well circumscribed lump with clear margins and separate from the surrounding fatty tissue. There are overgrowths of fibrous and glandular tissue.” What is the most likely interpretation of this report?
Correct Answer : D
The histology findings are consistent with a Fibroadenoma.
Q.18. A 35 year old construction worker is diagnosed with indirect inguinal hernia. Which statement below best describes indirect inguinal hernias?
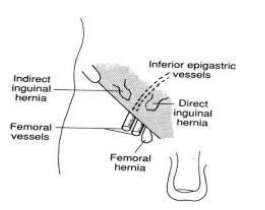
Correct Answer : D
Indirect inguinal hernias occur when abdominal contents protrude through the deepinguinal ring, lateral to the inferior epigastric vessels; this may be caused by failure of embryonic closure of the processus vaginalis.
An indirect inguinal hernia like other inguinal hernias protrudes through the superficial inguinal ring. It is the most common cause of groin hernia.
In an indirect inguinal hernia, the protrusion passes through the deep inguinal ring and is located lateral to the inferior epigastric artery.
Q.19. A 34 year old diabetic man has a positive family history for colon cancer. He is a smoker and smokes 8 cigarettes a day. He also consumes in excess of 30 units of alcohol per week. Due to the pressures of his job, he is only able to exercise once a month. Which of the following carries the greatest risk for colon cancer?
Correct Answer : B
Colorectal cancer is a multifactorial disease.
Non-modifiable risk factors such as genetic factors, environmental exposures, and inflammatory conditions of the digestive tract.
Modifiable risk factors such as diet, smoking, sedentary habits, and increased alcohol intake.
There is also an increased risk of colorectal cancer with a diet high in red meat and animal fat, low-fiber, low overall intake of fruits and vegetables.
However, amongst the options, genetic factors have correlation to colorectal cancer with around 20% of bowel cancers associated cancer-causing with hereditary factors. Cancer causing genes such as in familial adenomatous polyposis, carry an increased risk of the development of colorectal carcinoma in which affected individuals carry an almost 100% risk of developing colon cancer by the age of 40 years.The single greatest risk factor for colorectal cancers is age but that is not an option in this question.
RISK FACTORS OF COLORECTAL CANCER:
• Age – Older age is the main risk factor for colorectal cancers
• Family history of colorectal neoplasia: carcinoma, adenoma under the age of 60 years
• Past history of colorectal neoplasm: carcinoma, adenoma
• Inflammatory bowel disease: ulcerative colitis, crohn's disease
• Polyposis syndromes: familial adenomatous polyposis (Gardner's syndrome),
Turcot's syndrome, attenuated adenomatous polyposis coli, flat adenoma syndrome, hamartomatous polyposis syndromes (Peutz-Jeghers syndrome, juvenile polyposis syndrome, Cowden's syndrome)
• Hereditary non-polyposis colorectal cancer (HNPCC)
• Diet - Rich in meat and fat, Poor in fibre, folate and calcium
• Sedentary lifestyle
• Obesity
• Smoking
• High alcohol intake
• History of small bowel cancer, endometrial cancer, breast cancer or ovarian cancer
Q.20. A 49 year old lady had a colostomy closure 4 days ago. She now comes with fluctuating small swelling in the stoma. Her temperature is 37.9 C, respiratory rate is 18/min, pulse rate is 80 bpm. What is the most appropriate management?
Correct Answer : A
Fluctuating small swelling indicates an abscess has formed. Local exploration would be beneficial in this scenario. Stomal abscess is a collection of pus (infection) occurring just under the skin around the site of the stoma.
Antibiotics and drainage of the pus is sometimes required.
Q.21. A 49 year old female presents with right upper quadrant pain radiating to the right shoulder. An ultrasound establishes the diagnosis of gallstones. Her BP is 120/85 mmHg; respiratory rate 15/min; heart rate 85 bpm; Temperature 37.3 C; WBC 9 x 109 /L. What is the most appropriate management?
Correct Answer : A
As she is symptomatic, reassurance is out of the question. The two remaining options are elective laparoscopic cholecystectomy or emergency laparotomy.
Laparoscopic cholecystectomy is the preferred option here as there are no signs of gallbladder perforation. Laparotomy has higher risk as it is much more invasive.
Q.22. A 31 year old previously healthy gym instructor was involved in a road traffic accident. He sustained an intracapsular fracture of his femur requiring an operation. A hemi-arthroplasty is performed and he is admitted to the orthopaedic ward. What is the most likely complication he can suffer from?
Correct Answer : B
The most common post-operative complication is an infection, including wound and lung infections (hospital-acquired pneumonia). The femoral head has been replaced (hemiarthroplasty), therefore there is no risk of femoral head avascular necrosis.
There is a risk of pulmonary embolism however now with early mobilisation and venousthromboembolism prophylaxis, it is not the most common complication. A fat embolism is very rare.
Q.23. A 55 year old man has been admitted for an elective herniorrhaphy. Which among the following is the most likely reason to postpone his surgery?
Correct Answer : B
After a myocardial infarction, elective surgery should not be performed for the next 6 months as there is an increased risk of mortality for this specific group.
Q.24. What anatomical structure is pierced during a midline port insertion during a laparoscopic cholecystectomy?
Correct Answer : B
The linea alba is the correct answer here. As this is a midline port insertion, the linea alba is the main structure that would be pierced.
The exposure of the linea alba is usually performed by sharp dissection after which insertion of a trocar can be done.
Q.25. A 53 year old lady was sent for investigations including biopsy after being found to have a breast lump and associated changes to the skin overlying this lump that appeared red and dimpled. The biopsy result was suggestive of cancer. What is the most likely statement that would describe the histopathological findings?
Correct Answer : A
The correct answer is A. Invasive intraductal carcinoma of the breast extending to the epithelium as this is a histopathological description of the most common type of breast cancer. Given that there is an indication this is cancer in the question stem and that the question is asking for the most likely statement to be correct, the most common form of cancer should be considered.
Option B. In situ, carcinoma involving the nipple epidermis is incorrect as it describes Paget’s disease of the breast which is one o the more rarer types of breast cancer affecting the nipple.
Option C. Encapsulated adipocytes within a fibrotic stroma is incorrect as it describes a Hamartoma which is a benign breast tissue disorder.
Option D. Proliferation and expansion of the stroma with low cellularity is incorrect.
This describes the appearance of a fibroadenoma, which are benign cause of breast lumps.
Option E. Cystic formations with mild epithelial hyperplasia in ducts is incorrect.
This describes other type of benign breast tissue disease known as fibrocystic changes.
Q.26. A 31 year old woman has an injury to the right external branch of superior laryngeal nerve during a thyroid surgery. What is the most likely symptom in this patient?
Correct Answer : D
The two most important complications of nerve damage you would need to know during a thyroidectomy are :
1. Recurrent laryngeal nerve damage
2. Superior laryngeal nerve damage
A unilateral recurrent laryngeal nerve damage commonly injured results in hoarseness and for bilateral damage symptoms include aphonia and airway obstruction.
The external branch of the superior laryngeal nerve is one of the nerves commonly injured in thyroid surgery. Injury to this nerve results in the inability to lengthen a vocal fold and, thus, the inability to create a high-pitched sound (dysphonia). They would have a toned voice. This would be detrimental to a person who is a a professional singer. the So in this stem, injury to the external branch to produce of superior laryngeal nerve is likely to produce symptoms of dysphonia.
THYROIDECTOMY COMPLICATIONS :
Hypocalcaemia :
• Surgery can lead to trauma to the parathyroids, devascularization of the glands with resultant ischaemia, or removal of the glands during surgery. These would lead to decreased production of parathyroid hormones (hypoparathyrodism) which ultimately leads to decreased serum calcium.
• Acute hypocalcaemia generally presents at 24-48 hours
• Postoperative hypoparathyrodism, and the resulting hypocalcaemia, may be permanent or transient.
• The first symptms are usually tingling in the lips and fingertips. Additional findings may develop, including carpopedal spasm, tetany, laryngospasm, seizures, QT prolongation and cardiac arrest. Chvostek’s sign is facial contractions elicited by tapping the facial nerve in the pre-auricular area.
Trousseau’s sign is carpal spasm on inflation of a blood pressure cuff. Airway obstruction (compressing haematoma, tracheomalacia)
• Acute airway obstruction from haematoma may occur immediately post operatively and is the most frequent cause of airway obstruction in the first 24 hours.
• Definitive therapy is opening the surgical incision to evacuate the haematoma
• Re-intubation may be lifesaving for persistent airway obstruction.
Superior laryngeal nerve damage :
• The external branch of the superior laryngeal nerve is one of the nerves commonly injured in thyroid surgery
• Injury to this nerve results in the inability to lengthen a vocal fold and, thus, inability to create a high-pitched sound (dysphonia). They would have a mono toned voice. This would be detrimental to a person who is a professional singer.
Thyrotoxic storm :
• Unusual complication resulting from manipulation of thyroid gland during surgery in patients with hyperthyroidism
• Symptoms include: Tachycardia, tremors, cardiac arrhythmias
Wound infection : Incidence is around 1 to 2%
Q.27. A 40 year old female underwent a laparotomy one week ago. On day 6 postoperatively, you are asked to review her by the nurse in charge. The patient complains that she has not been able to open her bowels since the operation and that she has vomited twice since yesterday. Her past medical history includes hypertension, diagnosed two years ago, for which she tasks ramipril. She has a twenty pack year smoking history. She does not drink alcohol at all. On examination, the patient appears to be anxious and uncomfortable. She is also noted to be overweight. She has a distended abdomen and no bowel sounds can be auscultated. There is no tenderness on palpation, apart from some mild discomfort around the laparotomy site. A plain X-ray of her abdomen revealed gas distributed throughout the small and large gut. Minor fluid levels were seen on an erect abdominal X-Ray. Her vitals are as follows: Blood pressure 130/82 mmHg Heart rate 90 beats/min What is the next best step to manage this patient?
Correct Answer : B
The patient in the scenario has presented with a common postoperative complication: Paralytic ileus. Paralytic ileus is a condition whereby the bowel takes a while to start working again after surgery.
It can last for a few hours to a few days and may occasionally last much longer. It is more common after bowel surgery due to the manual handling of the bowel loops. This patient has a distended abdomen, produced mainly from swallowed air that cannot pass through the bowel. This impairs the blood supply of the bowel wall and allows the absorption of toxins to occur.
The fact that this patientintravenous has no bowel sounds upon auscultation helps differentiate paralytic ileus from mechanical obstruction.
A silent abdomen is more diagnostic of paralytic ileus, whereas noisy bowel sounds indicate a mechanical obstruction.
Another differentiating point is the absence of pain in this patient.
Paralytic ileus tends to have less abdominal pain compared to mechanical obstruction. The best way to treat this patient is to pass a nasogastric tube to remove the swallowed air and prevent gaseous distension.
Furthermore, intravenus fluid and electrolyte therapy should be administered with careful biochemical control. An immediate laparotomy is not required as it is not an emergency and the patient is quite stable.
Q.28. A 60 year old man has difficulty in swallowing. He has regurgitation of food and bad breath. He has been coughing a lot lately. He has lost some weight during the last couple of months and is concerned about oesophageal cancer. What is the most appropriate initial investigation?
Correct Answer : A
The bad breath and regurgitation of food points towards a pharyngeal pouch. Loss of weight can also occur in pharyngeal pouch.
Performing an endoscopy in a patient with a pharyngeal perforating the pouch could lead to a perforation.
Pharyngeal pouch (Zenker's diverticulum) : It is a herniation between the thyropharyngeus and cricopharyngeus muscles that are both part of the inferior constrictor of the pharynx.
Presentation :
• Dysphagia
• History of food sticking and regurgitation
• Aspiration (Aspiration pneumonia can also occur)
• Chronic cough
• Some may present with progressive weight loss
• Usually there are no clinical signs but there may be a lump in the neck that gurgles on palpation.
• Halitosis (bad breath) from food decaying in the pouch.
Investigations :
• Endoscopy should be avoided as an initial investigation for fear of the pouch barium lesion
. A barium swallow may show a residual pool of contrast within the pouch.
Q.29. A 28 year old female presents to the breast clinic after having noticed a lump in the left breast which has been present for one month. On examination, there are 2 smooth, regular, firm, mobile lumps on the upper outer quadrant of the left breast. Both lumps are non-tender and measure 2 cm by 2 cm. Her last menstrual period was 2 weeks ago. What is the most likely diagnosis?
Correct Answer : C
Fibroadenomas are the most common breast tumors found in adolescents and young women. Clinically, fibroadenomas are firm, nontender, highly mobile palpable lumps. It is important to remember that the most distinctive feature of fibroadenomas that distinguishes them from other breast lumps are the fact that they are highly mobile.
In fact, some small lumps may slip away from the examining hand during palpation because they are extremely mobile, giving rise to their description as “breast mice”.
Most fibroadenomas are found in the upper outer quadrant of the breast.
They are thought to result from an increased sensitivity to oestrogen.
Diagnosis is usually made with a combination of clinical assessment, ultrasonography, and fine needle aspiration cytology.
Q.30. A 62 year old lady with family history of ovarian carcinoma. A pelvis ultrasound reveals a complex mass that is 7 cm by 5 cm in the left adnexa. What is the most appropriate tumour marker to request for?
Correct Answer : A
A pelvic mass that is identified after menopause should raise the suspicion of ovarian cancer. Remember that in postmenopausal women, the ovaries should normally be atrophic so if they are felt, think of ovarian carcinoma. Among the above options, CA 125 should be taken for the possibility of an ovarian epithelial cancer.
Q.31. A 35 year old lady presents with painless bleeding from her left nipple over the past 2 days. No mass can be palpated on the breast. There are skin changes of the breast. What is the most likely diagnosis?
Correct Answer : C
Ductal papilloma is a benign breast condition and the most common cause of bloody nipple discharge in women age 20-40. A papilloma is a growth a bit like a wart.
These can grow inside the ducts of the breast, often near to the nipple. They can bleed causing a bloody discharge from the nipple.
The masses are often too small to be palpated.
They do not show up on a mammogram due to their small size.
A galactogram is therefore necessary to rule out the lesion. The other options are less likely to be the answer.
Duct Ectasia – is suggested by a green or brown nipple discharge Paget’s disease of the nipple – is suggested by breast nipple ‘eczema’
Nipple abscess – is suggested byaged a painful collection of pus forming in the breast tissue or around the nipple, usually as a result of bacterial infection.
Fat necrosis is suggested by a firm and solitary localized lump usually with a history of trauma.
Q.32. A 49 year old man had a sigmoid colectomy 48 hours ago. He is recovering well and has been apyrexial since the operation. His blood results postoperatively show a CRP of 75 and a white blood cell count of 13 x 109 /L. He is mobilising well and has started oral fluids and a light diet. He has no further complaints besides a mild abdominal discomfort. On examination, he has a soft, nontender abdomen. His surgical wounds are dry. What is the most appropriate management?
Correct Answer : D
Mild abdominal discomfort is completely reasonable for someone who just had are abdominal surgery.
A raised white cell count and CRP is not uncommon for a post-op patient and therefore antibiotics should not be initiated based on just these findings.
Single-dose antibiotics are typically given on induction and it is not unless the patient is unwell or is pyrexic that it would be appropriate to start intravenous antibiotics.
This is because anastomotic leaks and wound infections are the feared complications of sigmoid colectomy.
In this case, he is completely asymptomatic so the best answer would be to repeat the white blood cell count and CRP in 24 hours.
If these levels are seen decreasing the following day, it is a reassuring sign and no action would be required.
Q.33. A 30 year old lady has a long history of dysphagia especially when eating solid foods. Her symptoms of dysphagia has been worsening over the past few months. She notices that she regurgitates stale fluid. She also suffers from an ongoing nocturnal cough that started several months ago. What is the most likely diagnosis?
Correct Answer : B
The confusion here is the history of the long term dysphagia which some may assume that she is suffering from a long term gastro-oesophageal reflux disease which consequently gave rise to an oesophageal stricture.
However, remember that the stale food material can only point to one diagnosis which is pharyngeal pouch and so oesophageal stricture is less likely the option.
The remaining options may have regurgitation but none with stale food. Sometimes, question writers may also give a history of bad breath. The cough is due to food regurgitated into the airway.
Q.34. A 34 year old man with a history of Crohn’s disease has throbbing pain and a bloody discharge coming out via a punctum near his anus. The pain is worse when he tries to sit down. On examination, a fistula is seen passing superficially beneath the submucosa layer and does not cross the sphincter muscles. What is the most appropriate management?
Correct Answer : C
Low or simple fistulae like in this stem are usually “laid open” by cutting a small amount of anal skin and muscle to open the tract. Chronic granulation tissue is removed and the tract is left open to allow it to heal spontaneously.
It is usually packed on a daily basis until the wound starts to heal from inside out.
High or complex fistulae cannot be “laid open” because it involves cutting too much muscle and could result in faecal incontinence.
Remember, lay-open management cannot be used for fistulae that cross the entire internal and external sphincters as it will result in faecal incontinence.
A submucosal fistulae is considered a low fistulae and can be treated with lay open method Anal fistula after surgical treatment. Other methods of treatment involve antibiotics but antibiotics cannot treat the underlying fistula. It can only reduce symptom from recurrent sepsis.
Q.35. A 58 year old man presents with altered bowel habits and painless bleeding per rectum. A full blood count shows the following: Haemoglobin 82 g/L White cell count 10.2 x 109/L Neutrophils 4.1 x 109/L Platelets 350 x 109/L A sigmoidoscopy was performed subsequently which showed an ulcer. What is the most likely diagnosis?
Correct Answer : A
Rectal cancers may appear as large fungating masses or an isolated ulcer. These malignancies are usually painless but tend to bleed.
COLORECTAL CANCER CLINICAL FEATURES :
RECTAL LOCATION :
• PR bleeding - Deep red on the surface of stools.
• Change in bowel habit - Difficulty with defecation, sensation of incompleteevacuation, and painful defecation (tenesmus)
DESCENDING SIGMOID LOCATION :
• PR bleeding - Typically dark red
• Change in bowel habit
RIGHT SIDED LOCATION :
• Iron deficiency anaemia may be present.
Clinical presentation :
• Weight loss
• Mass in right iliac fossa
• Disease more likely to be advanced at presentation
Emergency presentations up to 40% of colorectal carcinomas will present as emergencies.
• Large bowel obstruction (colicky pain, bloating, bowels not open)
• Perforation with peritonitis
• Acute PR bleeding
Q.36. A 32 year old man was involved in a road traffic accident and was operated for abdominal trauma where a splenectomy was performed. On the second day postop, his abdomen becomes gradually distended and tender and he complains of epigastric fullness. He feels nauseous and vomited twice in the morning. His blood pressure has now dropped to 70/40 mmHg and he has a pulse rate of 140 beats/minute. A nasogastric tube was inserted and the patient was almost immediately relieved. What is the most likely diagnosis?
Correct Answer : A
Patients can develop acute gastric dilatation as a postoperative complication of splenectomy dilatation editing patients' stomach and abdominal surgery. This is due to disruption of blood supply to thestomach which predisposes to acute gastric dilatation.
One of the causes of acut is If the patient drinks too soon after an abdominal surgery when the stomach is still in acute ileus patient's patientspatient'spatients.
The accumulation of fluid in the stomach may induce hypovolaemic shock. In addition, patients with acute gastric dilatation may proceed to have a gastric rupture.
This will lead to the development of peritonitis.
Signs and symptoms of acute gastric dilatation include a distended and tender abdomen,epigastric fullness, nausea, vomiting and heartburn. Insertion of a nasogastric tube would allow decompression of the stomach and immediately improve the.
condition. Given that the nasogastric tube relieved his symptoms, it is unlike that this is a bleed. The other options are less likely Primary haemorrhage ? Occurs immediately after surgery or as a continuation of intraoperative bleeding.
This is usually due to an unsecured blood vessel.
Reactionary haemorrhage - Occurs within the first 24 hours and it is usually due to important venous thepatients the patient'spatients circulation blithe editingpatients' and the patients patient still important venouscirculation thus postoperative to postoperative circulation and fluid volume,
which results in rolling or slipping of ligature. It is importantto remember that postoperatively, the blood pressure would rise due to the refilling of the venous system postoperative circulationthus exposing unsecured vessels that bleed.
Secondary haemorrhage- Develops 24 hours or more after the surgery. It occurs up raw surfaces to 10 days of intravenous patients circulation post-operatively. It is usually due to infection of an operative wsurfaces causing clot disintegration and bleeding from exposed tissue.
Q.37. A 46 year old woman has offensive yellow discharge from around the left nipple area over the past few days. She has a history of a subareolar abscess 6 months ago which was treated surgically. There are no abnormal skin changes on the breast or lumps palpable. What is the most likely diagnosis?
Correct Answer : C
Ductal fistula (Mammillary fistula) is an abnormal communication between a mammary duct and the skin surface, usually near the areola, and is suggested by discharge from the para-areolar region.
A fistula may form following an incision and drainage of an abscess hence the reason that a subareolar abscess is included in the history of this stem.
Occasionally, there may be a history of a spontaneous rupture of an inflammatory mass preceding the development of the mammillary fistula.
It is managed by excising and providing antibiotic cover. Recurrence of the ductal fistula is common.
Mammary duct ectasia is also another consideration as an answer.
Duct ectasia refers to retractionsdilatation of the large and intermediate breast ducts and it is suggested by a green or brown nipple discharge. The ducts become blocked and secretions stagnate.
Occasionally, nipple retraction and a lump with local pa are seen.
Duct ectasia also occurs in patients with recurrent breast abscesses.
The infection is usually mixed anaerobic based. Breast abscess would usually present with unilateral localized pain, tenderness, erythema, purulent nipple discharge and a subareolar mass.
This was not seen in this stem. Note that breast abscess may be due to mammary duct ectasia.
Q.38. A 62 year old woman presents to the Emergency Department with per rectal bleeding that started yesterday but has been ongoing. She reports this as dark red blood. On taking a full history, she states that she has painful defecation. In the last 2 months, she has noticed a change in bowel habit. Her blood tests show: Haemoglobin 91 g/L White cell count 8.9 x 109 /L Neutrophils 3.1 x 109 /L Platelets 310 x 109 /L What is the most likely diagnosis?
Correct Answer : A
One needs to consider colorectal carcinoma in any elderly woman presenting with a change in bowel habits, and rectal bleeding in the presence of anaemia.
Q.39. A 33 year old pregnant woman of 28 weeks gestation had sustained a minor chest injury three weeks ago caused by direct trauma from her seat belt during a car accident. She presents with a left subareolar mass. The mass is painless and firm and has dimpling. What is the most likely diagnosis?
Correct Answer : D
Fat necrosis feels like a firm, round lump (or lumps) and is usually painless, but in some people it may feel tender or even painful. The skin around the lump may look red, bruised or occasionally dimpled. It is more likely to occur in high BMI women and it usually follows trauma like in this stem.
Q.40. A 28 year old pregnant woman with polyhydramnios comes for an anomaly scan at 31 weeks. On ultrasound scan, there was no gastric bubble seen. What is the most likely diagnosis?
Correct Answer : B
Diagnosis of oesophageal atresia may be suspected antenatally because of polyhydramnios and an absent fetal stomach bubble detected on ultrasound.
Oesophageal atresia Prenatal signs : Polyhydramnios; small stomach,
Absent fetal stomach bubble detected on ultrasound Postnatal: Cough, airway obstruction, secretions, blowing bubbles, distended abdomen, cyanosis, aspiration. Inability to pass a catheter into the stomach. X-rays show it coiled in the oesophagus.
Q.41. You are asked to review a 70 year old man who had a right hemicolectomy for caecal carcinoma 4 days ago as he has abdominal distension and recurrent vomiting. He has not opened his bowels since the surgery. On auscultation, there are no bowel sounds present and the abdomen looks distended. He has a temperature of 37.3 C and a heart rate of 90 beats/minute. A plain x-ray of the abdomen shows dilated small bowels. A full blood count was done of which results show: White cell count 9 x 109 /L Haemoglobin 120 g/L What is the most appropriate next management?
Correct Answer : D
The diagnosis here is paralytic ileus which is seen commonly after a prolonged surgery. It should be treated conservatively.
‘Drip and suck’ method would be the best option here.
“Drip” meaning IV fluids. “Suck” meaning pass an NGT to empty the stomach of fluid and gas. Intestinal ileus usually settles with appropriate treatment.
Q.42. A 45 year old man is scheduled to have an elective anterior resection of the rectum. What is the most appropriate antibiotic prophylaxis regimen?
Correct Answer : C
Surgical antibiotic prophylaxis is defined as the use of antibiotics to prevent infections at the surgical site. It needs to be given at the correct time and for most parenteral antibiotics that would be at the time of induction of anaesthesia.
Q.43. A 25 year old woman with longstanding constipation has severe anorectal pain on defecation. She notices streaks of blood that covers her stool. Rectal examination is impossible to perform as she is in such great pain. She recalls that the symptoms started following a particular episode of sharp intense pain on defecation. What is the most likely diagnosis?

Correct Answer : B
Anal fissures are caused by constipation and straining. Patients often remember the episode of pain when the tear occurred. The pain is so severe tht they would refuse rectal examinations. The distractor here is anal abscesses and haemorrhoids.
Anal abscesses present with painful swelling and defecation can be painful however blood is not typical.
Haemorrhoids may also present similarly with pain and bleeding (like anal fissures) however the symptoms of pain are usually intermittent (unless thrombosed where the pain is acutely severe) and do not tend to appear as streaks of blood on stools.
ANAL FISSURE Anal fissures are longitudinal or elliptical tears of the squamous lining of the distal anal canal.
• exquisite pain with defecation and blood streaks covering the stools
• The fear of pain is so intense that they avoid bowel movements (and getconstipated)
• refuse proper examination of area ? thus exam needs to be done underanaesthesia If present for less than 6 weeks ? defined as acute If present for more than 6 weeks ? defined as chronic.
Q.44. A 57 year old male presents with sudden onset of severe abdominal pain, nausea and vomiting. The pain initially started as left lower quadrant pain but is now generalized. He has a temperature of 38.9 C and a pulse of 135 beats/minute. On examination, his abdomen has generalized guarding and rigidity. He has no past medical or surgical history of note and he is not taking any regular medications. What is the most likely diagnosis?
Correct Answer : D
Sudden onset of severe abdominal pain, rigidity, and left iliac fossa pain in combination with abdominal recurrent and fever are in favour of a perforated diverticulum.
A perforated diverticulum is a very rare complication of diverticulitis. Surgical treatment for a perforated diverticulum involves resection of the affected segment Intussusception ? is unlikely as it presents with nonspecific abdominalis pharyngeal alsoisrecurrent.
Occasionally, they present with nausea and vomiting as well.
Bowel ischaemia ? also unlikely as it usually presents with moderate-to-severe colicky orare out constant and poorly localised pain.
A striking feature is that the physical findings areout of proportion to the degree of pain and, in the early stages, there may be minimal or no, tenderness and no signs of peritonitis.
In the later stageof peritonisms typical symptoms ofperitonism develop, with rebound guarding and tenderness. In the stem, or areis pouch pharyngeal likely
For example give some clues if they would like you to pick bowel ischaemia. Example, they may includ atrial fibrillation in part of the history. Sigmoid Volvulus ? Another unlikely answer.
Most often it presents with suddenonsetcolicky lower abdominal pain associated with severe abdominal distension. that hypertension Patients includewould also be unable to pass either flatus or stool.
Vomiting would occur later. N sion and an elevated temperature may be present if there is colonic perforation.However, a pharyngeal that there was another choice in the question of a perforation(perforated diverticulum), that would be a better answer.
Zenker’s diverticulum ? This is pouch definite pharyngeal pouchly incorrect as Zenker’s diverticulum rep tachycardia pouch and does not present with abdominal pain.
The usual presenting features are dysphagia, regurgitation, aspiration, chronic cough and weight loss.
Q.45. A 50 year old man is admitted for an elective herniorrhaphy. Which best criteria would lead to his elective procedure being postponed?
Correct Answer : B
After a myocardial infarction, elective surgery should not be performed for the next 6 months as there is an increased risk of mortality for this specific group
Q.46. A 55 year old man with cirrhosis of the liver complains of tiredness and right upper quadrant pain over the last few months. He has lost 8 kg in the last 2 months. The liver is palpable on abdominal examination. What is the most appropriate investigation?
Correct Answer : C
The signs and symptoms and history of cirrhosis are indicative of hepatocellular carcinoma. Alpha-fetoprotein (AFP) is a good screening test for hepatocellular carcinoma.
Q.47. An 8 year old child has oral burns is found not to be breathing well. Intubation has failed. His oxygen saturations are low. What is anatomical structure is likely to be pierced to help this child recover?
Correct Answer : A
A cricothyroidotomy would be indicated here and it involves a 2 cm transverse incision through the skin overlying the cricothyroid membrane and then straight through the cricothyroid membrane.
Q.48. A 22 year old man presents with haemoptysis. He had a tonsillectomy done 7 days ago. His blood pressure is 120/80 mmHg, pulse rate is 70 beats/minute and respiratory rate is 18 breaths/minute. What is the most appropriate next step?
Correct Answer : C
Admission and IV antibiotics would be most appropriate step. The patient should be admitted and the course of bleeding should be observed. Not every patient needs to go to theatre right away.
Secondary haemorrhage are caused by necrosis of an area of blood vessel, related to previous repair and is often precipitated by wound infection Complications of tonsillectomy Intraoperative
• Haemorrhage
• Dental trauma due to displacement of the mouth gag Immediate postoperative
• Haemorrhage; either primary or secondary.
The overall bleeding rate is 2.3–3.4% of cases
• Primary haemorrhage happens within the first 24 hours, due to inadequate haemostasis at the time of surgery or the displacement of a tie from the inferior pedicle. It would require return to theatre in up to 1% of patients, although the majority of cases can be managed conservatively.
• Secondary, or reactive, haemorrhage occurs after discharge (1–10 days) and is
• due to separation of the slough in the tonsillar bed. The readmission rate is
• approximately 5%, of which less than 1% are returned to theatre
• Temporary dysphagia
Q.49. A 40 year old manual worker presents with a swelling in the groin. He says he noticed the appearance earlier today and it is accompanied by pain. On examintion, a mass is found to be just above and lateral to the pubic tubercle. On examination, the mass is reducible and impulse on coughing is seen. What is the most likely diagnosis?
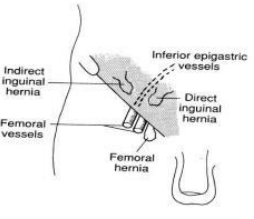
Correct Answer : A
The first hint here is his sex (male) and his occupation (manual worker). In adults, malesex and heavy lifting are risk factors for inguinal hernias
Traditionally it is taught that an inguinal hernia will lie above and medially to the pubictubercle whereas a femoral hernia lies laterally and below. This is not strictly true, as theinternal ring is always lateral to the femoral canal and
a small indirect inguinal hernia willtherefore be lateral to the pubic tubercle. A better test to differentiate the two might beto place the finger over the femoral canal for reducible hernias and then ask the patientto cough.
When the patient coughs, a femoral hernia should remain reduced while aninguinal hernia will reappear as an obvious swelling. Remember, inguinal hernias has impulse on coughing or bearing down. Femoral herniasare usually irreducible (due to the narrow femoral canal) and cough impulse rarelydetectable.
Incarcerated hernia cannot be pushed back into the abdomen by applying manualpressure and hence are irreducible. Strangulated hernia are also irreducible.
They are tense and red and usually followed bysymptoms and signs of bowel obstruction. Discrimination between direct and indirect inguinal hernia by physical examination is notvery accurate.
In an indirect inguinal hernia, the protrusion passes through the deepinguinal ring and is located lateral to the inferior epigastric artery.
Whilst traditionaltextbooks describe the anatomical differences between indirect (hernia through theinguinal canal) and direct hernias (through the posterior wall of the inguinal canal),
this is of no clinical relevance as the management still remains the same. The type ofinguinalhernia in adults is usually confirmed at the operation.
Q.50. A 43 year old diabetic, who takes regular sitagliptin, has a planned elective hernia repair surgery. What is the most appropriate advice to give regarding the perioperative management of his diabetic medication?
Correct Answer : B
Perioperative management of diabetes is often quite confusing. There's an exhaustive list and different hospitals have different protocols for diabetic medications but the general concept is still the same.
Q.51. A 64 year old man has just had major abdominal surgery. He is not a known smoker and takes no chronic medications. His post-operative pain is being effectively controlled with epidural analgesia. Ten hours post-operatively, he was noticed to have only passed 30 ml of urine in his catheter bag. The patient is otherwise alert, oriented and well. His blood pressure is 100/60 mmHg and his pulse rate is 90 beats/minute. What is the most appropriate initial step for this patient?
Correct Answer : B
The fact that he still has a catheter, the initial step would be to check the catheter. Sometimes the catheter or drainage bag tubing may be kinked and you just need to straighten it. It could also be that the catheter is blocked in which case a simple flush may fix it.
The position of the catheter and drainage back is also important whereby it should be positioned below your bladder for urine to drain.
Post-operative urinary retention cannot happen when he has a urinary catheter in situ.
Thus, there would be less of a reason to perform an ultrasound of the bladder at this stage.
In whichever case, stopping analgesia would be the wrong answer as this patient has just undergone a major abdominal surgery and requires analgesia for adequate management of his pain.
Administration of fluids may be considered if we are considering an intraabdominal bleed as a cause of an acute kidney injury resulting in decreased urine output. This is not the case here. If the patient had postoperative hypotension and consequently developed oliguria, it would be reasonable to correct this by means of a fluid challenge.
Patients can develop postoperative hypotension and decreased urine output due to several reasons, one of which is haemorrhage.
Why choose a crystalloid over a colloid for resuscitation? Theoretically, colloids exert more osmotic load and is able to keep more fluids intravascularly however there is evidence of increased rates of renal failure associated with colloid resuscitation and
one has to take into account that colloids are a lot more expensive than crystalloids.
For those reasons, clinicians prefer the use of crystalloids as a choice of fluid for resuscitation
Q.52. A 41 year old female presents to her GP concerned about the possibility of her having breast cancer. Her family history is significant for her grandmother having passed away from breast cancer, her mother having had a right mastectomy last year and her sister who was diagnosed with breast cancer at age 38 who is currently in remission from breast cancer. Gene typing was done based on her family history and the presence of the BRCA1 gene mutation were shown in this patient. Her last mammogram was 6 months ago and was found to be normal. Examination of the breast revealed no skin changes, no nipple changes and no masses. A 1 cm by 1 cm, smooth and non-tender lymph node was found in her axilla. What is the most appropriate next step for this patient?
Correct Answer : D
A prophylactic mastectomy might seem drastic at this stage but with her family history and genetic mutations, she is at a very high risk of developing breast cancer.
There are four instances in which a prophylactic mastectomy of either one or both breasts should be carried out.
These are as follows:
• Strong family history of breast cancer
• Presence of inherited mutations in one of two breast cancer susceptibility genes (BRCA1 and BRCA2)
• Previous cancer in one breast .
• Biopsies showing lobular carcinoma in situ and/or atypical hyperplasia of the breast. As we can see from the scenario, this patient ticks two out of the four boxes. The next best step for her would be a referral to a surgeon for a prophylactic mastectomy.
Women aged 50 to 70 years old are offered mammograms every 3 years. In cases like this patient where there is BRCA1 mutation, a mammogram would be offered annually from ages 40 to 69. Since she just had it 6 months ago, it is not the right answer.
The breast cancer risk should be taken very seriously, and would need precuationary steps such as organising MRI scans of the breast annually as well as mammograms for those who have a BRCA1 mutation.
An ultrasound of the breast is used in cases in which a breast lump is found during examination of the breast. A sentinel node biopsy isdone for the staging of cancers. The sentinel lymph node is the first lymph node or group of lymph nodes that drain a cancer site.
Fine needle aspiration is done if a lump was found during breast examination.
It is done after an ultrasound of the breast. Remember, prophylactic bilateral mastectomies and prophylactic bilateral oophorectomies can be offered in cases in which the patient has a strong family history of cancer and has genetic markers for the cancer.
Q.53. A 75 year old man has left-sided earache and discomfort when he swallows. There is ulceration at the back of his tongue and has a palpable non-tender cervical mass. What is the most likely diagnosis?
Correct Answer : D
Oropharyngeal carcinoma is the most probable diagnosis here. Acute mastoiditis may have ear pain but does not have discomfort when swallowing anddoes not present with an ulcer at the back of tongue.
Herpes zoster infection has a different presentation where patients complain of burning,itching or paraesthesia in one dermatome.
Although in Ramsay Hunt Syndrome thepresenting feature is often pain deep within the ear, there is usually a rash or herpeticblisters in the distribution of the nervus intermedius.
A dental abscess would present with worsening pain which may radiate to the ipsilateralear, jaw and neck with a bad taste in the mouth, fever, malaise and trismus (inability to open the mouth).
The ulceration of the tongue does not fit in this case. Tonsillitis pain may be referred to ears but on examination, reddened and swollentonsils would definitely be seen.
There would also be presence of a fever and again itwould not account for the ulceration at the base of the tongue Oropharyngeal carcinoma
Features - Typical old patient,
smoker - Persistent sore throat - A lump in the mouth or throat - Referred otalgia - Difficulty swallowing or moving your mouth and jaw - Unexplained weight loss
Q.54. A 53 year old man has become increasingly short of breath in the 3 hours since returning to the ward after a thyroidectomy. He has a temperature of 37.5 C, heart rate of 110 beats/minute, blood pressure of 90/60 mmHg, respiratory rate of 35 breaths/minute, and SaO2 of 89% on air. There are harsh inspiratory upper airway sounds and reduced air entry bilaterally. What is the most appropriate course of action?
Correct Answer : A
This is a very common question asked in the exam. Once you do a few of these questions, you would soon realise that you would be able to answer this question after reading thefirst sentence.
Anyone with shortness of breath and stridor after a very recentthyroidectomy needs their sutures cut. A rare complication of thyroidectomy is upper airway obstruction secondary to haematoma.
To prevent the airway from being totally occluded, it is necessary to releasethe pressure this haematoma is causing by loosening the tightness of the compartmentin which it is building up.
If this does not improve his breathing, this man will very soonneed intubation.
Whilst this is a rare scenario and not important per se , it is stillcommonly asked in exams. Adrenaline ? is used in anaphylaxis, which is a reasonable differential in stridor (due to laryngoedema), but is less likely here than the local effects of the surgery.
Low molecular weight heparin ? is the treatment for a pulmonary embolus, which doescause sudden breathlessness, but not due to upper airway compromise.
Oxygen ? is a reasonable response to dropping SaO2 in someone with healthy lungs but is not the treatment that is going to arrest this man’s upper airway occlusion.
Salbutamol Nebulizer ? is useful to open smaller constricting airways (e.g. in asthma or COPD) but will not reduce the pressure effect of a haematoma on the trachea.
Q.55. A 44 year old man has just had a hemi-colectomy for colorectal cancer. He is now post-op and has been put on 100% facemask oxygen. An arterial-blood gas analysis reveals: pH is 7.54 PaO2 = 28.8 kPa PaCO2 =3.8 kPa He is breathless and dyspneic. What is the best management for this patient?
Correct Answer : B
Physiotherapy is the incorrect answer. If you chose this, you might be thinking of atelectasis as the diagnosis. Atelactasis presents with much of the same signs and symptoms except it presents with hypoxia, and here we can see that the PaO2 is greater than normal.
There was no mention of a fever so IV antibiotics is the incorrect answer as well. The diagnosis here is hyperoxaemia or hyperoxia Hyperoxaemia/Hyperoxia Hyperoxaemia or hyperoxia is defined as PaO2 > 16 KpA (120 MMhG).
This kind of hyperoxia can lead to oxygen toxicity, caused from the harmful effects of breathing molecular oxygen at elevated partial pressures.
Hyperoxia differs from hypoxia in that hyperoxia refers to a state in which oxygen supply is too much, whereas hypoxia refers to the state in which oxygen supply is insufficient. Atelectasis is also known as alveolar collapse.
This is caused when airways become obstructed, usually by bronchial secretions. Most cases are mild and may go unnoticed. Symptoms are slow recovery from operations, poor colour, mild tachypnoea and tachycardia
. Prevention is by pre-operative and postoperative physiotherapy. In severe cases, positive pressure ventilation may be required
Q.56. A 24 year old woman presents with a 1 cm small smooth, firm, mobile mass in her left breast. She is very anxious and wants a form of investigation. What is the most appropriate investigation to perform?
Correct Answer : B
Generally for a woman younger than 35 years old, an ultrasound is the preferred radiological assessment. This is because young women have increased tissue density which reduces sensitivity and specificity of a mammography.
Q.57. A 35 year old diabetic man on insulin is booked in for an elective hernia operation. What is the most appropriate management plan for his diabetes on the day of the surgery?
Correct Answer : C
The patient needs to be on a sliding scale pre-operatively to maintain optimal glucose control. In the sliding scale method, insulin dose is based on your blood glucose level. The higher your blood glucose, the higher the insulin dose is adjusted to.
Every hospital has slightly different guidelines for a sliding scale. But the general key idea is to maintain ahourly monitoring of capillary blood glucose target between 4-9 mmol/L. This is done by administering insulin, dextrose and saline to keep the glucose levels between 4-9 mmol/L.
Q.58. A 66 year old woman is found to be anaemic. As part of her exam, she had a barium enema which reveals a mass lesion in the right side of the large intestine. What is the most likely diagnosis?
Correct Answer : D
A mass in the right side of the large intestine and anaemia makes caecal carcinoma the likely diagnosis from the given options.
Usually the patient presents with unexplained pain in the right iliac fossa with or without general symptoms such as anaemia, malaise and weakness.
However it is important to note that abdominal pain often develops latein the disease.
Cancers arising on the right side of the large intestine (ascending colon and caecum) tend to be exophytic.
For that reason, it very rarely causes obstruction of faeces, and presents with symptoms such as anaemia.
Q.59. A 46 year old woman presents to her local GP with the primary complaint of yellowing of her eyes and skin. She saysthat her son, who works in the United States, noticed it first when he visited home last week and she is now seeking advice upon his insistence. On further questioning, the patient reveals that she has also been suffering from constant back pain for the past few months. She thinks that her back pain is from an old university hockey injury that she sustained when she was a young woman. She admits that the back pain keeps her up at night. She also admits that she has noticed a drastic 10 kilogram weight loss in the past few weeks but thinks that is due to her not having much of an appetite any more. The patient smokes 12 cigarettes a day and has smoked for the past eighteen years. She admits to drinking alcohol more than average on a weekly basis. She has worked for over twenty years in the NHS as a nurse but is now on sabbatical. She reports no complaints in her private or professional life. Upon physical examination, the patient appears cachectic. There is marked yellowing of her sclera and her skin. There are numerous scratch marks on her torso and limbs. When questioned about them, the patient admits to feeling itchy constantly. Abdominal examination reveals a palpable mass just beneath the liver. Blood tests were done and the results are as follows: Bilirubin 28 micromol/L Alanine transferase (ALT) 76 U/L Aspartate transaminase (AST) 73 U/L Alkaline phosphatase (ALP) 329 U/L Gamma glutamyl transferase (GGT) 346 U/L A random capillary blood glucose test shows her blood glucose level to be 18 mmol/L What is the most likely diagnosis for this patient?
Correct Answer : A
This patient has cancer of the head of the pancreas. The initial signs and symptoms of pancreatic cancer are often non-specific and patients will report anything from anorexia to mid-epigastric/back pain. The pain for carcinoma of the head of pancreas is often very vague and this stem portrays it well.
By the time of patient presentation, pancreatic cancer will have often spread to other parts of the body or the entirety of the pancreas.
The clue that points to pancreatic cancer in this stem is the patient’s drastic weight loss AND the elevation of her bilirubin levels as well as all of her liver enzymes.
Liver function tests are done in patients in whom pancreatic cancer is suspected to confirm jaundice.
Liver function tests will typically show an obstructive jaundice with raised bilirubin (conjugated and total) levels.
There will also be an increase in all other live enzymes with alkaline phosphatase and gamma-glutamyl transferase being raised the most, and aspartate transferase and alanine transferase being raised to a lesser extent.
The reason for an obstructive picture is because the tumour of the head of the pancreas blocks the biliary tract. The palpable mass just beneath the liver described in this stem represents the gallbladder which is typically palpable in patients with carcinoma of the head of pancreas.
Other subtle hints that point towards pancreatic cancer is the more than average alcohol intake and smoking which are risk factors. It is important to note that alcohol does not appear to be an independent risk factor but alcohol is a risk factor towards chronic pancreatitis which may lead to pancreatic cancer.
Cholangiocarcinoma are rare adenocarcinomas of the biliary tract often presents with abdominal pain mostly localised to the right upper quadrant. The triad of cholangiocarcinoma is jaundice, right upper quadrant pain and weight loss.
Right upper quadrant pain is the main differentiating feature in this stem of cholangiocarcinoma from pancreatic cancer since the liver function tests of cholangiocarcinoma may be similar to the liver function test results of pancreatic cancer.
PANCREATIC CANCER : 60% of pancreatic tumours are adenocarcinomas which typically occur at the head of the pancreas.
Associations - Smoking , Diabetes , Chronic pancreatitis.
Features : Tumours in the head of pancreas
• Obstructive jaundice :
Dark urine
Pale stools
Pruritus
• May be painless although around 70% are associated with epigastric or left upper quadrant pain radiating to the back which may be vague. Tumours in body or tail of pancreas.
• Epigastric pain which radiates to the back and relieved by sitting forward Either tumour in head or body/tail may cause:
• Anorexia, weight loss
• Atypical abdominal pain
Investigation :
• CA 19-9 is non specific but helps assess
Prognosis :
• Transabdominal ultrasound has a sensitivity of around 60-90%
• High resolution CT scanning is the investigation of choice.
Management :
• Whipple's resection (pancreaticoduodenectomy) is considered in fit patients with no metastasis
• ERCP with stenting is often used for palliation
Q.60. You are working as a junior doctor in the surgical department. A 65 year old man is in the ward following resection of an adenocarcinoma in his descending colon. During the operation, the surgeon also opted to do a left hemicolectomy. On the tenth postoperative day, he suddenly developed left abdominal pain. By the time he had alerted the nurse to his pain, three hours had already lapsed. The pain is severe and dull in nature and worsens when he moves or turns to his sides. There is no associated nausea or vomiting. His past medical history is significant for a background of chronic obstructive disease(COPD) of which part of his medications include oral steroids. He also has a thirty pack-year smoking history. Upon physical examination, the patient appears to be anxious and lethargic. Abdominal examination reveals an area of tenderness at his left lower quadrant but no rigidity or guarding is present. Bowel sounds are sluggish. His vitals are as follows: Temperature 37.8 C Blood pressure 130/82 mmHg Heart rate 100 beats/minute What is the most likely cause of his pain?
Correct Answer : B
The scenario is quite straightforward and depicts one of the most common and feared surgical complications after anterior resection of the bowel: an anastomotic leak. An anastomotic leak is defined as a leak of the luminal contents from a surgical joint between two hollow viscera. There are several risk factors that increase the risk of an anastomotic leak developing, such as peritoneal contamination, rectal anastomosis, immunocompromised, various medications and smoking.
In this patient, there is a significant history of long term smoking. He is also a known case of chronic pulmonary obstructive disease (COPD).
Prolonged use of steroids also increases the risk of anastomotic leak.
The patient has a fever and abdominal pain which are the most common clinical features of an anastomotic leak. They usually present between five to ten days postoperatively.
This can be quite dangerous especially if it leads to peritonitis. In this question, peritonitis has not developed yet as in peritonitis, the patient usually has severe generalised abdominal pain with generalized guarding and rigidity.
A pelvic haematoma is not the correct option. Pelvic haematomas are seen in obstetric or gynaecology surgeries where bleeding results in collection of blood in the pelvic peritoneal space.
The key principle in managing an anastomotic leak is to prevent contamination and resultant sepsis. Initial management involves nil by mouth (NBM), broad-spectrum antibiotic cover and intravenous fluids.
Minor leaks may be managed through observation and bowel rest alone, with potential for percutaneous drainage if needed. For a major leak, an exploratory laparotomy is required.
Hot tip: In the exam, if a patient presents 10 days post bowel surgery with abdominal pain, it is likely to be an anastomotic leak.
Q.61. A 39 year old smoker has a thick creamy brown discharge coming from her left nipple. It has been on going for the past two weeks. She has been experiencing left breast pain for the past few months. On examination, there is a palpable subareolar mass with nipple retraction on her left breast. There are no palpable lymph nodes. Her temperature is 37.1 C. What is the most likely diagnosis?
Correct Answer : C
Duct ectasia refers to dilatation of the large and intermediate breast ducts and it is suggested by a green or brown nipple discharge. The subareolar mammary ducts become chronically inflamed, dilated and scarred. The first clue given is that she is a smoker.
Duct ectasia is associated with smoking. The other options in this question are less likely.
Breast abscess is suggested by a fluctuant lump, hot and tender, acute presentation often in puerperium, chronic after antibiotics
Fibroadenomas firm, non-tender, highly mobile palpable lumps which are usually painless
Duct papilloma is suggested by bleeding from nipple Ductal fistula (Mammillary fistula) is an abnormal communication between a mammary duct and the skin surface, usually near the areola and is suggested by discharge from a para-areolar region.
Q.62. A 52 year old man has hoarseness of voice following a thyroid surgery a week ago. There has been no signs of improvement. What is the most likely anatomical structure(s) involved?
Correct Answer : B
There is a risk of recurrent laryngeal nerve injury post thyroidectomy. If it is unilateral, it results in hoarseness. If it is bilateral, it results in aphonia and airway obstruction. Unilateral damage is more common than bilateral laryngeal nerve injury.
Q.63. A 41 year old pregnant woman presents to A&E with right upper quadrant pain that started in the last 12 hours and is gradually worsening. She has dark urine and pale stools for the last 2 days. She is noted to have a yellow sclera on examination. Her blood pressure is 145/95 mmHg. What is the most appropriate investigation?
Correct Answer : A
Symptomatic gallstone disease is the second most common abdominal emergency inpregnant women. Pregnancy alters bile composition and gallbladder emptying slows inthe second trimester, increasing the risk of gallstones.
Do not be misled into thinking this is pre-eclampsia due to the high blood pressureand RUQ pain.
Blood pressure will be raised in any patient who is in pain. Furthermore,preeclampsia does not present with symptoms of jaundice.
Ultrasound of abdomen is the best option here as an ultrasound will most likely showthe cause which is likely gallstones in this stem.
Raised urinary bilirubin with absent or reduced urobilinogen is suggestive of obstructivejaundice and will merely confirm an obstructive jaundice picture.
Alkaline phosphatase will also be raised with gallstones causing bile duct obstructionbut also can be seen raised in pregnancy. Alkaline phosphatase is not a useful test inpregnancy because of elevated levels from the placenta.
Q.64. A 32 year old female patient presents with intermittent pain in the upper outer quadrant of her left breast which radiates to the axilla. The pain is described as stabbing pain. On examination, there are no palpable lumps or palpable lymph nodes. What is the most likely diagnosis?
Correct Answer : B
Non-cyclical mastalgia is defined as pain that does not coincide with the menstrual cycle. It occurs usually around 30 to 50 years of age. It is usually unilateral and localised to one part of the breast. It is described as having a burning or stabbing pain.
While true that non-cyclical mastalgia can occasionally be caused by a fibroadenoma or cyst, there is no lump in this stem to point us in the direction of that.
Both fibroadenoma and cyst would have a palpable lump. As this stem tells us that the pain is intermittent and there is no mention of menstrual cycles, the likely answer is non-cyclical mastalgia
Q.65. A 44 year old female presents with right upper quadrant pain radiating to the right shoulder. On examination, her sclera appears yellow. Her BP is 120/85 mmHg; respiratory rate 15/min, Heart rate 85 bpm; Temperature 37.3 C; WBC 9 x 109 /L. She has no relevant past medical history and is not on any medications. What is the most appropriate investigation?
Correct Answer : A
Ultrasound of abdomen is the best answer, as this will most likely show the cause (i.e. gallstones present or not). The diagnosis here is likely to be biliary colic which presents in this manner.
As gallstones obstruct the common bile duct, it may present with jaundice.
Urinary bilirubin will merely confirm an obstructive jaundice picture. Alkaline phosphatase can also confirm a cholestatic picture.
Testing serum cholesterol will only show increased cholesterol levels, which is not very specific and does not address the cause Plain Abdominal X-ray only shows around 10% of gallstones
Q.66. A 55 year old man has a history of weight loss and tenesmus. He is diagnosed with rectal carcinoma. Which risk factor is NOT associated with rectal carcinoma?
Correct Answer : B
It is quite the opposite. A low fibre diet is a risk factor for colorectal cancers.
Q.67. A 67 year old female underwent a radical mastectomy. She now comes with the complaint of swelling and redness in her right upper limb. Which of the following structure(s) can cause these symptoms after being removed in surgery?
Correct Answer : D
Axillary node clearance Axillary node clearance increases risk of lymphoedema. The extent of axillary node clearance performed in invasive breast cancer is dependenton the likelihood of finding involved lymph nodes. The more lymph nodes that are cleared, the higher the risk of lymphoedema.
This usually presents less than a year following the operation.
Indications;
• Invasive breast cancer
• Positive sentinel lymph node biopsy Common problems associatedwith axillary lymph node clearance
• Numbness around the scar and upper arm (canbe permanent)
• Lymphoedema
• Seroma (fluid collection at the site of operation)
• Frozen shoulder
Q.68. 2 hours after an appendectomy, a 33 year old man complains of feeling unwell, having abdominal pain. He has a pulse of 128 beats/minute, a blood pressure of 88/55 mmHg and a respiratory rate of 32 breaths/minute. What is the most likely reason for his observations?
Correct Answer : A
Q.69. A 67 year old woman presents with a firm, round, painless 5 cm lump in her right breast. She has a bruise on the surface and there is no discharge. What is the most likely diagnosis?
Correct Answer : A
Fat necrosis feels like a firm, round lump (or lumps) and is usually painless, but in some people it may feel tender or even painful. The skin around the lump may look red, bruised or occasionally dimpled. Like in this question, there was a bruise noticed on the surface.
Occasionally fat necrosis can cause the nipple to be pulled in (retracted).
Sometimes within an area of fat necrosis cysts containing an oily fluid can occur.
Fat necrosis or sclerosing adenitis is suggested by a firm, solitary localized lump.
Confirmed by appearance on mammogram and benign histology Fibroadenoma is suggested by a smooth and mobile lump (‘breast mouse’), usually in ages 15-30 years old.
They are someimes described as “breast mice” because they can easily move around within the breast.
Fibroadenosis is the most common cause of breast lumps in women of reproductive age.
The peak incidence is between 35 and 50 years of age. It is a term used to describe a group of benign conditions that affect the breast.
The symptoms of fibroadenosis include breast pain (mastalgia or mastodynia), increase in breast size and lumpiness of the breast (nodularity), particularly just before or during a period Duct ectasia is suggested by a green or brown nipple discharge Breast cancer is suggested by fixed, irregular, hard, painless lump, nipple retraction, fixed to skin (peau d’orange) or muscle, and local, hard or firm, fixed nodes in axilla
Q.70. A68 year old male presents with swelling in the lower pole of the parotid gland. This swelling has been slow growing for the past 7 years. On examination, the parotid gland is firm in consistency. What is the most probable diagnosis?
Correct Answer : A
Pleomorphic adenomas are the most common cause of salivary gland tumours. It is around 10 times more common in the parotid gland than in the submandibular gland or in the sublingual gland so in the exam the stem would be most likely a parotid gland swelling. They are slow growing and painless.
Although they most often occur in the middle age, they may also be seen in the elderly like in this stem.
PLEOMORPHIC ADENOMA
- Also called benign mixed tumour
- It is the most common tumour of the parotid gland and causes over a third of submandibular tumours Features
- Presents around middle age
- Slow-growing and asymptomatic
- Solitory - Painless
- Usually mobile
- Firm single nodular mass Although pleomorphic adenomas are classified as a benign tumour, they have the capacity toundergo malignant transformation.
Treatment involves removing by superficial parotidectomy or enucleation.
Q.71. A 72 year old man presents with intermittent difficulty in swallowing with regurgitation of stale food materials. Lately me he has been having a chronic nocturnal cough. What is the most likely diagnosis?
Correct Answer : D
The stale food material can only point to one diagnosis which is pharyngeal pouch. The remaining options may have regurgitation but none with stale food. Sometimes, they also give a history of bad breath.
Q.72. A 52 year old diabetic man comes with complaints of severe pain in his anus. The pain started a week back and has gradually increased in severity. The pain is throbbing in nature and is particularly worse when he sits down and right before a bowel movement. On examination, there is a tender palpable mass noted in the perianal region with erythematous changes on the overlying skin. He has a pulse rate of 90 beats/minute and a temperature of 37.5 C. What is the most appropriate management?
Correct Answer : A
The patient has a perianal abscess. A perianal abscess is always treated with an incision and drainage which should be done immediately to prevent the formation of anal fistula. One of the common causes of anorectal pain is perianal abscess.
Perianal abscesses have a gradual onset, usually with a constant localized perianal pain. Throbbing and severe are good ways to describe a perianal abscess especially if the patient describes the pain as worse when sitting down.
Tenderness and swelling is common and occasionally with discharge. Other symptoms include constipation or pain associated with bowel movements.
Perianal abscesses need to be referred as an acute surgical emergency for incision and drainage. Antibiotics may be given after the incision and drainage.
Q.73. A 57 year old man complains of symptoms of vomiting, tiredness, and palpitations. He has lost 8 kg in the last 3 months. On examination, hepatomegaly and ascites is noted. He has a palpable left supraclaviculr mass. Records show that he is blood group A. What is the most likely diagnosis given the symptoms and risk factors?
Correct Answer : A
It is clear that this is gastric carcinoma. The vomiting, tiredness, weight loss are general features of gastric cancer. In addition, the palpitation are a symptom of anaemia. Hepatomegaly and ascites are late features of gastric cancer. The lump at the left supraclavicular region known as Troisier’s sign (an enlarged left supraclavicular node – Virchow’s node). It is indicative of gastric cancer.
People with blood group A are at a higher risk of gastric cancer.
Gastric cancer risk factors and associations :
- Increasing age
- H. pylori infection
- Blood group A
- Gastric adenomatous polyps
- Pernicious anaemia
- Smoking
- Diet: salty, spicy, nitrates
Presentation :
- Nonspecific with dyspepsia, weight loss, vomiting, dysphagia and anaemia.
- The majority of patients present with advanced disease and alarm symptomssuch as weight loss, vomiting, anorexia, abdominal pain and anaemia.
- Signs suggesting incurable disease - eg, epigastric mass, hepatomegaly, jaundice, ascites,
- Troisier's sign - an enlarged left supraclavicular node - Virchow's node.
Q.74. A 72 year old male is due for a lower anterior resection of the colon due to colorectal carcinoma. What is the prophylactic regimen to be given in theatre in his case?
Correct Answer : A
Colectomies are performed to treat and prevent diseases and conditions that affect the colon and rectum. These diseases are usually cancer of the colon or rectum or both but can also incude inflammatory bowel disease as well as diverticulitis.
Regardless of the type of procedure that is being performed, prophylactic antibiotics are needed for all colectomies.
This is due to the colon and rectum being a reservoir for faecal matter and having the potential to cause serious infections.
Prophylactic antibiotics are usually administered within 30 minutes of the first incision and are given by the anaesthetist.
There is no hard & fast rule on antibiotic choice for colorectal procedures, however, the antibiotics chosen for antimicrobial prophylaxis should have activity against the anaerobic and aerobic floras of the bowel.
Cefuroxime have good coverage of gram positive and negative bacteria and metronidazole works well against anaerobic bacteria. Always check your local antibiotic policy before administering antibiotics.
To summarise, a common prophylactic antibiotics for an anterior resection of the colon is a cephalosporin and metronidazole.
NB: a lower anterior resection is the new term for an anterior resection.
Q.75. A 35 year old day 1 post caesarean section complains of inability to void. She denies dysuria but complains of fullness. She was given an epidural for analgesia. What is the most appropriate investigation?
Correct Answer : B
Bladder scan is the correct answer here.
Women would be catheterised during the C-section. Infection control and continence guidelines specify that newly inserted urinary catheters should be removed within 48 hours to reduce urinary sepsis and restore normal bladder function as quickly as possible.
In a routine elective C-section, this would usually be on the same day or the next day.
Most catheters can be removed promptly using a trial without catheter (TWOC) procedure.
Postoperative urinary retention occurs due to the effects of the epidural during a C section. In practice, after taking out the catheter, doctors or nurses would ensure the patient is aware of symptoms of urinary retention such as passing small volumes, hesitancy or having the feeling of a full bladder that is unable to empty.
If postvoid residual volumes on bladder scan (PVRVs) are 300-500 ml and patient unable to void or uncomfortable, or if PVRV > 500 ml, the usual management would be to reinsert catheter.
Q.76. During a routine colonoscopy for colorectal cancer screening, a 64 year old man was found to have grade 3 haemorrhoids. On questioning after the procedure, he says that the haemorrhoids do not cause any pain or rectal bleeding. What is the most likely management?
Correct Answer : A
A grade 3 haemorrhoidectomy without bleeding or pain does not need to be treated unless they bother the patient. Remember, no matter how terrible the haemorrhoids look, they do not need to be treated unless they are symptomatic!
HAEMORRHOIDS :
Haemorrhoids can be described as excessive amounts of normal endoanal cushions. They are associated with constipation and chronic straining.
Haemorrhoids can be divided into:
• Internal - Originating from the vascular anal cushions
- Painless, fresh rectal bleeding
• External - Originating from perianal vessels (originate below the dentate line)
- Pain, itching, and swelling Internal haemorrhiods can be classified into 4 grades :
• Grade I: No prolapse out of anal canal, just prominent blood vessels
• Grade II: Prolapse seen when strains but spontaneously reduces and returns
• Grade III: Prolapse seen when strains requiring manual reduction
• Grade IV: Prolapse seen and cannot be manually reduced
Management - Conservative and medical management
• Digital replacement of prolapsed haemorrhoid - Often relieves the pain
• Avoid straining and constipation by using laxatives or bulking agent.
• Local anaesthetic creams and ointments
Surgical -
• Sclerotherapy : Injection of small amount of irritant solution reducing the blood supply to the haemorrhoid eventually decreasing the size of the haemorrhoid over weeks.
• Banding : Rubber band like material is placed around the neck of the haemorrhoid which constricts the haemorrhoidal vessels which results in shriveling of haemorrhoids.
• Stapled haemorrhoid surgery : Uses a circular shaped stapling device to remove excess tissue above the haemorrhoids and the remaining tissue is stapled inside the rectum.
• Haemorrhoidectomy : Excision of haemorrhoids under general anaesthesia. Thrombosed prolapsed internal or external haemorrhoids may be treated conservatively with analgesia and ice packs applied to the area to reduce oedema and inflammation. However, these may require surgery especially if patients present within 72 hours.
Q.77. A 38 year old woman presents with itching around the breast and greenish foul smelling discharge from the nipple. She had a similar episode a year ago. What is the most likely diagnosis?
Correct Answer : B
Duct Ectasia is suggested by a green or brown nipple discharge.
The other options in this question do not present with greenish foul smelling discharge from the nipple.
Breast abscess is suggested by a fluctuant lump, hot and tender, acute presentation often in peurperium, chronic after antibiotics.
Duct papilloma is suggested by bleeding from nipple.
Fat necrosis is suggested by a firm and solitary localized lump usually with a history of trauma.
Paget’s disease of nipple is suggested by breast nipple ‘eczema’.
Q.78. A 50 year old woman who was treated for breast cancer 3 years ago now presents with increased thirst and confusion. She has recently become very drowsy. What is the most likely metabolic abnormality?
Correct Answer : A
The most common causes of hypercalcaemia are malignancy and primary hyperparathyroidism. In this scenario, breast cancer has metastasis to the bone.
Bone metastases are one of most common causes of hypercalcaemia and you should be able to associate breast cancer with bone metastases and hypercalcaemia.
Note: if in this question they were to ask about management of hypercalcaemia, intravenous saline would be the correct answer.
The first step in management in hypercalcaemia is always rehydration with IV fluids.
Q.79. A 65 year old woman has been losing weight and feels lethargic. Three years aog, she had a right hemicolectomy for cancer of the ascending colon. She looks pale on examination but there were no abnormal findings. What is the most appropriate investigation?
Correct Answer : D
Carcinoembryonic antigen (CEA) is especially important to monitor response to treatment and identify relapse in tumours showing raised CEA at diagnosis (e.g. colorectal cancers).
Q.80. A 28 year old woman who is 8 weeks pregnant has central abdominal pain for the last 36 hours. The pain is now colicky. She reports no vaginal bleeding. She has vomited once and has had an episode of loose stools earlier in the day. She has a temperature of 37.9 C. On examination, she looks ill, and has rebound tenderness in the right iliac fossa. Her urinalysis is negative. Her blood results show: Haemoglobin 130 g/L White cell count 14.2 x 109 /L CRP 130 mg/L What is the most likely diagnosis?
Correct Answer : B
The pain that has shifted towards the right iliac fossa and the fact that there is a positive McBurney’s sign and loose stools makes the diagnosis of appendicitis more likely. One cannot rule out ectopic pregnancy and so ideally an ultrasound scan would take place to confirm that the pregnancy is in utero.
However, the clinical features and the blood results in the above stem clearly show evidence of an acute appendicitis. Note that appendicitis is usually more difficult to diagnose in pregnancy as the position of the appendix is usually higher as pregnancy progresses and the uterus enlarges.
If a woman is 28 weeks pregnant, she may feel the pain at the right central abdomen or right upper quadrant.
In reality, it would be difficult to differentiate an ectopic pregnancy from appendicitis and the likely action in an unwell (but stable) patient is to perform a laparoscopy to identify the cause of the severe abdominal pain.
As this stem is pointing more towards the diagnosis of appendicitis, it would be ideal if the general surgeon took this patient to theatre and performed a laparoscopy whilst the gynaecology team is on standby to take over in the event the general surgeons find an ectopic pregnancy.
Q.81. A 63 year old woman with a history of ovarian cancer with bony metastases is admitted after having a fall. A plain X-ray of the right thigh reveals a mid-shaft femur fracture. The fracture was managed by closed reduction and percutaneous stabilisation. On the third day of her admission she complains of worsening colicky abdominal pain. She vomited four times in the last day and still feels nauseous. Her abdomen appears to be distended and is markedly tender. Bowel sounds are not appreciated upon auscultation. What is the most appropriate immediate management to relieve this patient’s pain?
Correct Answer : B
This patient likely has a paralytic ileus which can occur from long periods of immobilisation. The single best way to relieve her pain is to insert a nasogastric tube to empty the stomach of fluid and gas.
The distractor here is the palliative stoma. Advance ovarian cancers can metastasise to the bowels and cause kinks in it leading to symptoms of bloating.
If surgery was required, part of the bowel may be removed and a stoma may be created. However, given her symptoms coincide with immobilisation and are rather acute, inserting anasogastric tube would be a better answer as it would relieve the pain almost immediately.
Morphine and all its analogues would worsen her symptoms.
The matter of fact, treatment of paralytic ileus involves reducing opiate analgesia. Although endoscopic stenting can be used for palliative care, it is long term treatment and, in this case, can be considered once the patient is stable.
Q.82. A 65 year old woman presents to the breast clinic having noticed that she has had a blood stained discharge from the left nipple. She also has dry skin over the left areola which resembles eczema. On examination, a blood stained discharge with dry flaky skin is noted on the left areola and the nipple was ulcerated. What is the most appropriate investigation?

Correct Answer : C
There is suspicion of Paget’s disease of the breast/nipple here. These are usually diagnosed by having a simple skin punch biopsy.
PAGET DISEASE OF THE BREAST/NIPPLE :
This is an uncommon breast malignancy with a generally better prognosis thaninfiltrating ductal carcinoma.
Presentation :
Chronic eczematous change of the nipple with -
• Itching • Erythema • Scale formation (may mimic psoriasis)
• Erosions • Nipple discharge including bleeding
• Inverted nipple
• It usuall presents unilaterally
This image shows the scaly, erythematous, crusty, and thickened plaque on the nipple of Paget Disease of the Breast.
Q.83. A 55 year old woman presents with a sore nipple. She has been complaining of a growing rash at her nipple which is itchy. She has clear fluid discharge from her left nipple over the past few months which has recently been a little blood stained. On examination, her left nipple is dry cracked and has scaly skin. Her right nipple appears normal and no lymphadenopathy was seen. What is the most likely diagnosis?
Correct Answer : A
The signs and symptoms here are consistent with Paget disease of the breast. This is an uncommon breast malignancy. The lesion is pruritic and appears red and scaly often located in the nipple spreading to the areola.
The skin appearance can mimic dermatitis like eczema or psoriasis. Discharge may occur which may include blood stained discharge.
Fibroadenosis (or fibrocystic disease) is the most common cause of breast lumps in women of reproductive age.
The peak incidence is between 35 and 50 years of age. It is a term used to describe a group of benign conditions that affect the breast.
The symptoms of fibroadenosis include breast pain (mastalgia or mastodynia), increase inbreast size and lumpiness of the breast (nodularity), particularly just before or during a period Breast abscess is suggested by a fluctuant lump, hot and tender, acute presentation often in puerperium, chronic after antibiotics.
Duct papilloma is suggested by bleeding from nipple.
Fat necrosis is suggested by a firm and solitary localized lump.
Q.84. A 63 year old female patient presents to Accident & Emergency department with the complaint of profuse rectal bleeding. She describes having had the urge to defecate but passing a large volume of bright red blood instead. The patient also complains of a 2-day history of left lower abdominal pain which is exacerbated by eating. She last opened her bowels a day ago with loose stools. She feels nauseous but has not vomited. The patient describes her diet as consisting of mainly canned meat products. An abnormal examination reveals localised tenderness in the left lower quadrant with normal bowel sounds. However, there is no guarding or rebound tenderness. A rectal examination shows presence of blood on the examiner’s glove. The patient’s observations are as follows: Blood pressure 87/56 mmHg Heart rate 102 beats/minute Temperature 38.1 C Oxygen saturation 99% on room air Respiratory rate 20 breaths/minute What is the most appropriate management for this patient?
Correct Answer : C
This is a tricky question and has two parts. The first part is figuring out what the patient has. This patient likely has diverticular disease however colorectal cancer needs to be also considered.
Some useful definitions for diverticular disease are as follows:
• A diverticulum (plural diverticula) is a herniation of the large colon
• Diverticulosis is the presence of asymptomatic diverticula
• Diverticular disease refers to diverticula that are symptomatic
• Diverticulitis is inflammation of diverticula and is almost always symptomatic.
Diverticular disease is common in those who have a low dietary fibre intake and in those over the age of 50. It frequently presents with lower abdominal pain which is usually left-sided, bloating, constipation, rectal bleeding or features of inflammation (fever, tachycardia).
NICE Clinical Knowledge Summaries (CKS) states that all patients with diverticular disease who are symptomatic and who are haemodynamically unstable require urgent admission. This patient would need to be admitted as an acute surgical emergency for a suspected haemorrhage from a diverticulum with possible diverticulitis.
This patient would benefit from intravenous antibiotics instead of oral antibiotics. Intravenous fluids to replace fluid is also essential but not mentioned in the options. Dietary advice alone is reserved for patients who are symptomatic but who do not meet the criteria for admission. Antispasmodics have no role in the acute management of diverticulitis. Furthermore, nonsteroidal anti-inflammatory drugs (NSAIDs) should generally be avoided as it may increase the risk of diverticular perforation.
The patient would likey have a CT scan of the abdomen and pelvis to establish the diagnosis and to determine the severity. An urgent colonoscopy to treat the source of bleeding if there is diverticular haemorrhage may also be warranted. A full blood count needs to be taken to ensure the patient is not severely anaemic.
If her haemoglobin has dropped significantly, a blood transfusion would be arranged. A C-reactive protein (CRP) would also be important to include a CRP of 50 mg/L or more in this patient would suggest an acute left-sided colonic diverticulitis.
The critical point to remember for this question is that one of the complications of acute diverticulitis is a MASSIVE PER RECTAL bleed which warrants admission.
DIVERTICULITIS : Diverticulitis is the inflammation of a diverticulum.
Clinical features of acute diverticulitis ;
• Rapid onset left iliac fossa pain and tenderness
• Nausea and vomiting
• Diarrhoea
• Features of infection such as fever, raised WBC and CRP Investigations If in the hospital, computed tomography (CT) scan of the abdomen and pelvis is one that is most used to establish the diagnosis, determine the severity, and exclude other differentials.
Treatment : Antibiotics It is unlikely that the exam would ask you for the antibiotic choice, but for those who would like to know more, keep on reading.
If the patient presents to primary care and if mild, uncomplicated diverticulitis is suspected:
• Co-amoxiclave for 7 days
• Ciprofloxacin and metronidazole if the patient is penicillin allergic If the patient has a more significant episode and needs to be managed in hospital.
• Intravenous antibiotics (cefuroxime + metronidazole is a good option)
Q.85. A 12-year-old patient presents with copious diarrhea. Examination: urine output low, mucous membrane dry, skin turgor low. What is the most appropriate initial management?
Correct Answer : D
Fluid replacement. Diagnosis is severe dehydration.
Points in favour:
i) Low urine output
ii) Dry mucous membrane and
iii) Low skin turgor
Q.86. A 2-months-old child with diarrhea and vomiting for 6 days is brought in looking lethargic. What is the appropriate initial investigation?
Correct Answer : B
Random blood sugar.
Though there occurs electrolyte imbalance it is a common practice to do random blood sugar at the patient's arrival as an initial investigation.
Q.87. A 28-year-old drug user presents to the emergency department with collapse and anuria. His serum K+ 7.5 mmol/L. CXR early pulmonary edema. What is the next appropriate management?
Correct Answer : B
The key is B. IV calcium gluconate.
IV calcium gluconate is given to protect the heart from lethal arrhythmia or cardiac arrest from high potassium levels and is used to buy time while definitive management is being taken.
Actually, calcium gluconate doesn’t lower the potassium level that much but protects the heart from arrhythmia.
Q.88. A 6 week child is very sick-looking. Bloods: Na+ 124, K+ 2.8. Dehydrated. What would you choose to resuscitate?
Correct Answer : B
0.9% NS.
Rsuscitation is mostly done with 0.9% NS or ringers lactate, or hartmans solution. Here is hypokalemia.
To treat hypokalaemia the cutoff value is below 2.5 mmol/L and absence of anuria during resuscitation. Maintenance is with fluids.
Q.89. A 72-year-old woman who is taking loop diuretics is suffering from palpitations and muscle weakness. What is the electrolyte imbalance found?
Correct Answer : A
Na+ 130mmol/l, K+ 2.5mmol/l.
Loop diuretic causes hypokalemia and hyponatremia.
Q.90. A middle aged male is feeling unwell after a recent MI. The recent ECG shows prolonged QRS complex and tented T wave. Na+ 136 mmol/l, K+ 6.2 mmol/l, urea 5 mmol/l. What is the most appropriate management?
Correct Answer : A
Calcium gluconate.
ECG change of prolonged QRS complex and tented T wave are suggestive of hyperkalaemia which is further supported by K+ level of 6.2 mmol/l. So to protect the heart from arrhythmia calcium gluconate should be given.
Q.91. A 40-year-old man complains of thirst and lethargy. His BP is 140/90 mmHg, corrected Ca2+ 3.7 mmol/l. What is the most appropriate management at this stage?
Correct Answer : A
Hypercalcemia is treated by IV fluids.
Q.92. A 28-year-old drug user presents to emergency department collapsed and anuria. His serum K+ is 7.5 mmol/l. CXR shows early pulmonary edema. What is the next appropriate management for this patient?
Correct Answer : B
In severe hyperkalemia, IV calcium gluconate is given to protect the heart from cardiac arrest or life-threatening arrhythmias till definitive treatments are arranged.
Q.93. You are the medical officer / General practitioner in the hospital and the lab report of a patient shows glucose 4 mmol/l, K+ 5.2 mmol/l, Na+ 129 mmol/l. what is the most appropriate management?
Correct Answer : A
Here there is significant hyponatremia with mild hyperkalemia.
Glucose is at a lower normal level. Insulin can shift K+ in cells but this mild hyperkalemia does not need this treatment at this level. Moreover in lower blood glucose insulin may cause hypoglycemia.
So the best management option is A. NS 0.9% which will correct the electrolyte imbalance (including K+ level by renal handling).
Q.94. An 89-year-old patient has lung cancer. His Na+ 122 mmol/l. What is the treatment for this?
Correct Answer : C
Restrict fluid.
This is a case of SIADH secondary to lung cancer and in the case of SIADH even in severe hyponatremia 1st line treatment is fluid restriction.
So for this question answer is C. Fluid restriction.
Q.95. An 80-year-old man with prostatic cancer has confusion, thirst, abdominal pain and an abnormal ECG. What is the most appropriate investigation?
Correct Answer : D
Serum calcium concentration.
Confusion, thirst, abdominal pain and ECG changes (marked shortening of QT interval) are features of hypercalcemia.
So E. Serum calcium concentration is the likely option.
Q.96. A 62-year-old man has multiple liver metastasis due to adenocarcinoma with an unknown primary. He is deeply jaundiced and has ascites with edema upto the buttocks. He is now drowsy and his family are worried that he is not drinking enough. His medications include: haloperidol 1.5mg, lactulose 10ml. Bloods taken 3days ago: electrolytes normal, urea 6.5mmol/l, creatinine 89mmol/l, calcium=2.04mmol/l, albumin=17g/L, total bilirubin=189mmol/l. What is the most appropriate management of his fluid intake?
Correct Answer : A
Here serum albumin is 17. So the patient developed ascites and oedema secondary to reduced plasma colloidal osmotic pressure. Albumin infusion can help rise the colloidal osmotic pressure and improve the patients condition.
Q.97. A 61-year-old man was found with K+ 7.5 and ECG with prolong QRS complex. What is the best possible treatment option?
Correct Answer : A
In this high level of potassium BEST option is Dialysis and the most appropriate or NEXT option is IV calcium gluconate.
Q.98. A 36-year-old man has been diagnosed with diabetes insipidus. What electrolyte picture is expected to be seen?
Correct Answer : D
High serum Na, high serum osmolarity, low urine osmolarity.
Q.99. A patient is diagnosed with SIADH. Choose the appropriate biochemical change.
Correct Answer : A
Plasma Na+ decrease and urine osmolarity increase.
Q.100. A lady presents with itching around the breast and greenish foul smelling discharge from the nipple. She had a similar episode before. What is the most likely diagnosis?
Correct Answer : B
Duct ectasia of the breast or mammary duct ectasia or plasma cell mastitis is a condition in which the lactiferous duct becomes blocked or clogged. This is the most common cause of greenish discharge. Mammary duct ectasia can mimic breast cancer. It is a disorder of peri or post-menopausal age.
Q.101. A 50-year-old patient is admitted for elective herniorraphy. Which of the following options will lead to a postponement of the operation?
Correct Answer : B
MI 2 months ago.
After MI elective surgery should not be done before 6 months post MI, as operation earlier than this time has a significant increase in mortality.
Q.102. A lady with breast cancer has undergone axillary LN clearance. She develops arm swelling after being stung by a bee. What is the most likely mechanism responsible for the swelling?
Correct Answer : A
Lymphoedema. Reason is compromised lymphatic drainage of the arm due to axillary LN clearance. So if there is any inflammation or swelling, lymph drainage is compromised further giving rise to swelling of the limb of that operated side.
Q.103. A 34-year-old patient presents with 50% partial thickness burns. What should be the most appropriate management?
Correct Answer : B
IV fluids calculated from the time of burn.
Read Parkland's formula for burns calculation. IMPORTANT.
Q.104. A man presented with cellulitis and swelling. He was started on flucloxacillin. What other medication do you want to add?
Correct Answer : B
Penicillin.
Cellulitis is usually caused by staphylococcus and streptococcus. To cover both Flucloxacillin (for staphylococcus) and Penicillin (to cover streptococci) should be prescribed.
Q.105. A man has reducible bulge above the pubic tubercle, and on occlusion of the deep inguinal ring, cough impulse is present. What is the most likely diagnosis?
Correct Answer : B
Indirect inguinal
It is just below the pubic tubercle that is just below the inguinal ligament. On occlusion of deep ring cough impulse is present (means visible) as femoral hernia doesn’t come through deep ring but indirect inguinal hernia does.
Q.106. A man with anterior resection and end to end anastomosis done complains of severe pain in the chest and abdominal distension. What is the most appropriate investigation likely to review the cause this deterioration?
Correct Answer : C
As many anastomotic leak is self-limiting so laparotomy is not done unless indicated otherwise. Definitive diagnosis is made by CT scan.
Q.107. A 35-year-old male builder presented with sudden onset of severe abdominal pain. He was previously fit and well other than taking ibuprofen for a long term knee injury. On examination he is in severe pain, pulse 110bpm, BP 110/70mmHg and has a rigid abdomen. What is the most likely diagnosis?
Correct Answer : D
Perforated peptic ulcer.
NSAIDs induced perforation.
Points in favour-
1. Prolonged use of NSAIDs
2. Sudden onset of severe abdominal pain
3. Rigid abdomen
Q.108. A woman 5 days post-operative for bilateral salphingo-oopherectomy and abdominal hysterectomy has developed abdominal pain and vomiting along with abdominal distension and can’t pass gas. No bowel sounds heard, although well hydrated. What is the most appropriate next step?
Correct Answer : A
X-ray abdomen.
The diagnosis is paralytic ileas.
Causes of paralytic ileus:
i) Electrolyte imbalance
ii) Gastroenteritis
iii) Appendicitis
iv) Pancreatitis
v) Surgical complications and
vi) Certain drugs
Management of paralytic ileus:
i) Nil by mouth
ii) Nasogastric suction to alleviate the distension and remove the obstruction
Q.109. A 22-year-old woman with longstanding constipation has severe ano-rectal pain on defecation. Rectal examination: impossible due to pain and spasm. What is the most probable diagnosis?
Correct Answer : B
Anal fissure
Q.110. A 60-year-old smoker presents with cramp-like pain in the calves relived by rest and nonhealing ulcers. Examination: cold extremities with lack of hair around the ankles, absent distal pulses. What is the most probable diagnosis?
Correct Answer : B
Chronic ischemia of the limb. Intermittent claudication is a symptom not a diagnosis.
It is not a buerger’s disease as buerger occurs in younger heavy smokers (before the age of 50 years), It is not DVT as DVT pain or tenderness is not of an intermittent claudication pattern.
Though diabetes can cause peripheral vascular disease, the history of smoking and given clinical picture is more consistent with chronic ischemia of limb.
Q.111. A 35-year-old woman had an uneventful laparoscopic cholecystectomy 18 hours ago. She has a pulse 108bpm, temperature 37.8C. There are signs of reduced air entry at the right base but the CXR doesn’t show an obvious abnormality. What is the most appropriate management strategy?
Correct Answer : D
Chest physiotherapy
Atelectasis can be seen in chest x-ray but sometimes it becomes undetectable in chest x-ray as we are suspecting in this case.
Q.112. A 60-year-old patient recovering from a surgery for toxic goiter is found to be hypotensive, cyanosed in the the RR (recovery room). Examination: tense neck. There is blood oozing from the drain. What is the most likely diagnosis?
Correct Answer : B
Reactionary haemorrhage.
In the recovery room, cyanosis, hypotension, tense neck, oozing of blood from the drain, all these go in favour of reactionary haemorrhage. "Reactionary," hemorrhage that occurs within the first 24 hours after surgery.
Q.113. A 49-year-old patient presents with right hypochondriac pain. Investigation show a big gallstone. What is the most appropriate management?
Correct Answer : A
Lap Cholecystectomy.
As symptomatic only reassurance is not appropriate
ii) As big stone ursodeoxycholic acid is less effective
iii) Less invasive is preferred so laparoscopic rather than laparotomy.
Q.114. A footballer has been struck in the groin by a kick and presents with severe pain and mild swelling in the scrotum. What is the most appropriate next step?
Correct Answer : C
Exploratory surgery - To exclude torsion.
Q.115. A 45-year-old woman comes with red, swollen and exudating ulcer on the nipple and areola of right breast with palpable lump under the ulcer. What do you think is causing this skin condition?
Correct Answer : B
Infiltration of the lymphatics by the carcinomatous cells.
Q.116. A 66-year-old man, an hour after hemicolectomy has an urine output of 40ml. However, an hour after that, no urine seemed to be draining from the catheter. What is the most appropriate next step?
Correct Answer : D
Check catheter
Q.117. A 67-year-old woman has presented with hard, irregular, poorly defined 5cm lump in her right breast. She has a bruise on the surface and there is no discharge. What is the most likely diagnosis?
Correct Answer : B
Fat necrosis.
Fat necrosis usually occurs following trauma or surgery. Given case is a fat necrosis of breast as there is no discharge and there is a bruise indicating prior trauma.
Q.118. A 67-year-old female who had undergone a radical mastectomy now comes with the complaint of swelling and redness in her right upper limb. Involvement of which of the following structures explain these symptoms?
Correct Answer : D
Axillary group of LN.
Axillary clearance compromise lymphatic flow and may results in swelling of upper limb.
Q.119. A 68-year-old male presented with swelling in the lower pole of the parotid gland for the last 10 years. Examination: firm in consistency. What’s the most probable diagnosis?
Correct Answer : A
Pleomorphic adenoma.
Pleomorphic adenoma (most common) - also called benign mixed tumour: is the most common tumour of the parotid gland and causes over a third of submandibular tumours.
They are slow-growing and asymptomatic, having a malignant potentiality.
Q.120. A 28-year-old shipyard worker was admitted for pain in calf while at work which has been increasing over the last 3 months. There is no history of HTN or DM but he is a smoker. Exam: loss of posterior tibial and dorsalis pedis pulsation along with a non-healing ulcer at the base of the right 1st MTP (metatarsophalingeal joint) joint. What is the most probably diagnosis?
Correct Answer : A
Thromboangitis obliterans.
i) Young age
ii) Smoker
iii) Pain in cuff
iv) Loss of posterior tibial and dorsalis pedis pulsation
v) Non-healing ulcer at the base of the right 1st MTP joint all are suggestive of Buerger’s disease.
Q.121. A 35-year-old construction worker is diagnosed with indirect inguinal hernia. Which statement below best describes it?
Correct Answer : D
Passes through the deep inguinal ring.
Q.122. A 55-year-old man has been admitted for elective herniorraphy. Which among the following can be the reason to delay his surgery?
Correct Answer : D
MI 2 months ago better go for surgery 6 months post MI as surgery before this has a higher mortality rate.
Q.123. A man on warfarin posted for hemicolectomy. As the patient is about to undergo surgery. What option is the best for him?
Correct Answer : D
Stop warfarin and add heparin
Q.124. A 48-year-old lady presents with itching, excoriations, redness, bloody discharge and ulceration around her nipple. What is the most likely diagnosis?
Correct Answer : A
Paget’s disease of the breast
Q.125. Patient with widespread ovarian carcinoma has bowel obstruction and severe colic for 2 hours and was normal in between severe pain for a few hours. What is the most appropriate management?
Correct Answer : C
Palliative colostomy.
Cancer or chemotherapy induced obstructions are unlikely to respond to conservative management (NBM, IV fluid, nasogastric suction) and hence only analgesia will not relieve it. So in such cases we have to go for palliative colostomy.
Q.126. A patient presented with history of swelling in the sub-mandibular region, which became more prominent and painful on chewing. He also gave history of sour taste in the mouth, the area is tender on palpation. Choose the most probable diagnosis?
Correct Answer : A
Chronic recurrent sialadenitis.
Pain, swelling, more pain on chewing, tenderness, and swelling of the submandibular region suggests the diagnosis of submandibular chronic recurrent sialadenitis, usually secondary to sialolithiasis or stricture.
Q.127. A lady, post-colostomy closure after 4 days comes with fluctuating small swelling in the stoma. What is the management option for her?
Correct Answer : A
Local exploration
Q.128. A T2DM is undergoing a gastric surgery. What is the most appropriate pre-operative management?
Correct Answer : D
Stop oral hypoglycemic the prv night and start IV insulin with glucose and K+ before surgery.
Q.129. A 70-year-old man had a right hemicolectomy for ceacal carcinoma 6 days ago. He now has abdominal distension and recurrent vomiting. He has not opened his bowels since surgery. There are no bowel sounds. WBC=9, Temp=37.3C. What is the most appropriate next management?
Correct Answer : D
NG tube suction and IV fluids.
The patient has developed paralytic ileus which should be treated conservatively. But as in such cases in cancer patients conservative management may not respond and laparotomy may be considered.
Q.130. Which of the following formulas is used for calculating fluids for burn patients?
Correct Answer : C
4 x weight (kgs) x area of burn = ml of fluids
Parkland's formula
Q.131. A 45-year-old man underwent an emergency splenectomy following a fall from his bicycle. He smokes 5 cigarettes/day. Post-operation, despite mobile, he develops swinging pyrexia and a swollen painful left calf. His CXR shows lung atelectasis and abdominal US demonstrates a small sub-phrenic collection. What is the most likely risk factor for DVT in this patient?
Correct Answer : D
Splenectomy.
Splenectomized patients have an increased risk of developing deep vein thrombosis and pulmonary embolism.
Q.132. A 45-year-old man had cancer of head of pancreas which has been removed. He has a history of longstanding heartburn. He now comes with rigid abdomen which is tender, temp 37.5C, BP 90/70mmHg, pulse 120bpm. What is the next step of the investigation?
Correct Answer : B
X-ray abdomen will help diagnose perforation by showing gas under the diaphragm. This is a case of perforated peptic ulcer with the features of shock, abdominal rigidity, and raised temperature.
Stress from serious disease and operation causes the body to produce higher amounts of acid, which can irritate preexisting ulcers leading to easy perforation.
Q.133. A 64-year-old woman has been treated for breast cancer with tamoxifen. What other drug should be added to her treatment regime?
Correct Answer : A
Bisphosphonates reduce the risk of bone metastasis in cancers and are normally taken as adjuvant therapy in many types of tumours including breast cancer. Plus it prevents bone resorption.
Q.134. A 6-year-old came with full thickness burn. He is crying continuously. What is the next step of management?
Correct Answer : B
Here already mentioned full-thickness burn which is painless. Children often cry from anxiety about hypoxemia and hypovolaemia rather than pain. The patient then responds better to oxygen or increased fluid administration rather than to narcotic analgesics.
Q.135. A 75-year-old woman presents to the breast clinic having noticed that she has had a blood stained discharge from the left nipple, together with dry skin over the left areola. Exam: blood stained discharge with dry flaky skin noted on the left areola. The nipple was noted to be ulcerated. What is the most appropriate investigation?
Correct Answer : C
Punch biopsy.
As the lesion is on the surface punch biopsy can be well obtained.
Q.136. A 46-year-old woman has offensive yellow discharge from one nipple. She had a history of breast abscess 3 years ago. What is the possible diagnosis?
Correct Answer : C
Duct fistula
Q.137. A 45-year-old woman presents with discharge from the left nipple. The discharge is brownish-green and foul smelling. What is the most likely diagnosis?
Correct Answer : C
Women near menopause are more affected by duct ectasia characterized by brown, green, or cheesy discharge. This condition is harmless and tends to clear up without treatment.
Q.138. A 17-year-old boy while playing football got a kick and now he is complaining of severe pain and swelling of the left side of his scrotum. What investigation is the most appropriate to diagnose?
Correct Answer : D
Surgical exploration of scrotum.
This is a case of testicular torsion which needs urgent diagnostic and therapeutic surgical exploration of the scrotum.
Q.139. A 57-year-old male presents with sudden onset severe abdominal pain and rigidity against a 4 days background of LIF (left iliac fossa) pain and pyrexia. He has no past medical or surgical history of note and isn’t on any medicine. What is the most likely diagnosis?
Correct Answer : D
Perforated diverticulum.
Sudden onset, severe abdominal pain, rigidity, left iliac fossa pain and fever are in favour of perforated diverticulum.
Q.140. A 20-year-old male smoker is noted to have intense rubor of the feet and absent foot pulse. Examination: amputated right 2nd toe. What is the most probable diagnosis?
Correct Answer : C
The traditional diagnosis of Buerger's disease is based on 5 criteria (smoking history, onset before the age of 50 years, infra popliteal arterial occlusive disease, either upper limb involvement or phlebitis migrants, and absence of atherosclerotic risk factors other than smoking).
As there is no specific diagnostic test and an absence of positive serologic markers, confident clinical diagnosis should be made only when all these 5 criteria have been fulfilled
Q.141. A 44-year-old woman with breast cancer had an extensive removal and LN clearance. She needs an adjunctive treatment. Her mother had cancer when she was 65. Which of the following factors will be against the treatment?
Correct Answer : D
Her age.
Chemotherapy may result in premature ovarian failure.
Q.142. A patient on insulin is booked in for a hernia operation. What is the most appropriate management of insulin?
Correct Answer : C
Give IV insulin + dextrose + saline pre-op
Q.143. A 26-year-old presents with prolonged constipation, blood on side of stool and very painful defecation. PR examination: very painful. What is the most likely diagnosis?
Correct Answer : D
Anal fissure
Q.144. A 26-year-old male has been operated for abdominal trauma and splenectomy was done. On the 3rd post-op day the patient developed acute abdominal pain and distention in the upper abdominal area with hypotension. On insertion of ryles tubes, 2L of coffee ground fluid was aspirated. What is the most probable diagnosis?
Correct Answer : A
Acute gastric dilatation may be caused by:
Hyperglycaemia,
Childbirth,
Abdominal injury,
Application of a spinal cast, rarely, after abdominal surgery when the stomach is in ileus and drink has been taken too soon.
The abdomen is distended and tender. The patient complains of epigastric fullness, nausea, heaviness, and heartburn.
There is a succussion splash. The accumulation of fluid in the stomach may induce hypovolaemic shock. Reflux of gastric contents may cause aspiration pneumonia.
Q.145. 2 hours after an appendectomy, a patient complains of a rapid HR (heart rate) and fever. He says there is alsoabdominal pain and pain in the shoulder area. What is happening to this patient?
Correct Answer : A
Intra-abdominal bleeding
Q.146. A diabetic man feels hot, painful lump near the anal region. What is the most probable diagnosis?
Correct Answer : B
Abscess.
Diabetic patients are much more prone to infection.
Q.147. A 65-year-old lady with type 1 diabetes mellitus for the last 20 year comes with a tender lump near the anal opening. She says she also has a fever. What treatment should she get?
Correct Answer : A
I&D + antibiotics
D/D 1. Perianal abscess
2. Perianal hematoma
3. Thrombosed piles.
As infection is common in DM likely case is perianal abscess.
Q.148. 2 hours after an appendectomy, a patient complains of a rapid HR (heart rate) and fever. He says there is also abdominal pain and pain in the shoulder area. What is the first step in the management?
Correct Answer : A
Maintain IV access and give IV fluids.
Q.149. A 65-year-old man on dexamethasone underwent surgery. During and after the surgery, his blood glucose was around 17-19 mmol/l. What will you give the patient?
Correct Answer : A
Insulin.
If the patient is on dexamethasone there may be suppression of pituitary adrenal axis suppression. In such patient, operation may precipitate adrenal insufficiency and to prevent this corticosteroid coverage with additional dexamethasone is given.
This may lead to hyperglycemia. If this hyperglycemia is significant (as given in the present question) insulin should be given.
Q.150. A 60-year-old man presents with mass in the groin. Examination: mass lies below the midpoint of the inguinal ligament and is pulsatile. What is the most probable diagnosis?
Correct Answer : D
Femoral aneurism.
Hernia below pubic tubercle (below inguinal ligament) is a femoral hernia. But below the mid-inguinal point and pulsatile mass is femoral aneurism.
Q.151. A 40-year-old manual worker presents with a swelling in the groin. Examination: mass is found to be just above and lateral to the pubic tubercle. It is reducible. On applying pressure on the internal ring there is no cough impulse seen. What is the most probable diagnosis?
Correct Answer : B
Indirect inguinal hernia.
Swelling in the groin; mass just above and lateral to the pubic tubercle means inguinal hernia. It is reducible.
On applying pressure on the internal ring, there is no visible cough impulse; it means the hernia enters the deep ring, and the scrotum passes through the superficial ring.
That means it is an indirect inguinal hernia.
Q.152. A 25-year-old woman who is 11 weeks pregnant had central abdominal pain for 36 hours. The pain is now colicky. There is no vaginal bleeding. She has vomited once and has had an episode of loosen motion. She looks ill, temp=37.8C and there is rebound tenderness in the RIF. What is the most probable diagnosis?
Correct Answer : C
Appendicitis. No vaginal bleeding and pain above the pelvis make pregnancy complications less likely.
Loose motion, low-grade temperature, and positive Mc Burney’s sign make the diagnosis of appendicitis more probable.
Q.153. A 40-year-old woman presents with dysphagia. Examination: febrile with erythema and middle neck swelling. What is the best management strategy?
Correct Answer : A
IV antibiotics and drainage.
Neck abscess. Treated with IV antibiotics and drainage.
Q.154. A lady developed breast abscess after delivery. What is the most likely organism?
Correct Answer : A
Staph aureus
Q.155. A 55-year-old man presents with swelling at the angle of the mandible which is progressively increasing in size and it’s mobile for 6 months. What is the most probable diagnosis?
Correct Answer : A
Benign parotid. Mandibular tumour or tonsillar carcinoma would not be so mobile after such a period.
Q.156. A 55-year-old male has been admitted for elective herniorraphy. Which among the following can be the reason to delay his surgery?
Correct Answer : D
MI 2m ago.
Following MI at least 6 months should be elapsed for elective operation. Prior to this time surgery is associated with increased mortality.
Q.157. A 17-year-old girl with a lump in her breast was seen in the clinic. Examination: the lump was free and mobile and not attached to the skin. Her mother wants further tests done. What should be the next step?
Correct Answer : B
USG breast.
The described lump is fibroadenoma. The next investigation is either the US breast (for women under 35 years) or mammography (for women over 35 years).
Q.158. A lady with a firm smooth breast lump in outer quadrant had a FNAC done. Results showed borderline benign changes. She also has a family history of breast cancer. What is your next step?
Correct Answer : C
Core biopsy.
Genetic testing is done for asymptomatic patients in their 30s but the given case is symptomatic.
If FNAC was not borderline we could withhold core biopsy in favour of genetic counseling and if positive SERMs are given which cause significant reduction in cancer.
Q.159. A 65-year-old man had a bowel resection 5 days ago. He is anuric and breathless. His BP=150/110mmHg. He has crackles at both lung bases and sacral edema. Bloods: K+=6.8mmol/l, urea=58mmol/l, creatinine=600umol/l. What is the most appropriate immediate management?
Correct Answer : D
10U insulin, 50ml of 50% dextrose infusion. There is a renal failure with hyperkalemia.
First, we have to save the heart from arrest or life-threatening arrhythmia by shifting K+ into the cell. 10U insulin in 50 ml 50% dextrose will help do this.
Q.160. A 38-year-old man presents with acute infection of skin in the leg. Diagnosis of cellutitis has been made. What medicines should be prescribed?
Correct Answer : A
Penicillin + Flucloxacillin.
Cellulitis is usually caused by bacteria, such as staphylococci or streptococci that are commonly present on the skin.
So Penicillin + Flucloxacillin should be given.
Q.161. A boy was admitted with partial thickness burn, what is your next step?
Correct Answer : D
Refer to the burn unit
Q.162. A 32-year-old woman has undergone a biopsy for a breast lump. The report says: a well circumscribed lump with clear margins and separated from the surrounding fatty tissue. What is the most appropriate interpretation of this report?
Correct Answer : D
Fibroadenoma.
Fibroadenomas are the most common benign tumor of the female breast. White, well-circumscribed mass is clearly demarcated from the surrounding yellow adipose tissue.
Q.163. A 23-year-old female presented with a swelling of her neck that moved upwards on protrusion of tongue. What is the next appropriate investigation?
Correct Answer : A
The diagnostic investigation of thyroglossal cyst is FNAC. Then we palpate for thyroid tissue. If absent, we do one of the following to confirm the absence of thyroid tissue: ultrasonography, CT scanning, thyroid scanning or MRI.
If there is normal thyroid tissue we go for a more aggressive Sistrunk's operation but if there is no normal thyroid tissue [in that case thyroglossal cyst itself may be the only source of thyroid tissue] we do conservative surgery and preserve some portion of the cyst with thyroid tissue.
Q.164. A 35-year-old man has had acute pain and swelling below the mandible on the left side for 2 hours. The swelling occurred after eating a large meal. What is the most likely diagnosis?
Correct Answer : D
Submandibular calculus.
Pain and swelling below the mandible are due to a stone in the submandibular salivary gland duct.
Pain and swelling increased after a large meal as the saliva produced during the meal could not come out of the gland due to stone.
Q.165. A patient is about to undergo surgery. Her Hgb 8.9g/dl and MCV=70. What is the best option for her?
Correct Answer : A
Investigation and postpone the surgery.
For elective operation only proceed if Hb% > 10 g/dl. If Hb% < 10 g/dl then defer the operation and investigate first. If Hb% < 8 g/dl also must be transfused.
Q.166. A 24-year-old male presents with discomfort in the groin area and scrotal swelling. Exam: scrotal skin is normal. What would be the next best step?
Correct Answer : C
OPD referral.
A case of inguinal hernia or hydrocele. In both torsion or epididymo-orchitis, scrotal skin will be inflamed (erythematous and oedematous). As the skin is not inflamed the patient should be referred to Surgery OPD, as its not a emergency.
Q.167. A pregnant woman had hit her chest 3 weeks ago. Now she is 24 weeks pregnant and presents with left upper quadrant mass with dimpling. What is the most probable diagnosis?
Correct Answer : D
Fatty necrosis of breast
Q.168. Which of the following conditions requires operative management?
Correct Answer : D
Fournier’s gangrene.
Fournier's gangrene: A horrendous infection of the genitalia that causes severe pain in the genital area (in the penis and scrotum or perineum) and progresses from erythema (redness) to necrosis (death) of tissue. Gangrene can occur within hours.
Q.169. A 79-year-old man has a swelling of the right groin which was clinically diagnosed to be indirect inguinal hernia. What is the feature of the hernia sac that would confirm the diagnosis?
Correct Answer : D
Passes through the deep inguinal ring.
Ingunal hernia lies mostly above and medial (occasionally lateral particularly when small) to pubic tubercle. It first enters the inguinal canal through the deep inguinal ring and then enters the scrotum through the superficial inguinal ring.
Q.170. A 56-year-old woman with history of breast cancer 10 yrs ago has undergone radical mastectomy and axillary lymph node removal, now complains of swollen upper limb 3 weeks after an insect bite. The bite site is better but gross edema is still present. What is the cause?
Correct Answer : A
As during mastectomy axillary clearance is done, lymphatics on that upper limb are compromised. So there occurs lymphedema.
Q.171. A patient after his house fire came with hematemesis with erosion/ulcer of esophagus and on examination there is 55% burn and on endoscopy there is a stomach/gastric erosion and soot in the mouth. What is the treatment?
Correct Answer : D
Tracheal intubation.
If a burnt patient gets soots in the mouth and /or nose tracheal intubation is done.
GI ulceration (here oesophageal and gastric ulcers and erosions) due to burns are known as curling ulcers.
Q.172. A man rescued from a building on fire presented with unconsciousness without any evidence of burns or external injury or soot. What would you do next?
Correct Answer : A
100% oxygen inhalation.
In CO poisoning 100% oxygen is the initial management and also there is a role of hyperbaric oxygen in a hyperbaric chamber.
Q.173. A man presented with a purplish swelling at the anal area. It is acutely painful and he complains of constipation for the last 2 months. What is the most appropriate management?
Correct Answer : B
Excision is the method which is done in case of hemorrhoid , not incision.
This is a case of perianal hematoma which when clotted is treated by incision and left open with excellent result of healing with the aids of antibiotics and prophylaxis. It occurs in case of constipation.
The answer is B. Incision and drainage + antibiotics. In acute cases prior to thrombosis can be treated with evacuation with a syringe.
Q.174. A 55-year-old man presented with hot, raised, tender area of skin on his right leg. He is febrile with rigors. He has been started on flucloxacillin. What other medication will you add?
Correct Answer : D
Abscess, cellulitis, furuncle these lesions are usually caused by Staphylococcus and streptococcus.
So Benzylpenicillin should be added with flucloxacillin to cover streptococcus.
Q.175. A man feels mild discomfort in the anal region and purulent discharge in underpants. What is the most likely diagnosis?
Correct Answer : C
Fistula in ano. Abscess is with severe pain which may reduce after it bursts with purulent discharge. But here mild discomfort and purulent discharge favours the diagnosis of fistula.
Q.176. A 30-year-old woman has a painless lump in the outer aspect of her left breast. She has had a previous breast lump. Her grandmother had breast cancer at 70 years. She has a 1 cm smooth, firm, discrete, mobile lump in the other quadrant region of the left breast. What is the most likely diagnosis?
Correct Answer : D
H/O previous bre?st lump and presently with a lump of 1 cm size which is smooth, firm (not hard), discrete and mobile (not fixed) suggests fibroadenoma.
Q.177. A 35-year-old woman complains of hoarseness of voice 3 hours after partial thyroidectomy. She had no history of phonation problems before the surgery. What is the most appropriate investigation?
Correct Answer : A
Laryngoscopy.
Probable diagnosis is recurrent laryngeal nerve palsy.
Q.178. A 60-year-old patient recovering from a surgery for toxic goiter is found to be hypotensive, cyanosed in the recovery room. Exam: neck is tense. There is oozing of blood from the drain. What is the most probable diagnosis?
Correct Answer : B
Reactionary hemorrhage.
Hemorrhage within 1st 24 hours which usually occurs due to dislodgement of clot or slippage of a ligature.
Q.179. A 40-year-old woman has had varicose vein surgery, planned as a day patient. After the operation, she is distressed by repeated retching and vomiting. Her pain is currently well controlled. What is the best management strategy?
Correct Answer : D
As there is repeated retching and vomiting patient cannot keep oral medication down.
So IV ondansatron should be given.
Q.180. An 88-year-old woman is a known smoker. She had an attack of MI 2 years back and is known to have peripheral vascular disease. She presents with an irreducible herniation over the incision region of a surgery which she underwent in her childhood. What is the most appropriate treatment?
Correct Answer : B
Truss can not be used as the hernia is irreducible; urgent herniorrhaphy in strangulation; elective herniotomy. In herniotomy the hernia may recur; only reassure is not an option as irreducible hernia may become strangulated or may develop intestinal obstruction.
Q.181. A 62-year-old man has had ano-rectal pain aggravated by defecation for 3 days. Rectal examination: purple, tender lump at the anal verge. Flexible aigmoidoscopy: normal rectal mucosa and hard feces. What is the diagnosis?
Correct Answer : A
Anal hematoma
Q.182. A 63-year-old male undergoes abdominal surgery. On Monday morning, 3 days postoperative, repeat samples confirm serum K+ 7.1 mmol/l. His ECG shows broad QRS complexes. Which one of the following can be used as an effective treatment for this pt’s hyperkalemia?
Correct Answer : B
Calcium gluconate does not shift potassium into cells or reduce its level but prevents its arrhythmogenic effect on the heart and buys time till definitive measures are taken.
Q.183. A lady with post ileo-colectomy closure of stoma has a small 4cm swelling around the stoma. What is the most appropriate management of the swelling?
Correct Answer : A
Local exploration of swelling
Q.184. A woman became acutely SOB (short of breath) in the recovery bay and is coughing after GA. Auscultation: reduced air entry at the right lung base and diffuse wheeze. Observation: HR 88 bpm, BP 112/76 mmHg, temp=37.8C and saturation 91% in air. Choose among the options which C-section complication has she developed?
Correct Answer : A
Diffuse wheeze, reduced air entry at lung base and raised temperature favours the diagnosis of aspiration pneumonitis.
Q.185. A 35-year-old woman presents with mass in the groin. Examination: mass found just below and lateral to the pubic tubercle. There is no cough impulse and it is irreducible. What is the most probable diagnosis?
Correct Answer : C
Mass below and lateral to the pubic tubercle is suggestive of femoral hernia.
Q.186. A lady presents with a swelling below the groin crease that can be reduced. There is no medical history of note. What is the most probable diagnosis?
Correct Answer : D
Femoral hernia
Q.187. A 45-year-old mechanic presents with a reducible swelling in the groin, impulse on coughing is present. He has mild dragging pain in the abdomen, otherwise he’s normal. What is the best management strategy?
Correct Answer : B
Elective herniorrhaphy.
Usually before the age of 30, the recurrence rate of hernia after herniotomy is much less but after 30 recurrence is high. So Herniotomy is done at the age of less than 30. As the presenting case is 45 yrs we should do herniorrhaphy in this patient.
Q.188. A 25-year-old man present with a mass in the groin after heavy lifting. Examination: mass is found just above and medial to the pubic tubercle. It is reducible. On applying pressure on the internal ring, cough impulse is still present. What is the most likely diagnosis?
Correct Answer : A
On occlusion of deep inguinal ring if cough impulse still present (visible cough impulse) on medial to occluded ring it is direct inguinal hernia.
Q.189. A 35-year-old woman presents with a swelling in the neck. The swelling has increased in size gradually over the last two years and the patient feels she has difficulty with breathing. Examination: mass measures 8 cm by 10 cm, soft and not warm to touch. It moves with deglutition. Which is the most appropriate management of this mass?
Correct Answer : A
Gradually increased swelling in the neck which moves with deglutition is thyroid enlargement and as it is causing pressure symptoms like difficulty in breathing a partial thyroidectomy should be performed.
Q.190. A 46 year old laborer reports swelling in the right groin. The non-painful swelling is observable in both the erect and the recumbent positions. Examination: non-tender irreducible 4 cm mass in the right groin below and on the medial side of the inguinal ligament. Which is the most likely diagnosis in this patient?
Correct Answer : B
Sephanous vein varicocele is readily reducible with the recumbent position. So presented case is not sephanavarix.
The usual location of the femoral hernia is below and lateral to the pubic tubercle but it is not absolute and femoral hernia can present as a mass below and medial to the pubic tubercle. So the presented case is a case of femoral hernia.
Q.191. A 42 year old woman reports to the surgeon that she is worried about a lump that she feels the right breast. The surgeon observes a 2 cm by 3 cm mass in the right lower quadrant of the breast. There are no associated skin changes and the mass has limited mobility. There is no discharge from the nipple. There is no axillary lymph node enlargement. Examination of the left breast and axilla was completely normal. A mammogram report suggests the presence of microcalcifications. Which is the most appropriate next step in the management of this patient?
Correct Answer : B
A needle-guided biopsy of the breast.
Q.192. A 36 year old woman presents with swelling in the groin. Examination: swelling is diffuse and soft and lies below the inguinal ligament. It empties with minimal pressure and refills with release. There is a cough impulse and it disappears on lying down. On the calf of the same leg there are varicosities on the medial aspect. What is the most likely diagnosis?
Correct Answer : C
Below inguinal ligament, empties with minimal pressure and refills with a release, presence of cough impulse, and disappearance on lying down are suggestive of saphena varix supported by the presence of varicosity in the same leg.
Q.193. A man presents with a swelling above the groin crease in the abdomen. He has not had any med problems of note. What is the most probable dx?
Correct Answer : B
A Spigelian hernia (or lateral ventral hernia) is a hernia through the Spigelian fascia, which is the aponeurotic layer between the rectus abdominis muscle medially, and the semilunar line laterally.
Q.194. A 65 year old man had closure of colostomy performed 5 days ago. He is not systemically unwell. There is a tender, localised fluctuant swelling 4 cm in diameter in the wound. What is the most appropriate management?
Correct Answer : D
Local exploration of the wound.
Q.195. A 72 year old man being investigated for anaemia is booked for a colonoscopy in 24 hours. What is the most appropriate management the night before the procedure?
Correct Answer : D
Magnesium Citrate (Orally)
Q.196. A 60-year-old male is admitted with a 2 days history of lower abdominal pain and marked vomiting. On examination he has abdominal swelling, guarding and numerous audible bowel sounds. What is the likely diagnosis?
Correct Answer : D
History is not suggestive of ischemic colitis. There are no bowel sounds heard in the gallstone ileus.
Small bowel obstruction causes central abdominal pain, so given features with lower abdominal pain make it more likely to be sigmoid volvulus.
Q.197. A 23-year-old woman presents with a 1 cm small smooth, firm, mobile mass in her left breast. She is very anxious. What is the most appropriate investigation?
Correct Answer : B
This is fibroadenoma of the breast (breast mouse) for which the US of breast is the appropriate investigation and if it reveals a fibrous lump we shall go for FNAC.
Another point a doctor should know is that for any suspicious breast lesion, radiology should be done before options of biopsy and investigation of choice in radiology is a US scan before the age of 35 and mammography after the age of 35.
In that term also for this case, the investigation of choice is US breast.
Q.198. A 15-year-old girl presents with a 24 hours history of central abdominal pain, followed by the right iliac fossa pain, worse on coughing. She has fever and rebound in the right iliac fossa. What is the most appropriate diagnosis?
Correct Answer : A
Central abdominal pain radiating to the right iliac fossa is suggestive of acute appendicitis.
Pain worse on coughing, fever, and rebound tenderness in the right iliac fossa are well-known features of acute appendicitis.
Q.199. A 30-year-old old woman has severe colic and upper abdominal pain radiating to the right scapula and is vomiting. What is the most likely diagnosis?
Correct Answer : A
Biliary colic is characterized by the sudden onset of intense right upper abdominal pain that may radiate to the shoulder or right scapula. Sweating and vomiting are common. The pain tends to be steady and lasts up to three hours. Residual abdominal tenderness may occur.
Q.200. A 12-year-old girl has central abdominal pain and is vomiting. On examination her abdomen is found to be distended with no rebound and a tender lump in the right groin. What is the most likely diagnosis?
Correct Answer : B
Characteristics of strangulated hernias are as follows:
Patients have symptoms of an incarcerated hernia
Systemic toxicity secondary to ischemic bowel is possible
Strangulation is probable if pain and tenderness of an incarcerated hernia persist after reduction.
Q.201. A 31-yr-old woman has severe colic & upper abdominal pain. She is febrile &. vomiting. Hematological investigations show a moderate leukocytosis. What is the most likely diagnosis?
Correct Answer : D
Fever and leukocytosis favours the diagnosis of cholecystitis.
Q.202. A 31-yr-old woman presents with acute severe abdominal pain. Her blood pressure is 100/60 and no abdominal signs are found. Hemoglobin level is 17g/dl and the plasma amylase is only mildly raised. What is the most likely diagnosis?
Correct Answer : A
Mesenteric thrombosis.
Specific hypercoagulable states are identified in 60% to 75% of patients with mesenteric venous thrombosis. These include heparin-induced thrombocytopenia, essential thrombocythemia, post-splenectomy thrombocytosis, hyperviscosity as in polycythemia vera, and neoplastic disorders.
A mild rise in amylase rules out pancreatitis which is often associated with mesenteric thrombosis and high hemoglobin levels point towards polycythemia vera as the cause of mesenteric thrombosis here.
Q.203. A 30-year-old lady has developed breast abscess 2 days after delivery of her second baby. What is the most likely causative organism?
Correct Answer : D
Staphylococcus aureus
Q.204. A patient who was previously on 120 mg slow release oral morphine has had his dose increased to 200 mg. He is still in significant pain. He complains of drowsiness and constipation. What is the next step in the management?
Correct Answer : D
Replace morphine with oxycodone
Q.205. A 56-year-old patient whose pain was relieved by oral Morphine, now presents with progressively worsening pain relieved by increasing the dose of oral morphine. However, the patient complainsthat the increased morphine makes him drowsy and his is unable to carry out his daily activities.What is the next step in his management?
Correct Answer : A
Oral oxycodon
Q.206. A 50-year-old man has had anterior resection of the rectum for carcinoma. He expressed concerns about control of post-op pain in discussions with the anaesthetist before surgery. What is the best management strategy?
Correct Answer : C
IM morphine.
Some post-operative pain is severe pain which needs strong opioid analgesics.
Q.207. A man was operated for colorectal ca. His pain is relieved with morphine 60mg bd PO but now he can’t swallow medications. What will be the next regimen of analgesic administration?
Correct Answer : B
Fentanyl patch
Q.208. An 84-year-old man got surgical pain which is well controlled by oral morphine 60mg BD. However, now this pt is unable to swallow. What is the most appropriate next step?
Correct Answer : D
Fentanyl patches
Q.209. A 61-year-old man who had stroke 2 year ago is on aspirin. He has RA (rheumatoid arthritis) but suffers from pain and can’t tolerate it. He is taking senna for constipation. What is the best medicine to relieve his pain?
Correct Answer : D
Paracetamol.
DMARDs are not painkillers but prevent disease progression in the long term.
Co-codamol will cause constipation. The patient is already taking laxatives! So Cocodamol is not an option.
NSAIDs are avoided in one who is already taking aspirin.
Here paracetamol is the answer. Sometimes we undertreat patients when other options are risky to avoid more severe complications.
Q.210. A 48-year-old patient after surgical removal of mandibular carcinoma presents with perioral paresthesia and severe pain which is not relieved by oral morphine. What is the next step in treating this patient?
Correct Answer : D
Gabapentin.
This pain is likely due to nerve injury during operation and both amitryptiline and Gabapentine are 1st lines for neuropathic pain.
Q.211. A patient whose pain is not relieved by oral codeine. What is the best management?
Correct Answer : D
Oral morphine
Q.212. A patient was complaining of pain within 6 hours after his appendectomy for gangrenous appendix. What medicine is the best option for his pain relief?
Correct Answer : D
Tramadol
Q.213. A 65-year-old has terminal cancer and his pain is relieved by a fentanyl patch but he now complains of shooting pain in his arm. Which of the following will add to his pain relief?
Correct Answer : A
Gabapentin.
Shooting in the arm indicates neuropathic pain for which both amitryptiline and gabapentin can be used.
Q.214. Jean is a 72-year-old woman with recurrent bowel cancer following a hemi-colectomy 2 years ago. She is known to have both local recurrence and liver metastasis and her pain has been under control on MST 90mg bd. She has had quite severe pain in the RUQ for the past hour despite having taken her normal dose of MST. You find that she has an enlarged liver which is hard and irregular. There is marked localised tenderness over the right lobe of her liver. Her abdomen is otherwise soft and non-tender and the bowel sounds are normal. She is apyrexial. The treatment of choice would be?
Correct Answer : D
IM diamorphine
Choose a Question
×Choose a Question
×
Trial Access Limit Reached
You’ve reached the limit of free content. Subscribe to continue learning without restrictions.