

Hello,
Dr. Batman
Hello Doctor, Welcome!
Profile

Name: Batman
Email: batman@gotham.com
OBSTETRICS & GYNAECOLOGY
(Total Questions - 396)Q.1. A 53 year old woman has complaints of vaginal dryness, hot flushes and night sweats for the past 6 months. Her last menstrual period was more than a year ago. She currently takes an ACE inhibitor as part of her management for her blood pressure. What is the most appropriate management for her symptoms?
Correct Answer : C
Hormone replacement therapy like oestrogen and progestogen patches are indicated here as she is having menopausal symptoms. This systemic treatment can also alleviate symptoms of vaginal dryness.
A vaginal oestrogen cream or pessary would be appropriate if the patient only had symptoms of vaginal dryness without the other symptoms of menopause like hot flushes. In such cases, there is no need for a systemic treatment as topical treatment can alleviate symptoms.
Current evidence suggests that the use of HRT is not associated with an increase in blood pressure and therefore HRT is not contraindicated in women with hypertension as long as the blood pressure can be controlled by antihypertensive medication.
It is good practice to monitor the patient’s blood pressure 2 to 3 times in the first 6 months and then 6 monthly.
Current indications for the use of HRT are :
• Vasomotor symptoms such as flushing, including sleep, mood disturbance, and headaches.
• For women with early menopause, they should be treated with HRT until the age of natural menopause (around 51 years). The most important reason for HRT in this group is preventing the development of osteoporosis.
• For those women under 60 years who are at risk of an osteoporotic fracture in whom non-estrogen treatments are unsuitable it is especially important to note that other indications such as the reversal of vaginal atrophy should be treated with topical oestrogens.
Q.2. A 22 year old woman who was diagnosed with a missed miscarriage a week ago now presents to the hospital because of abdominal pain. She says she passed a small fetus and a number of clots this morning. On examination, abdomen is tender, and cervical os is opened. A transvaginal ultrasound scan shows products of conception still present in the uterus. What is the diagnosis?
Correct Answer : A
Products of conception still present in the uterus define incomplete miscarriage. Some products of conception have been expelled but some remain thus giving the diagnosis of incomplete miscarriage.
There is usually pain and vaginal bleeding and the cervical os is open.
A summary of types of miscarriages that are commonly asked in the exam :
Threatened miscarriage - Vaginal bleeding + fetal heart seen. The cervical os is closed.
Missed miscarriage (delayed miscarriage) - Dead fetus before 20 weeks without the symptoms of expulsion. May or may not have vaginal bleeding. The cervical os is closed.
Inevitable miscarriage- Cervical os opened and bleeding.
Incomplete miscarriage - Not all products of conception have been expelled
Complete miscarriage - Everything has been expelled.
Q.3. A 35 year old woman had a spontaneous vaginal delivery 10 days ago. She delivered a healthy baby girl and is currently breastfeeding. There were no complications throughout labour and the midwife has documented that the placenta appears complete. She now presents with irregular dark red vaginal bleeding over the past 2 days. Her blood pressure is 130/75 mmHg, pulse rate is 85 beats/minute and respiratory rate is 18 breaths/minute. She has a temperature of 37.4 C. What is the next most appropriate action?
Correct Answer : D
Secondary PPH is characterized by abnormal or excessive bleeding from the birth canal between 24 hours and 12 weeks postnatally. It is most commonly caused by endometritis.
Investigations should include :
• High vaginal swab
• Blood including FBC and CRP
• Consider a transvaginal ultrasound to assess for retained products if there is no improvement.
Co-amoxiclav is the first-line antibiotic for endometritis. It is safe for breastfeeding.
Q.4. A 33 year old woman complains of waking in the middle of the night to rush to the toilet. Most of the time, she does not make it to the toilet on time and she wets herself. What is the diagnosis?
Correct Answer : B
This is the common presentation of urge incontinence.
Types of urinary incontinence:
Urge incontinence / overactive bladder (OAB) is due to detrusor overactivity. A common complaint is “When I have to go to the toilet, I really have to go” or “I have the desire to pass urine, and sometimes urine leaks before I have time to get to the toilet”.
Stress incontinence leaks small amounts of urine when coughing or laughing. Usually with a history of many vaginal deliveries as this would weaken the pelvic floor muscles.
Mixed incontinence: Mix of both urge and stress incontinence.
Overflow incontinence: Involuntary release of urine from an overfull urinary bladder, often in the absence of any urge to urinate. It occurs in people who have a blockage of the bladder outlet (benign prostatic hyperplasia, prostate cancer, or narrowing of the urethra), or when the muscle that expels urine from the bladder is too weak to empty the bladder normally.
Urethrovaginal fistula : Opening between vagina and urethra. A common complaint is “There is continual leakage of urine from my vagina” or “My vagina has a foul smell”.
MANAGEMENT OF URINARY INCONTINENCE:
The management of incontinence depends on whether urge or stress urinary incontinence is predominant.
For stress incontinence:
1. Pelvic floor exercise is the initial treatment of choice. NICE recommends that at least eight contractions be performed three times a day for a minimum of three months.
2. Surgical procedures e.g., retropubic mid-urethral tape procedures may be required.
3. Duloxetine is used for those who are not surgical candidates.
For urge incontinence :
1. Bladder retraining (minimum of six weeks). The idea is to increase the intervals between voiding gradually
2. Bladder stabilizing drugs: antimuscarinic agents are first-line. NICE recommends oxybutynin, tolterodine, or darifenacin. Immediate release oxybutynin should however, be avoided in frail older women.
Q.5. A 16 year old clinically obese girl has not started her menstrual periods yet. She has severe acne and facial hair growth. Among her investigations, a high level of insulin was found. What is the likely diagnosis?
Correct Answer : C
Polycystic ovary syndrome (PCOS) would fit the best among the answers.
Cushing’s would be a consideration here as it can sometimes cause amenorrhoea too.
POLYCYSTIC OVARIAN SYNDROME (PCOS) is a complex endocrine disorder with clinical features that include hirsutism and acne (due to excess androgens), oligomenorrhoea or amenorrhoea, and multiple cysts in the ovary.
Symptoms:
• Oligomenorrhoea or amenorrhoea
• Hirsutism
• Alopecia
• Obesity
• Acne
• Subfertility
Diagnosis :
Rotterdam consensus criteria : Two out of three of the following criteria are diagnostic of the condition.
1. Ultrasound polycystic ovaries (either 12 or more follicles or increased ovarian volume)
2. Oligo-ovulation or anovulation
3. Clinical and/or biochemical signs of hyperandrogenism. Around 20% of women have an appearance suggestive of polycystic ovaries on ultrasound but unless they fulfill the criteria of PCOS, they should not be treated.
Biochemical abnormalities :
• Hyperadrenogenism. Biochemical hyperandrogenism is considered an elevated free androgen index (FAI) of more than 5.
• Hyperinsulinemia
• Increase in serum LH
General management - Weight loss
Management of menstrual irregularities -
• Weight loss
• Combined oral contraceptive pills, cyclical progestogen, or levonorgestrel intrauterine system.
Management of infertility :
• Weight loss alone may achieve spontaneous ovulation
• Clomifene Citrate
• If clomifene citrate fails, add on metformin or gonadotrophins or Laparoscopic ovarian drilling.
Note regarding metformin:
• The RCOG published an opinion paper and concluded that on current evidence metformin is not a first-line treatment of choice in the management of PCOS.
• Metformin is however still used, either combined with clomifene or alone, particularly in patients who are obese.
• The rationale behind metformin use is that it improves insulin sensitivity and reduces hyperinsulinemia.
Q.6. A 35 year old lady presents with urinary incontinence 4 months after having a normal vaginal delivery of her second child. She says that she urinates a little every time she sneezes or coughs. On a speculum examintion, there are no anatomical abnormalities. What is the most approprite next step in management?
Correct Answer : C
This lady is suffering from stress incontinence as evidenced by small amounts of urine leakage when she sneezes or coughs.
The best management would be pelvic floor exercises.
.Tension-free vaginal tape operation should only be considered after trying conservative methods for the treatment of stress incontinence.
Bladder drill (retraining) is a method used for detrusor instability and not stress incontinence. Ring pessary is of no use here as there is no cystocele.
Loss of weight, and reducing caffeine are other lifestyle modifications that could be effective but were not given in this question.
Q.7. A 27 year old woman presents to the emergency department in a presenting complaint of lower abdominal pain. The pain started suddenly earlier in the day. She is sexually active and does not use barrier methods. She has abdominal tenderness, temperature of 39.0 C, heart rate of 102 bpm, and a blood pressure of 130/85 mmHg. There is no vaginal discharge seen on speculum examination. What is the most appropriate next course of action to make the diagnosis?
Correct Answer : A
A tubo-ovarian abscess is an advanced complication of acute salpingitis, known clinically as pelvic inflammatory disease.
Ultrasonography should be done in very ill patients in whom tubo-ovarian abscess is suspected. A high vaginal swab or endocervical swab can take days to return with results.
As this is an A&E case, an ultrasound would be more appropriate as this would lead to a diagnosis.
Q.8. A 33 year old woman has just had an uncomplicated normal vaginal delivery. The third stage of labour was managed actively and the placenta and membranes were expelled completely soon after delivery of the baby however she continues to bleed vaginally. She has now total estimated blood loss of 1 litre. Her uterus is relaxed and is felt to be boggy and above the umbilicus. What is the most appropriate immediate step to manage this patient?
Correct Answer : C
Causes for PPH may be considered to relate to one or more of ‘the four Ts’:
• Tone (abnormalities of uterine conception)
• Tissue (retained products of conception)
• Trauma (of the genital tract)
• Thrombin (abnormalities of coagulation)
The most common cause of primary PPH is uterine atony and in this case, since the uterus is felt to be above the uterus and relaxed, a uterine massage would be the most appropriate next step.
Q.9. A 33 year old woman who is rhesus negative had just delivered vaginally 3 hours ago. She would like to know when is the best time for anti-D immunoglobulins to be administered. What is the recommended time to administer anti-D immunoglobulins to a previously non-sensitised rhesus negative mother after delivery?
Correct Answer : B
Following potentially sensitizing events which include giving birth, anti-D immunoglobulins should be administered as soon as possible and always within 72 hours of the sensitizing event.
.If exceptionally this deadline has not been met and 72 hours have passed, you can still administer anti-D immunoglobulins for up to 10 days as there may still be some protection offered during this time.
RHESUS NEGATIVE PREGNANCY :
A basic understanding of the pathophysiology is essential to understand Rhesus-negative pregnancies. If a Rh -ve mother delivers a Rh +ve child a leak of fetal red blood cells may occur which causes anti-D IgG antibodies to form in the mother. In future pregnancies, these antibodies can cross the placenta and cause haemolysis in the fetus.
Prevention of Rh sensitization-
• Test for anti-D antibodies in all Rh -ve mothers at booking.
• If Rh –ve and not previously sensitised, guidelines (2008) advises giving anti-D at 28 and 34 weeks gestation.
• Anti-D is for prophylaxis only–Remember once sensitization has occurred it is irreversible and Anti-D administration would be pointless Anti-rhesus (anti-D) immunoglobulin is given intramuscularly. It neutralizes any Rhesus D-positive antigens that have entered the mother’s blood. If the antigens have been neutralized, there will be no reason for a mother to develop immunity and produce antibodies. She would remain non-sensitised.
Anti-D immunoglobulin should be given as soon as possible (but always within 72hours) in the following situations:
• Delivery of a Rh +ve infant, whether live or stillborn.
• Any termination of pregnancy or evacuation of retained products of conception (ERPC) after miscarriage.
• Miscarriage if gestation is > 12 weeks.
• Ectopic pregnancy.
• Blunt abdominal trauma.
• External cephalic version.
• Antepartum haemorrhage, any vaginal bleeding over 12 weeks gestation.
• Amniocentesis, chorionic villus sampling, fetal blood sampling.
Affected fetus : If unborn - Oedematous (Hydrops fetalis, as liver devoted to RBC production thus albumin falls), Foetal heart failure.
Treatment involves intrauterine blood transfusion :
• If born - Jaundice (due to build-up of excessive bilirubin from RBC breakdown), Anaemia, Hepatosplenomegaly.
• Treatment involves UV phototherapy, blood transfusion, and exchange transfusion.
Q.10. A 45 year old lady comes to the family planning clinic for contraception advice. She has two young children and does not want anymore children. An incidental finding of multiple small submucosal fibroids was found recently on an ultrasound scan. She is asymptomatic and her medical history is otherwise insignificant. What is most appropriate contraceptive for this lady?
Correct Answer : D
Combined hormonal contraception (CHC): Despite the 'pill' previously being considered a risk factor for fibroid growth, CHC is helpful if the patient requires contraception, although it is not as effective as a levonorgestrel-releasing intrauterine system.
Thus, the intrauterine system would be the answer here.
The intrauterine system (IUS) reduces the uterine size in women with fibroids. If this lady here had presented with asymptomatic fibroids and was not looking for contraception, expectant management would be a valid answer especially if she was peri-menopausal.
CONTRACEPTION CLINCHERS : Choosing the correct contraceptive for the correct situation is something a lot of doctors have problems with. Here are some useful contraception/abnormal uterine bleeding clinchers for the exam.
Young woman, not sexually active (don’t require contraception)
• Menorrhagia only – Tranexamic acid
• Menorrhagia with dysmenorrhoea – Mefenamic acid
• Menorrhagia / dysmenorrhoea/metrorrhagia (irregular menses) - COCP Sexually active woman (require contraception).
• Menorrhagia / dysmenorrhoea or those suffering from fibroids (which do not distort the uterine cavity) – IUS Mirena (first-line).
These questions will also mention possible contraindications for COCP like obesity/smoking/history of thromboembolism etc.
• Women with sickle cell disease and menorrhagia – Depo-provera IM
Emergency contraception • Within 72 hours of unprotected sex
• Within 120 hours of unprotected sex – IUCD
FIBROID MANAGEMENT-
If Asymptomatic
• Follow up annually to monitor size and growth unless rapid growth or reason to suspect pelvic malignancy in which case further investigations are warranted with menorrhagia.
• Levonorgestrel-releasing intrauterine system (LNG-IUS) – provided uterine fibroid is not distorting the uterine cavity.
• Tranexamic acid, NSAIDs or COCP
• Norethisterone as a temporary measure With severe menorrhagia and fibroid more than 3 cm • Ulipristal acetate up to 4 courses. Each course is up to 3 months. Usually used in pre-operative treatment.
Surgical management-
• Hysterectomy – The most successful treatment
• Myomectomy
• Uterine artery embolization
• Endometrial ablation – only for fibroids less than 3 cm in diameter.
Both myomectomy and uterine artery embolization can be performed in patients who would like to preserve their fertility with myomectomy usually being the preferred option in these cases especially if treatment of infertility is required. Myomectomy has been shown to increase pregnancy rates compared with uterine artery embolization.
Other medical management :
• Gonadotropin-releasing hormone (GnRH) agonists. Reduces the size of fibroids and is used before surgery to reduce perioperative blood loss. Surgery must take place as uterine fibroids would return to pretreatment size if GnRH agonist treatment is stopped.
Q.11. A 40 year old woman attends the Gynaecology outpatient clinic for painful periods. The pain is worse on the first day of her menstrual cycles and continues for 5 days. She has regular 28 day cycles. She also suffers from menorrhagia. She has had a laparoscopic tubal sterilisation in the past. She takes ibuprofen and paracetamol for pain relief during the first few days of pelvic pain. She is currently sexually active with her stable partner of 10 years. She has no bowel or urinary symptoms. Endometriosis is suspected. What is the most appropriate action?
Correct Answer : A
The key to answering this is knowing when a diagnostic laparoscopy is required for endometriosis. In practice, we would offer a trial of hormonal treatment for a period of 3 to 6 months before having a diagnostic laparoscopy. This is due to the risk of laparoscopic surgery with the additional fact that even with a laparoscopic ablation of endometrial tissue the relapse of symptoms occurs in 40 to 45% of women with up to 30% of women being readmitted for surgery within 5 years.
ENDOMETRIOSIS :
Endometriosis is the presence of endometrial-like tissue outside the uterine cavity. It is oestrogen dependent, and therefore mostly affects women during their reproductive years. If the ectopic endometrial tissue is within the myometrium itself it is called adenomyosis. Up to 10-12% of women have a degree of endometriosis.
Clinical features :
- Chronic pelvic pain (cyclic or constant)
- Dysmenorrhoea - pain often starts days before bleeding
- Deep dyspareunia (indicates possible involvement of uterosacral ligaments)
- Subfertility
INVESTIGATIONS :
- Laparoscopy is the gold-standard investigation
- Transvaginal ultrasound scanning appears to be a useful test, both to make and exclude the diagnosis of an ovarian endometrioma.
Management :
- NSAIDs to treat pain
- Combined oral contraceptive pill (other hormonal drugs can be used too)
- Levonorgestrel intrauterine system
Note: Drug therapy unfortunately does not seem to have a significant impact on fertility rates. Laparoscopic excision and ablation of endometrioid lesions help reduce endometriosis-associated pain. Laparoscopic excision and ablation of endometriotic ovarian cysts may improve fertility.
Q.12. A 27 year old woman has pelvic pain, dysmenorrhoea and increasingly heavy periods over the last 12 months. She also complains of dyspareunia. There is generalized pelvic tenderness without peritonism. A pelvic ultrasound was requested and was reported with no evidence of adenomyosis or ovarian endometrioma. What is the most likely diagnosis?
Correct Answer : C
There are two possibilities here. Endometriosis and pelvic congestion syndrome. Given that endometriosis is much more common than pelvic congestion syndrome, endometriosis is the answer.
A take-home point here is a normal ultrasound pelvis does not exclude endometriosis.
Endometriosis presents exactly the way they describe this question with chronic pelvic pain, dysmenorrhoea, and dyspareunia.
Pelvic ultrasound scans are usually normal. In pelvic venous congestion, there are dilated veins believed to cause a cyclical dragging pain. It is worse premenstrually and after prolonged periods of standing and walking.
Dyspareunia is also often present. Given there is no history of standing here, pick endometriosis. It is also by far more a common diagnosis when it comes to chronic pelvic pain.
Q.13. A 36 year old woman is planning to undergo a laparoscopic tubal sterilisation. What is the risk of pregnancy after sterilisation by tubal ligation?
Correct Answer : B
Laparoscopic tubal occlusion using Filshie clips to mechanically occlude the fallopian tubes is now the laparoscopic method of choice.
The risk of pregnancy after sterilization by tubal ligation is about 1:200, meaning that 1 in every 200 women who undergo sterilization may get pregnant at some point after sterilization.
Q.14. A 22 year old woman was prescribed doxycycline for 10 days to treat Lyme disease. She has been using combined oral contraceptive pills regularly for the past 6 months. What is the most appropriate advice?
Correct Answer : B
No action is needed. The latest recommendations are that no additional contraceptive precautions are required when combined oral contraceptives are used with anti bacterials that do not induce liver enzymes unless diarrhoea or vomiting occurs.
ORAL CONTRACEPTION INTERACTION AND HEPATIC ENZYME INDUCERS : Hepatic enzyme inducers can decrease the effectiveness of the combined oral contraceptive pill and progesterone-only pill when taken at normal doses.
The two most commonly used oral contraception interactions with hepatic enzyme inducers are:
1. Rifampicin
2. Anticonvulsants (such as phenytoin, carbamazepine, phenobarbitone) : Women starting enzyme-inducing drugs should be advised to use a reliable contraceptive method that is unaffected by enzyme inducers. In general, depo-provera, copper intrauterine devices or the levonorgestrel containing intrauterine system (LNG-IUS) are the safest to use.
A good GP would discuss the use of additional barrier methods, having progesterone-only injections, insertion of intrauterine devices, or use of an increasing dose of oestrogen.
Q.15. A 24 year old woman with multiple sexual partners complains of non-cyclical intermittent lower abdominal pain, deep dyspareunia and menstrual irregularities that has been ongoing for 18 months. On vaginal examination, cervical excitation was noted and she is tender on both adnexae. She has no significant past medical history. Which is the most likely cause of her symptoms?
Correct Answer : C
Multiple sexual partners are a risk factor for Pelvic inflammatory disease. Women of her age group (<25 years old) are at greater risk for pelvic inflammatory disease as they are more sexually active during this period.
Other options are less likely because:
Although chronic pelvic pain, deep dyspareunia, and menstrual irregularities could be seen in endometriosis, it is unlikely the given choice here as the history of multiple sexual partners and cervical excitation does not match this answer. This pain is non cyclical which also suggests PID rather than endometriosis.
Fitz-Hugh-Curtis syndrome is a complication of pelvic inflammatory disease (PID). Usually presents with an acute onset of the right upper quadrant (RUQ) abdominal pain aggravated by breathing, or coughing. This pain may be referred to the right shoulder.
Cervicitis usually presents with discharge.
Do not get confused between cervicitis and PID. Infection at the cervix can eventually ascend to cause PID. But if the infection is purely at the cervix, they will not present with menstrual irregularities and lower abdominal pain as the infection has not ascended to involve the uterus, fallopian tubes, and ovaries.
Asherman syndrome are adhesions of the endometrium often associated with dilation and curettage of the intrauterine cavity. It results in infertility. Often, they experience menstrual irregularities. But in this question, there is no relevant past medical history meaning she did not have any dilation and curettage thus this option is very unlikely.
PELVIC INFLAMMATORY DISEASE :
Pelvic inflammatory disease (PID) is a term used to describe infection and inflammation of the female pelvic organs including the uterus, fallopian tubes, ovaries, and the surrounding peritoneum.
Most commonly caused by ascending infection from the endocervix.
Causative organisms :
• Chlamydia trachomatis - The most common cause
• Neisseria gonorrhoeae
Risk factors for PID :
• Age <25
• Previous STIs
• New sexual partner / multiple sexual partners
• Uterine instrumentation such as surgical termination of pregnancy
• Intrauterine contraceptive devices
• Post-partum endometritis
Features :
• Lower abdominal pain
• Fever
• Deep dyspareunia
• Dysuria and menstrual irregularities may occur
• Vaginal or cervical discharge
• Cervical excitation
• Abnormal vaginal bleeding (intermenstrual, postcoital)
Investigation :
• Screen for Chlamydia and Gonorrhoea
Management :
There are many combinations of antibiotics to treat PID. This is one of the combination examples for the treatment of PID.
Outpatients: Ceftriaxone 500 mg as a single intramuscular dose, followed by oral doxycycline 100 mg twice daily plus oral metronidazole 400 mg twice daily, both for 14 days.
Note the differences between acute PID and just cervicitis.
If just cervicitis (Chlamydia)
• Azithromycin 1g single dose (OR doxycycline 100mg bd for 7 days); both have similar efficacy of more than 95%.
If just cervicitis (Neisseria gonorrhoeae)
• Azithromycin 1g PO and ceftriaxone 500mg IM.
RCOG guidelines suggest that in mild cases of PID intrauterine contraceptive devices may be left in.
Complications :
• Infertility - the risk may be as high as 10-20% after a single episode
• Chronic pelvic pain
• Ectopic pregnancy
Q.16. A 34 year old female presents with a very strong foul smelling vaginal discharge. What organisms could cause such a symptom?
Correct Answer : D
Bacterial vaginosis and Trichomonas vaginalis can give foul-smelling discharge.
In bacterial vaginosis, the vaginal discharge is grey-white and has a “fishy” smell.
In trichomonas vaginalis, it can be greenish and frothy along with vulvovaginitis i.e. strawberry cervix.
The discharge of Chlamydia and Gonorrhea is not usually foul-smelling.
Since Trichomoniasis is not present among the available choices, Gardnerella is the answer.
Bacterial vaginosis (BV) is caused by an overgrowth of mixed anaerobes, such as Gardnerella vaginalis, which replace the usually dominant vaginal lactobacilli resulting in a raised vaginal pH. It is the commonest cause of abnormal vaginal discharge in women of childbearing age. Whilst BV is not a sexually transmitted infection it is seen almost exclusively in sexually active women.
Features :
• Vaginal discharge: 'fishy', offensive
• Asymptomatic in 50%
• Homogenous grey-white discharge
• Characteristic fishy smell
• ‘Clue cells’ present on microscopy
• Vaginal pH > 5.5
Management- May resolve spontaneously and if successfully treated has a high recurrence rate.
However, most women prefer it to be treated.
• Metronidazole 400mg orally bd for 5 days or metronidazole 2g (single dose) OR
• Clindamycin 2% cream vaginally at night for 7 days.
Q.17. A 64 year old woman has been treated for breast cancer with tamoxifen. What medication should be added to her regime?
Correct Answer : A
No guideline says any of the above medications should be started as an adjuvant to her regime. However, given the choices provided, bisphosphonates are probably the best choice as it is shown in some studies to reduce the risk of bone metastasis in breast cancers.
Q.18. A 34 year old woman who is 26 weeks pregnat attends her general practice with complaint of constipation. She has already tried conservative managements like increased water intake and is on high fibre foods. She is also active and exercises 3 times a week. What is the most appropriate medication to administer?
Correct Answer : C
Constipation can be improved by increasing fluid intake, eating high-fiber foods, and exercising, all of which this patient has already done. When conservative management has been attempted and is unsuccessful, laxatives should be tried.
Lactulose, which is not known to be harmful in pregnancy is usually used as first-line for pregnant women as it is a very well-tolerated medication.
Senna which is a stimulant laxative is also very effective however they do cause more abdominal discomfort compared to bulk-forming laxatives like lactulose.
If senna is used, it should only be used for short periods.
Q.19. A 32 year old woman presents to the clinic with a 11 week history of amenorrhoea. A home pregnancy test done that morning was shown to be positive. Today, she is complaining of painless vaginal bleeding. She has excessive morning sickness for the past 2 weeks. She has had two previous normal vaginal deliveries. Routine examination of the patient’s abdomen reveals a gravid uterus which extends to slightly past the umbilicus. The fundal height measures around 16 cm. On speculum examination, the cervical os is seen as closed. What is the most likely diagnosis?
Correct Answer : D
Not all questions are straightforward in exams. You will come across somewhere you feel the information is missing like this one. The options of incorrect dates and molar pregnancy come close. It is important to that that the question states the uterus extends up to 16 weeks gestation.
It can therefore be inferred that the pregnancy is either large for dates with a uterine fibroid or molar pregnancy alternatively an incorrect menstrual period date is also a possibility.
If this patient had uterine fibroids, it would NOT explain the excessive morning sickness. If this patient had an incorrect menstrual period date and was 16 weeks gestation, it would NOT explain the reason hyperemesis started so late in pregnancy. Symptoms of hyperemesis would have occurred several weeks ago as hyperemesis symptoms begin 6 to 8 weeks and peak at 12 weeks. The patient is presenting with features of molar pregnancy which are uterus large for dates, first trimester bleeding, and hyperemesis.
This is a presentation that is also similar to multiple pregnancies like twin pregnancies as they are also at increased risk of bleeding, hyperemesis, and have a uterus that is larger for dates. However, in multiple pregnancies, the uterus is seen to be larger in the second trimester rather than the first. Also, multiple pregnancies are not an option given here. Hyperemesis gravidarum is not completely incorrect as this patient also has a diagnosis of hyperemesis gravidarum as she has been seen to be vomiting for the past two weeks. However, the most likely diagnosis given the whole clinical picture is still molar pregnancy.
Gestational trophoblastic disease (GTD) covers a spectrum of diseases caused by overgrowth of the placenta.
It ranges from molar pregnancies to malignant conditions such as choriocarcinoma.
If there is any evidence of persistence of GTD the condition is referred to as gestational trophoblastic neoplasia (GTN).
Features:
• Hyperemesis due to excessive amounts of human chorionic gonadotropin (hCG)
• Irregular first-trimester vaginal bleeding
• Uterus large for dates
• Vaginal passage of vesicles containing products of conception
• Serum hCG is excessively high with complete moles, but levels may be within the normal range for partial moles.
Ultrasound findings of a complete mole : ‘Snowstorm’ appearance of mixed echogenicity, representing hydropic villi and intrauterine haemorrhage , Large theca lutein cysts.
Management of Hydatidiform mole:
• Surgical evacuation (Suction curettage)
Note that histological examination of products of conception is essential to confirm the diagnosis.
• Two-weekly serum and urine samples until hCG concentrations are normal. Women should be advised not to conceive until their hCG level has been normal for 6 months. Barrier contraception should be used until serum hCG is normal (oral contraception may also be used after molar evacuation before hCG returns to normal)
Management of gestational trophoblastic neoplasia (GTN) : This is unlikely to be asked in detail in EXAM due to the complexity of management. But you do need to know it involves chemotherapy. If chemotherapy is started, women should wait a year from the completion of their treatment before trying to conceive.
Q.20. A pregnant woman with long term history of osteoarthritis comes to the antenatal clinic with complaints of restricted joint movement and severe pain in her affected joints. What is the most appropriate management?
Correct Answer : C
It is important to remember that you should never prescribe any pain-relief other than paracetamol to a pregnant woman. Paracetamol has a good safety profile with pregnant women when compared to all the other analgesics.
There are cases where stronger pain relief is needed, but usually, consultants would be involved in the management.
For EXAM, whenever you see a pregnant lady with any sort of pain(whether it is from osteoarthritis, back pain, headaches, or a sprained ankle), never give any analgesia except for paracetamol.
Q.21. A 50 year old lady presents with complaints of urinary incontinence which occurs daily. She says that she urinates a little everytime she laughs or coughs. She has had 2 previous vaginal deliveries. She has been avoiding going out and has reduced her outdoor activities due to her urinary incontinence. On physical examination, the patient is found to have vaginal atrophy and a well supported uterus. A urinalysis was done and the results were found to be insignificant. What is the most appropriate initial step in her management?
Correct Answer : A
This is a typical case of stress incontinence. To understand it further, first, we need to understand what urinary incontinence is. Incontinence is the involuntary leakage of urine.
Stress incontinence is a leak of small amounts of urine when coughing or laughing. This is due to an increase in intra-abdominal pressure. Usually with a history of many vaginal deliveries as this would weaken the pelvic floor muscles.
The next management here would be pelvic floor exercises. Loss of weight and reducing caffeine are other lifestyle modifications that could be effective but were not given in this question.
Q.22. A 24 year old lady presents to the Early Pregnancy Unit with vaginal spotting and mild left-sided abdominal pain. Her last menstrual period was 8 weeks ago. A pregnancy test done in the GP clinic was positive. She has a transvaginal ultrasound scan, which is reported as ‘inconclusive’. Serum human chorionic gonadotropin (hCG) is 1400 IU/litre. What is the most likely diagnosis?
Correct Answer : C
The diagnosis here is ectopic pregnancy. The first clue here is the gestational age 8 weeks. Ectopic pregnancies would usually present around 6-8 weeks from the start of the last period as it is then that they are large enough to stretch the fallopian tubes thus causing pain.
The stretching of the fallopian tubes is also the reason why they may sometimes experience cervical motion tenderness on a vaginal examination. The second clue here is the unilateral abdominal pain.
This gives us a clue that the pathology is towards one side rather than in the middle. The remaining choices are far less likely to be the correct answer.
In the past, fibroids could be the cause of an inconclusive scan as they may obstruct the view of the gestational sac.
However, with the modern transvaginal scan, this is no longer the case. And thus ectopic pregnancies are a more likely diagnosis here.
Complete miscarriage - This is when all products of conception have been expelled. This is unlikely the case as she has only suffered mild vaginal bleeding (vaginal spotting).
Threatened miscarriage - Presents with vaginal bleeding + fetal heart is seen. A diagnosis of threatened miscarriage cannot be made without seeing a viable fetus on an ultrasound scan.
Incomplete miscarriage - Not all products of conception have been expelled. This means that products of conception would still be visible on an ultrasound scan.
ECTOPIC PREGNANCY: Defined by the implantation of a fertilized ovum outside the uterus.
Clinical features :
• Lower abdominal pain: typically the first symptom.
• Vaginal bleeding: usually less than a normal period.
• History of recent amenorrhoea: typically 6-8 weeks from the start of the last period.
• Peritoneal bleeding can cause shoulder tip pain.
Any woman of childbearing age who attends A&E with abdominal pain MUST have a urine pregnancy test performed. Ruptured ectopic pregnancies are life-threatening. Do not miss a diagnosis of an ectopic by forgetting to do a urine pregnancy test.
Examination findings :
• Abdominal tenderness
• Cervical excitation (also known as cervical motion tenderness)
• Adnexal mass may be noticed – rarely seen.
Always observe the blood pressure of the patient as a significant drop of blood pressure in a suspected ectopic needs to be quickly escalated.
Management:
• If haemodynamically stable - Laparoscopic salpingectomy or salpingostomy
• If haemodynamically unstable- Laparotomy (open salpingectomy or salpingostomy)
METHOTREXATE would be the first line for an ectopic pregnancy, if the patient was not in significant pain however it can only be used if it contains all the criteria below
• Not in significant pain
• Haemodynamically stable
• Adnexal mass smaller than 35 mm with no fetal heart visible
• No intrauterine pregnancy
• Serum hCG less than 5000 IU/liter (ideally less than 1500 IU/liter)
• Able to return for follow-up.
Q.23. A 31 year old woman who is currently 39 weeks gestation attends the antenatal day unit feeling very unwell with sudden onset of epigastric pain associated with nausea and vomiting. She has a temperature of 36.7 C and her blood pressure is 155/100 mmHg. Her liver enzymes are raised and her other blood results are as follows: Haemoglobin 82 g/L White cell count 5 x 109/L Platelets 90 x 109/L. What is the most likely diagnosis?
Correct Answer : B
HELLP syndrome : This is a serious complication regarded by most as a variant of severe pre-eclampsia which manifests with haemolysis (H), elevated liver enzymes (EL), and low platelets(LP).
Liver enzymes usually increase and platelets decrease before haemolysis occurs. The syndrome is usually self-limiting, but permanent liver or renal damage may occur. Note that eclampsia may co-exist.
Signs and Symptoms:
• Epigastric or RUQ pain and tenderness
• Nausea and vomiting
• Urine is ‘tea-colored’ due to hemolysis.
• Increased BP and other features of pre-eclampsia
Management :
• Delivery
• Supportive and as for eclampsia (magnesium sulfate (MgSO 4 ) is indicated)
• Although platelet levels may be very low, platelet infusions are only required if bleeding, or for surgery and <40
DIFFERENTIATING AFLP FROM HELLP - Acute fatty liver of pregnancy vs Haemolysis, Elevated Liver enzymes, Low Platelets syndrome. It is unlikely that you would need to know all the different features of HELLP and AFLP for the level of the exam as even senior medical and obstetric teams often have difficulty telling them apart in a clinical setting, however, this table is inserted for those who would like to understand how to differentiate them for your clinical knowledge.
Q.24. A 20 year old primiparous woman, 32 weeks gestation, presents to the maternity assessment unit with a history of painless vaginal bleeding after intercourse. She is not booked at your current hospital, but came to the closest hospital for assessment. She states that there have been no problems during her pregnancy and that she has been seeing her midwife in the community. On examination, a soft and relaxed uterus is noteed with a fundal height of 32 cm. CTG is normal. She has a pulse of 112 beats/minute, a blood pressure of 94/60 mmHg and a respiratory rate of 26 breaths/minute. What is the most likely diagnosis?
Correct Answer : C
Painless vaginal bleeding without abdominal pain should raise suspicion of placenta praevia.In many countries, it is common to have an ultrasound scan during the first trimester and again around 20 weeks for an anomaly scan in which the sonographer would formally report the position of the placenta.
In this case, she did not have previous scans so she may very well have a low-lying placenta. The painless bleeding seen in the placenta praevia may occur without warning or after intercourse. This is one reason obstetricians advise women with placenta praevia not to have intercourse.
From her observations, one can see that it is maternal blood that is being lost which is consistent with placenta praevia. If this was the case of vasa praevia, it would be fetal blood that would be lost and maternal observations would remain normal.
Placental abruption presents with sudden onset abdominal pain +/- vaginal bleeding. It is also commonly associated with CTG abnormalities.
Placenta accreta is less common than placenta praevia and is seen commonly in the presence of a uterine scar which allows the placenta to attach to the myometrium.
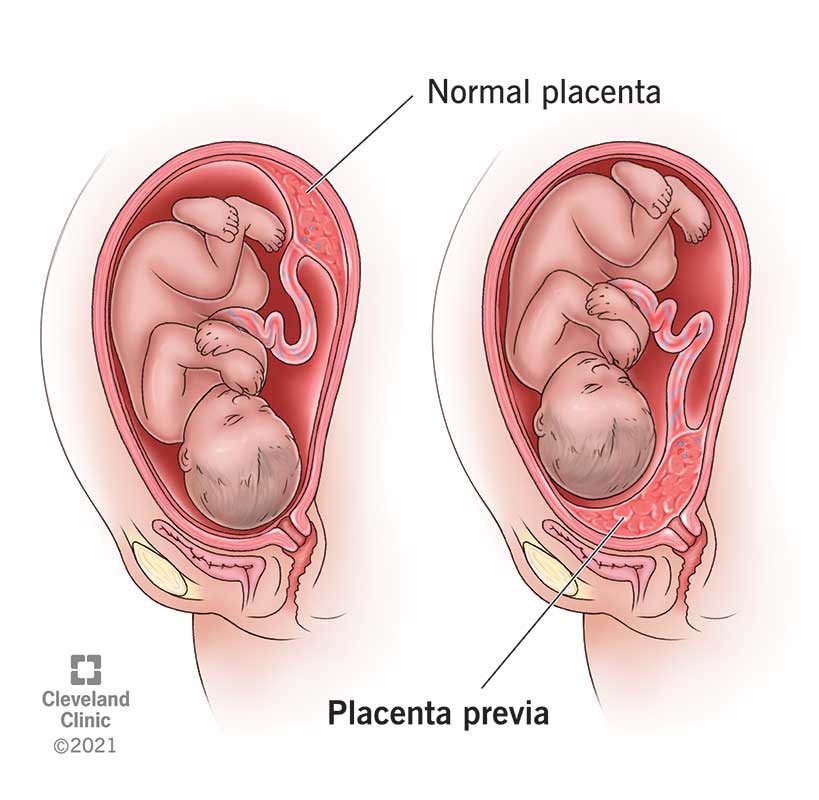
PLACENTA PRAEVIA:
Placenta praevia describes a placenta lying wholly or partly in the lower uterine segment. This is common early in the pregnancy but is most often not associated with bleeding. The key clinical feature is painless bleeding after 24 weeks of gestation.
Risk factors :
• Previous placenta praevia
• Multiple pregnancies
Symptoms :
- Vaginal bleed
- Uterus not tender
- Lie and presentation may be abnormal
- Fetal heart is usually normal. The painless late-pregnancy bleeding may occur during rest or activity, suddenly and without warning. It may be preceded by trauma, coitus, or pelvic examination. A digital vaginal examination should NOT be performed. However, a speculum or a transvaginal probe can safely be used in placenta praevia.
Diagnosis- This is based on the presence of painless late-trimester vaginal bleeding with an obstetric ultrasound showing placental implantation over the lower uterine segment. A transvaginal ultrasound is preferred over abdominal ultrasound for the detection of placenta praevia.
Q.25. A 35 year old woman presented with the complaint of lower abdominal pain to the gynaecology outpatient clinic. She had been experiencing mild abdominal pain since the insertion of an intrauterine contraceptive device (IUCD) two months ago. Her last menstrual period was seven days ago. On speculum examination, the IUCD strings were not visualized. The patient says that she is in a long term sexual relationship with her boyfriend of three years. The patient was subsequently referred fro a transvaginal ultrasound whereupon the IUCD was not found in the uterus. What is the most appropriate next step in this case?

Correct Answer : A
To answer this question accurately, it is essential to know about the management of lost intrauterine device threads.How do we manage lost intrauterine device threads
1. Exclude pregnancy by performing a urine pregnancy test.
2. Request a pelvic ultrasound to look for the IUCD
3. If the IUCD is not found on ultrasound, request an abdominal X-ray
Emergency contraception is incorrect as there is no evidence of recent sexual intercourse in the stem. Remember, one needs to know the timing of sexual intercourse to know which emergency contraception to use.
For example, levonorgestrel can be used for up to 72 hours whereas ulipristal acetate and copper intrauterine device can be used for up to 5 days. We are not sure if the coil is in place. There is no evidence of sexual intercourse.
A hysteroscopy may be used to remove an IUCD from within the uterine cavity provided it is proven to be there. An X-ray of the abdomen would be best to determine if the IUCD is in the abdomen. This can occur when the IUCD perforates through the uterus during insertion or finds a way to migrate to the abdominal cavity when initially inserted intrauterine.
If the IUCD is found outside the uterus but inside the abdominal cavity, a laparoscopy can be done to retrieve it.
MANAGEMENT OF LOST INTRAUTERINE DEVICE THREADS : If speculum examination reveals no IUD thread -
• Take a menstrual and sexual history, excluding pregnancy. Provide alternative contraception and/or post-coital contraception if indicated by history. If a woman is pregnant refer to the Early Pregnancy Unit for rapid access to ultrasound scans. The viability of pregnancy, site, and gestation will need to be determined. If the ultrasound scan reports the device is correctly located in the uterus, leave the IUD in situ until it is due to be removed. If an IUD is not seen in the uterus, order a plain abdominal X-ray.
• If an abdominal X-ray shows the IUD is in the abdominal cavity, this may require laparoscopic removal If an X-ray shows IUD is not located, this implies that the IUD has fallen out and a replacement of the IUD can be offered.
Q.26. A 26 year old woman presents with a “fishy” vaginal discharge. On examination, a homogeneous grey-white vaginal discharge is seen. Vaginal pH is 5.8. What is the most appropriate management?
Correct Answer : C
Please see Q-16
Q.27. A 36 year old female goes to her local GP clinic with the complaint of heavy menstrual bleeding. She also complains of pain in her lower abdominal area during her menstrual periods. She describes the pain as being intermittent in nature with a cramping quality. The pain sometimes radiates to her lower back. She takes standard over-the-counter paracetamol for the pain but she says that they provide only minimal relief. She has a standard 28 day menstrual cycle and describes her menstrual period as being regular in duration and onset, but extremely heavy in nature. She has had three children, and she claims that their births were all by elective caesarean section and that they were uncomplicated in nature. A urine pregnancy test comes up negative. Her past medical history is significant for her being diagnosed with a deep vein thrombosis five years ago. The patient was put on oral warfarin for three months after her diagnosis of a deep vein thrombosis. Now, she has no other medical problems and takes no chronic medications. A transvaginal ultrasound was done for the patient. The ultrasound revealed multiple small sized fibroids measuring about 2 cm x 2 cm in diameter. The fibroids do not distort the uterine cavity. What is the best contraceptive method to offer this patient?
Correct Answer : B
In this scenario, this patient needs a contraceptive method that will solve her excessive menstrual bleeding and which will cater to her specific needs. The levonorgestrel-releasing intrauterine system (Mirena) is the best option for this patient. The levonorgestrel-releasing intrauterine system (Mirena) is the best option for this patient to treat her heavy menstrual periods and to relieve her dysmenorrhoea.
It has been shown to reduce the severity of dysmenorrhoea even though it doesn’t affect or regulate the release of the female hormones that govern ovulation. According to guidelines, if a uterine fibroid is less than 3 cm by 3 cm in size and is not distorting the uterine cavity, medical treatments that can be considered are the intrauterine system, tranexamic acid, and the combined oral contraceptive pill.
We cannot offer the combined oral contraceptive pill in this patient as COCPs are contraindicated in patients with a history of venous thromboembolism. In the exam, if no contraindications exist for choosing the levonorgestrel-releasing intrauterine system, then choose that as an answer.
Q.28. A 31 year old primigravida at 24 weeks’ gestation was admitted 24 hours ago to the maternity unit because of preterm rupture of membranes (PROM). She is starting to have abdominal pains and uterine contractions. She has a pulse rate of 122 beats/minute and a temperature of 36.8 C. Routine examination of the patient’s abdomen reveals tenderness suprapubically. A speculum examination reveals a foul-smelling discharge originating from the cervix with the cervix slightly opened. What is the most likely diagnosis?
Correct Answer : C
Maternal tachycardia, tenderness suprapubically, and purulent vaginal discharge with a history of ruptured membranes points toward chorioamnionitis.
PROM is a major risk factor for ascending infections causing chorioamnionitis. Maternal tachycardia often precedes pyrexia hence the normal temperature given in this stem. There is no indication of miscarriage here which is characterized by vaginal blood loss.
CHORIOAMNIONITIS : Chorioamnionitis is an acute inflammation of the fetal amnion and chorion membranes, typically due to ascending bacterial infection from the vagina into the uterus in the setting of membrane rupture in pregnancy.
Features suggestive of chorioamnionitis :
• Fever
• Abdominal pain, including contractions
• Maternal pyrexia and tachycardia (tachycardia)
• Uterine tenderness
• Fetal tachycardia
• Foul odour of amniotic fluid
• Speculum: offensive vaginal discharge - yellowish brown
Risk factors :
• Prolonged labour
• Internal monitoring of labour
• Multiple vaginal exams
• Meconium-stained amniotic fluid
Q.29. A 33 year old woman presents to the GP surgery with a positive pregnancy test and concerns about this pregnancy. She has had 3 early miscarriages in the past with no live births. Based on her last menstrual period, she is now 6 weeks gestation. She was investigated for antiphospholid syndrome in the past and her lupus anticoagulant antibodies were found to be positive. Her BMI is 22 kg/m2 and she is a non-smoker. What is the most appropriate management?
Correct Answer : C
She has been diagnosed with antiphospholipid syndrome in the past. This puts her at risk for blood clots and she would eventually need heparin. Heparin and aspirin also reduce the risk of miscarriages in patients with diagnosed antiphospholipid syndrome.
Guidelines give clear recommendations for the use of prophylactic cerclage and prophylactic vaginal progesterone. They should be offered to women if she has a history of spontaneous preterm birth or mid-trimester loss between 16 weeks and 34 weeks of gestation AND in whom a transvaginal ultrasound scan has been carried out between 16 to 24 weeks of pregnancy that reveals a cervical length of less than 25 mm.
Prophylactic cervical cerclage can also be considered in women with cervical length less than 25 mm who have a history of cervical trauma like a LLETZ procedure. This patient had 3 early miscarriages and thus there is no indication of a cervical cerclage or progesterone pessaries.
CERVICAL CERCLAGE : Cervical weakness is a recognized cause of second-trimester miscarriage. The diagnosis is essentially a clinical one and based on a history of second-trimester miscarriage preceded by spontaneous rupture of membranes or painless cervical dilatation. Cervical cerclage does come with risks which are related to the surgery.
Risks include infections and rupture of the membranes. The criteria is a strict and complicated one thus it is unlikely to be a correct answer during EXAM. Nonetheless, if they do give a history of painless dilatation during previous miscarriages, cervical cerclage could be the option.
ANTIPHOSPHOLIPID SYNDROME : Antiphospholipid syndrome is the most important treatable cause of recurrent miscarriage. Antiphospholipid syndrome refers to the association between antiphospholipid antibodies (lupus anticoagulant, anticardiolipin antibodies, and anti-B2 glycoprotein-I antibodies) and adverse pregnancy outcomes or vascular thrombosis.
All women with recurrent first-trimester miscarriages and all women with one or more second-trimester miscarriages should be screened before pregnancy for antiphospholipid antibodies. Note the term recurrent miscarriage refers to the loss of three or more consecutive pregnancies.
If diagnosed with antiphospholipid syndrome, pregnant women can be treated with aspirin 75 mg plus heparin as this is seen to lower the risk of further miscarriage. Corticosteroids have no role in improving the live birth rate of women with recurrent miscarriages associated with antiphospholipid antibodies.
Q.30. A 26 year old woman with regular menses and her 28 year old partner comes to the GP surgery complaining of primary infertility. She and her husband have been trying to achive pregnancy for more than 2 years and have been unsuccesful. She has a regular 28 day menstrual cycle. Her BMI is 23. What is the most appropriate investigation to determine if she is ovulating?
Correct Answer : D
Day 21 progesterone which is the mid-luteal progesterone level is used to assess ovulation. If this is low, it may need repeating, as ovulation does not occur every month.
FSH and LH should be measured if there is menstrual irregularity :
High levels may suggest poor ovarian function.
A comparatively high LH level relative to FSH level can occur in PCOS.
In reality, we would obtain FSH, LH, and mid-luteal progesterone levels.
But for examination, always pick mid-luteal progesterone levels as the answer when it comes to infertility investigations.
Basal body temperature charts are not recommended to predict ovulation, as they are unreliable.
Causes of female infertility :
• Unexplained
• Ovulation failure
• Tubal damage
• Note that a history of pelvic inflammatory disease is highly suggestive of damage to tubes basic investigations.
• Serum progesterone 7 days prior to the expected next period. Meaning day 21 of a 28-day cycle. However, this day will need to be adjusted for different lengths cycle.
•This is also termed the “Mid-luteal progesterone level “
• It is done to assess ovulation. If low, it may need repeating, as ovulation does not occur every month.
Q.31. A 28 year old woman, gravida 2, para 1, comes to the maternity unit for evaluation for regular uterine contractions at 39 weeks’ gestation. Her previous delivery was an emergency cesarean section at 38 weeks for dystocia. She is now experiencing severe abdominal pain and profuse vaginal bleeding. Her heart rate is130 bpm, blood pressure is 95/55, oxygen saturation is 98% and temperature is 37.1 C. Reduced variability and late decelerations are now seen on CTG. What is the most likely diagnosis?
Correct Answer : C
Uterine rupture is the complete separation of the wall of the pregnant uterus with or without expulsion of the fetus that endangers the life of the mother the fetus, or both. This usually occurs during labour but has been reported antenatally.
Signs and symptoms:
• Tenderness over sites of previous uterine scars
• Fetal parts may be easily palpable
• Fetus not palpable on vaginal examination
• Vaginal bleeding may be evident
• Signs of maternal shock may be present. CTG may show fetal distress and change in apparent uterine activity (contractions may seem to disappear on the tocograph).
The most common risk factors are:
• Previous C-section or other uterine surgeries
• Excessive oxytocin stimulation
• Failure to recognize obstructed labour.
Diagnosis : Confirmation of the diagnosis is made by surgical exploration of the uterus and identifying the tear.
Management :
• Urgent laparotomy to deliver the fetus and repair the uterus.
Q.32. A 42 year old overweight smoker complains of heavy periods. An ultrasound scan reveals a normal uterus. She would like a long term treatment with minimal side effects that would offer treatment for the menorrhagia and provide contraception although she is still unsure if she would like children in the future. What is the most appropriate management?
Correct Answer : C
Among the options levonorgestrel intra-uterine system (Mirena coil) is the best treatment to reduce menorrhagia. It is currently the first-line treatment for menorrhagia. Combined oral contraceptive pills can do the job as well but she has already stated that she would want a long-term treatment with minimal side effects.
Thus the levonorgestrelintra-uterine system would be the most appropriate. Copper intrauterine contraceptive devices and progestogen implants are more prone to have irregular heavy bleedings compared to levonorgestrel intra-uterine system(Mirena coil). Endometrial ablation does affect fertility and is not an appropriate management for a woman who may still want children in the future.
MENORRHAGIA MEDICAL MANAGEMENT : Guidelines has suggested that this medical management of heavy menstrual bleeding should be considered in the following order:
1. Levonorgestrel-releasing intrauterine system.
2. Tranexamic acid or non-steroidal anti-inflammatory drugs (NSAIDs) or combined oral contraceptives.
3. Norethisterone (15 mg) daily from days 5 to 26 of the menstrual cycle, or injected long-acting progestogens. This should be taken into account if contraception is desired. If contraception is desired, then preference would go towards the intrauterine system (Mirena) followed by COCP and injected long-acting progestogens.
Important combinations :
• A combination of tranexamic acid and a nonsteroidal anti-inflammatory drug (NSAID) can be used if the patient has both menstrual bleeding and dysmenorrhoea
• A combination of NSAID and COCP can be used if dysmenorrhoea is problematic
• Do NOT combine tranexamic acid with a COCP or Mirena coil For heavy menstrual bleeding that needs stopping rapidly:
• Oral norethisterone 5 mg three times daily for 10 days In secondary care,
Treatment includes:
• Gonadotrophin-releasing hormone (GnRH) agonists.
The management of menorrhagia and fibroids overlap considerably. So it is always wise to go through these two topics together.
Q.33. A 34 year old woman presents to the infertility clinic with her husband. They have been trying to conceive for 3 years but have not been succesful despite having regular intercourse. Her BMI is 31 kg/m2. She has dark pigmentation on her neck and severe acne on her face. She also complains of thinning of her hair. She was sent for an ultrasound scan which showed multiple follicles on both her ovaries. What is the most appropriate initial management to treat her infertility?
Correct Answer : B
The question here describes the signs and symptoms of polycystic ovarian syndrome (PCOS). The scenario of acne on her face points towards an excess of androgens (hirsutism, alopecia, and acne are all manifestations of hyperandrogenism). Not to mention that her initial complaint was infertility which is one of the diagnostic criteria for PCOS.
The dark pigmentation on her neck is called acanthosis nigricans which is characterized by brown to black hyperpigmentation of the skin found in body folds, such as the axilla, nape of the neck, and groin. It is a marker of insulin resistance.
Weight loss is the most appropriate answer as part of INITIAL management. Clomifene citrate is an option together with weight loss however it is advisable to encourage weight loss first. In practice, we would advise patients to lose weight while getting blood tests done to confirm anovulation.
Some clinicians would start them on metformin right away on their first visit. This is a debatable action but since metformin was not given in the options, we shall not discuss it here. Just note that metformin is currently unlicensed for use in PCOS and so women would need to be counseled carefully before initiating therapy.
Laparoscopic drilling is a treatment for infertility for PCOS but is not the first line. COCP is a treatment for PCOS to regulate irregular periods but it is not for treatment of infertility.
Spironolactone (an antiandrogen) is used by endocrinologists to help with the effects of hirsutism. But again, this will not help with infertility.
Q.34. A 17 year old girl with primary amenorrhoea complains of severe abdominal pain every 4 to 8 weeks which is now getting worse. On abdominal examination, a lower abdominal mass is felt. What is the most likely diagnosis?
Correct Answer : D
The key word here is primary amenorrhoea. This means that she has never had her menses before. The only possibility among the options given that could cause primary amenorrhoea is haematometra. Primary amenorrhoea and cyclical pain indicate haematometra. Haematometra is an accumulation of blood within the uterus.
One of the causes of haematometra that is associated with primary amenorrhoea is an imperforate hymen or a transverse vaginal septum. In an imperforate hymen, one might have a bluish bulging membrane visible at the introitus.
A transverse vaginal septum may present with a possible abdominal mass.
Q.35. A 34 year old lady comes to the GP for removal of an intrauterine device. On speculum examination, the cervix is visualised but the intrauterine device thread is not seen. Her last menstrual period is 2 weeks ago and she has been having regular sexual intercourses with her partner. She has a negative pregnancy test. What is the most appropriate action?
Correct Answer : A
Transvaginal ultrasound is a good step to locate if the intrauterine device is still intrauterine, displaced, or fallen out. It is unlikely that it has perforated the uterus as if, the patient would be presenting with an acute abdomen.
Transvaginal ultrasound has better image quality when looking at the uterus compared to a transabdominal ultrasound.
An X-ray is capable of seeing the intrauterine device as well but it is reserved for more acute presentations like suspected perforation or when the IUD is not seen on an ultrasound scan.
Combined oral contraceptives are not completely wrong as if there was a delay in obtaining the ultrasound scan, it may be necessary to start the woman on a form of contraception until the ultrasound scan can be performed. The choice of your answer depends on how the question is phrased. If the last line of the question asks “What is the most appropriate NEXT step” or “What is the most appropriate IMMEDIATE action”, prescribing a form of contraception would be your best pick.
Q.36. A 30 year old woman with suspected pelvic inflammatory disease has worsening of her symptoms of lower abdominal pain despite being treated with oral metronidazole and ofloxacin for 14 days. She has a temperature of 38.6 C, heart rate of 85 bpm, and a blood pressure of 110/80 mmHg. Her blood tests show: White cell count 18 x 109/L CRP 160 mg/L What is the most appropriate next course of action?
Correct Answer : A
The possible diagnosis here is a pelvic abscess or tubo-ovarian abscess which are complications of PID. A high vaginal swab or endocervical swab can take days to return with results.
As this is an A&E case, an ultrasound would be more appropriate as this would lead to a diagnosis. Ultrasound scan is the diagnostic imaging method of choice for acute pelvic pain in gynaecology.
It can easily diagnose sequelae of PID (including pyosalpinx and tubo ovarian abscess). Laparoscopy would be the next step after finding a mass on ultrasound. Urine culture has no part in the diagnosis of pelvic abscess.
Q.37. A 29 year old woman’s recent cervical smear results show inflammatory changes without any dyskaryosis. She has no pelvic or vaginal pain. There was no discharge on examination. Speculum examination had shown a normal cervix and vaginal mucosa. What is the most appropriate action?
Correct Answer : B
The results that show inflammatory changes are nonspecific. These findings are difficult to interpret. It may be nonsignificant or it may also represent genital infections like candida amongst others.
Inflammation is usually not a worrying sign unless it is severe in which case we may consider a more serious sexually transmitted infection. It is good practice to repeat the smear in 6 months to ensure that the inflammation has resolved.
Q.38. A 28 year old woman at 31 weeks gestation attends the antenatal clinic. Her full blood count was taken when she was 28 weeks which results show: Haemoglobin 10.6 g/dL Mean cell volume 96 fL Mean cell haemoglobin concentration 350 g/L. What is the most appropriate management?
Correct Answer : C
The values of anaemia differ in pregnancy as compared to a non pregnant women.
Anemia in pregnancy as the following values Hb levels of:
<11.0g/dl in the first trimester
<10.5 g/dl in the second and third trimesters <10.0 g/dl in the postpartum period.
Since her Hb level is above 10.5g/dL, she does not need iron tablets.
This is one of the questions that differ in terms of how you answer in exam and how you would act in real life.
Again, it depends on hospital guidelines.
Q.39. A 23 year old woman is followed up for 6 weeks after a surgical procedure to evacuate the products of conception in the uterus following a miscarriage. The histology shows changes consistent with a hydatidiform mole. What is the most appropriate investigation in this case?
Correct Answer : D
Serum and urine samples of hCG concentrations are extremely important. In hydatidiform moles, hCG levels are likely to be raised excessively (especially in incomplete moles). Management would involve surgical evacuation, after which the hCG levels are expected to return to a normal, non-pregnant level.
We would like the hCG to go down towards a normal level but If it plateaued or if hCG levels rise after evacuation, chemotherapy is indicated.
This is the reason it is so important not to get pregnant during the time that hCG levels are decreasing if one were to get pregnant, hCG levels would increase again, and we would not know if it is due to the hydatidiform mole or the new pregnancy.
Q.40. A 33 year old lady who is now 28 weeks pregnant comes to the antenatal clinic with pain and swelling on her left calf muscle. On physical examination, she has distension of superficial veins and increased skin temperature at affected area. What is the most appropriate treatment?
Correct Answer : A
Any pregnant woman with symptoms and/or signs suggestive of venous thromboembolism should have objective testing performed expeditiously and treatment with low-molecular-weight heparin (LMWH) given until the diagnosis is excluded by objective testing unless treatment is strongly contraindicated.
Q.41. A 15 year old female presents to the abortion service requesting a surgical termination of pregnancy. She is 10 weeks of gestation and has hid the pregnancy thus far from her parents and her partner. Her parents, who accompany her, disapprove of her decision and wish for her to see the pregnancy to term and then give the baby up for adoption. A consult with the patient in private reveals that she understands all aspects and risks of a surgical termination of pregnancy. She is adamant that she wants to have a surgical termination of her pregnancy without involving her partner and all efforts to persuade her otherwise have failed. What is the most appropriate conclusion?
Correct Answer : D
The guidance on termination of pregnancy in patients who are under 16 is clear. In summary, female patients under the age of 16 do not need parental consent to request a termination of pregnancy using either medical or surgical methods if:
• The patient understands all aspects of the procedure
•The patient’s physical or mental health is likely to suffer unless they receive a termination The consent of a young patient with Gillick competence and full mental capacity overrides parental refusal. Consent from the partner is not required. The decision to involve the partner is up to the patient as the partner has no legal right to be informed or consulted.
Q.42. A 28 year old female who is four weeks pregnant presents to the antenatal clinic for a check-up. She expresses a concern about ectopic pregnancies and wants to know the risk of her having an ectopic pregnancy. The patient claims that she read a NHS leaflet about ectopic pregnancies a few days ago and that it had gotten her worried that she might have an ectopic pregnancy. She is in a stable relationship with her boyfriend of three years and has no significant medical or surgical history. What is the most likely risk factor for an ectopic pregnancy?
Correct Answer : A
According to guidelines, one-third of women with ectopic pregnancies do have prior risk factors that predispose them to having an ectopic pregnancy. However, few risk factors are recognized only in around 25% of patients who are diagnosed with ectopic pregnancy.
Pelvic inflammatory disease is the most common cause of ectopic pregnancy. It may cause complete obstruction of the fallopian tube or it can even delay the transport of the embryo so that implantation occurs in the tube.
Predisposing factors for ectopic pregnancy include:
• Previous tubal pregnancy
• Previous induced abortion
• Pelvic inflammatory disease
• Previous ectopic pregnancy
• IUCD – (relative risk) conception rarely occurs with an intrauterine device in place but around half of such pregnancies conceived are thought to be ectopic
• Tubal ligation
Q.43. A 32 year old female who has completed her family wants to know more about contraception and the risk of ectopic pregnancies. Which of the following contraceptive method increases the absolute risk of ectopic pregnancies?
Correct Answer : C
This question by the examiners is written purely to test your knowledge of absolute and relative risk. You would need to know a little about the background of intrauterine systems. The absolute risk of ectopic pregnancy with the mirena coil is decreased but the relative risk is increased.
This means that if you were to become pregnant while on the Mirena coil, the risk of it being ectopic is higher as compared to if you were to become pregnant while you were not on the Mirena coil.
The risk of ectopic pregnancy when using IUDs is lower than when using no contraception.
If a woman becomes pregnant with the IUD in situ, the risk of ectopic pregnancy is about 1 in 20.
Q.44. A 29 year old woman at 38 weeks of gestation presents with a 2 hours history of constant abdominal pain. While waiting to be seen, she passes 300 ml of blood per vagina. There has been reduced fetal movement since the episode of bleeding. What is the most appropriate next step?
Correct Answer : B
With constant abdominal pain and PV bleeding, placental abruption is one of our differences. The first and most important step is to put on a cardiotocograph (CTG).
If there is fetal distress seen on the CTG, the woman may be rushed for an emergency C-section. As abruption is a clinical diagnosis, an ultrasound would have little value.
A CTG is extremely important as a first step to monitoring the fetus.
An ultrasound would be a good step to perform to rule out placenta praevia if the CTG is found to be reassuring.
A group and save is also important as she is having PV bleeding, but the importance of monitoring the fetus comes above having a group and save as most maternity units will have O-type blood stored in the fridge.
Q.45. A 25 year old primigravida at 30 weeks’ gestation comes to the maternity unit stating that 3 hours ago she had a gush of clear fluid from her vagina. She has no uterine contractions. She has a pulse rate of 110 beats/minute and a temperature of 38.4 C. Routine examination reveals a purulent yellow vaginal discharge with cervix slightly opened. Her blood tests show: Haemoglobin 115 g/L White cell count 21 x 109/L Platelets 260 x 109/L CRP 253. What is the most likely diagnosis?
Correct Answer : C
Fever, maternal tachycardia, tenderness suprapubically, and purulent vaginal discharge with a history of ruptured membranes points towards chorioamnionitis. The blood tests also show an inflammatory response with a high CRP and high white cell count. There is no indication of miscarriage here which is characterized by vaginal blood loss. Although endometritis is a possibility, this is a more common complication in the postpartum period.
Q.46. A 27 year old presents to the Emergency Department with left sided abdominal pain and vaginal spotting. Her last menstrual period was 7 weeks ago. Her abdomen was tender to palpate and cervical motion tenderness was noticed on examination. Transvaginal ultrasound scan was perfomed which showed an empty uterus. Serum human chorionic gonadotrophin (hCG) is 4900 IU/litre. Her observations include a blood pressure of 105/65 mmHg, heart rate of 80 beats/minute and respiratory rate of 18 breaths/minute. Her pain is not resolving despite morphine sulphate administered orally. What is the most appropriate next course of action? (A serum hCG above 25 IU/litre is considered positive for pregnancy)
Correct Answer : D
It is clear here that she has an ectopic pregnancy. As she is haemodynamically stable, a laparoscopic approach to the surgical management of tubal pregnancy is warranted. Laparotomy would be the choice if the patient is haemodynamically unstable. The reason for this is laparotomy is quicker than a laparoscopy. Methotrexate would be the first line for an ectopic pregnancy if she was not in significant pain.
Q.47. A 33 year old woman, gravida 2, para 1, comes to the maternity unit for evaluation for regular uterine contractions at 38 weeks’ gestation. Her previous delivery was an emergency cesarean section at 39 weeks due to a breech fetus. She is now experiencing severe abdominal pain and tenderness over the previous uterine scars. CTG shows fetal distress and absent uterine contractility. What is the most likely diagnosis?
Correct Answer : C
Please see Q-31
Q.48. A 25 year old woman had a spontaneous vaginal delivery 4 weeks ago. She delivered a healthy baby. There were no complications throughout labour and in the postpartum period. She now presents with bleeding per vaginum. She describes them as like a period bleed. Her blood pressure is 120/70 mmHg. Her pulse rate is 70 beats/minute and respiratory rate is 15 breaths/minute. She has a temperature of 37 C. What is the next most appropriate action?
Correct Answer : A
This is likely her menstrual cycles returning. Menstrual cycles could return as early as 21 days postpartum in a woman who is not breastfeeding. The fear here is missing a secondary postpartum haemorrhage associated with endometritis or placental tissue remaining in the uterus.
However, if there was an infection, the question writers would normally provide additional hints such as fever, offensive-smelling lochia, or feeling unwell. That being said, in a well patient like the above, it would be reasonable to just reassure.
There may also be retained pieces of the placenta after 4 weeks, however, with a small amount of bleed and normal observations, it is unlikely that any obstetrician would order a pelvic ultrasound.
A pelvic ultrasound would be ordered if the patient was haemodynamically unstable or if there were signs of an infection.
Q.49. A 29 year old woman stopped taking combined oral contraceptive pills 6 months ago and she has been amenorrhoeic since then. Ultrasonography reveals normal ovaries with no signs of developing follicles. Her blood results show: Follicle stimulating hormone (FSH) 8 IU/L Luteinizing hormone (LH) 9 IU/L Prolactin 44 ng/mL Oestradiol 53 pmol/L What is the most likely cause?
Correct Answer : B
POST PILL AMENORRHOEA : Post-pill amenorrhoea occurs when stopping oral contraceptives does not lead to a resumption of a normal menstrual cycle. It is described as the loss of menstrual periods for at least 6 months after stopping birth control pills. Post-pill amenorrhea is believed to be due to suppression of the pituitary gland by birth control pills.
Investigations are usually needed if menstrual cycles do not resume after 3 months of postpill.
It may be that the cause of amenorrhoea started whilst taking the contraceptives which induced an artificial cycle, masking the issue until they were stopped.
• Ultrasonography will reveal ovaries with no signs of developing follicles and ovulation even after having stopped the pills for 6 months
• Blood tests showing a low level of FSH, LH, and oestrogen are usually sufficient to confirm the diagnosis.
Treatment :
• The first line of treatment in case of post-pill amenorrhea is waiting for a spontaneous remission of the amenorrhea and a spontaneous occurrence of periods.
• The time limit is usually six months. But if the woman is anxious to get her period, active treatment may be started after waiting for only three months. The standard treatment of post-pill amenorrhea is by stimulating the pituitary to produce FSH and LH. This is done by the drug clomiphene citrate.
AMENORRHOEA : is the absence of menstruation. Pathological amenorrhoea is the failure to menstruate for at least 6 months.
Amenorrhoea can be divided into:
• Primary amenorrhoea – lack of menstruation before age 16 years or 14 in the absence of secondary characteristics
• Secondary amenorrhoea – cessation of menstrual cycles following established cycles.
Aetiology :
• Hypothalamic amenorrhoea - Most common. Usually due to low BMI or excessive exercise.
• Polycystic ovarian syndrome (PCOS)
• Hyperprolactinaemia
• Premature ovarian failure - Raised FSH levels
• Anatomical problems - Usually results in primary amenorrhoea. Vaginal examinations to rule out imperforate hymen is important. Pelvic ultrasound is also useful to determine the pelvic anatomy (Mullerian agenesis). Anatomical problems can also cause secondary amenorrhoea (Asherman’s syndrome).
• Thyroid problems - Both hyperthyroidism and hypothyroidism can cause amenorrhoea. Don’t forget pregnancy as a cause of amenorrhoea (Specific to look for in the stems)
• Short stature – may indicate Turner syndrome
• Hirsutism, acne (androgen excess) – May indicate PCOS or hyperprolactinemia
• Menopausal symptoms in women before age 40 – May indicate premature ovarian failure
• Eating disorder – May indicate anorexia nervosa
• Galactorrhoea – May indicate hyperprolactinemia.
Q.50. A 25 year old lady has had an uncomplicated pregnancy so far. She is now 39 weeks gestation. She was admitted because she had a show and has regular and painful uterine contractions. Her cervix is now 10 cm dilated and she has started pushing. What stage of labour is she in?
Correct Answer : C
Labour may be divided into three stages :
• Stage 1: from the onset of true labour to when the cervix is fully dilated. It is divided into a latent and an active phase. The latent phase begins with the onset of regular contractions and ends with the acceleration of cervical dilation. Active phase begins with cervical dilation acceleration, usually at 3-4 cm of dilation, ending with complete cervical dilation.
. • Stage 2: from full dilation to delivery of the fetus
• Stage 3: from delivery of fetus to when the placenta and membranes have been completely delivered.
Signs of labor include :
• Regular and painful uterine contractions
• A show (shedding of mucous plug)
• Rupture of the membranes (not always)
• Shortening and dilation of the cervix.
Q.51. A 33 year old lady attends the obstetric assessment unit with a history of a positive pregnancy test and bleeding from her vagina for the last two days. Her last menstrual period is 8 weeks ago. On speculum examination, the cervical os is closed but blood is seen in the vault. What is the most appropriate next step to determine the viability of the fetus?
Correct Answer : A
A transvaginal ultrasound is most specific to identify the viability of the fetus.
Q.52. A 31 year old pregnant woman has her antenatal screening at her booking appointment for HIV and Hepatitis B status. What other routine investigations are ordered at booking?
Correct Answer : C
The following are routine blood tests performed at the booking :
• Blood Group and antibodies
• Rhesus status
• Haemoglobinopathies
• Syphilis
• Hepatitis B status
• HIV
• Full blood count looking for anaemia
• Rubella susceptibility
Q.53. A 33 year old female presents with sudden severe colicky abdominal pain at her right iliac fossa. The pain is severe and has worsened intermittently over the last few hours. The pain radiates to her back and pelvis. She has also been vomiting and feeling nauseous since the pain started. A tender, mobile mass is felt at the right iliac fossa on examination. What is the most likely diagnosis?
Correct Answer : B
The likely diagnosis here is ovarian torsion. Although ovarian torsion cannot be diagnosed clinically as it is often diagnosed in theatre during a laparoscopy, the question writers want you to consider ovarian torsion as part of your differential diagnosis as it is one of the important gynaecologic emergencies.
It is quite rare and only accounts for about 3% of gynaecologic emergencies however it is important to consider it especially given that this patient has a tender mobile mass at the right iliac fossa.
In clinical practice, appendicitis would also be part of your differential. If there was a history of an ovarian mass or if an ultrasound pelvis was done which found an ovarian mass, then the surgeons would refer her to the gynaecology team to rule out an ovarian torsion.
Ovarian torsion presents with sudden onset of sharp, unilateral lower abdominal pain often with nausea and vomiting. In the reproductive years, regular growth of large corpus luteal cysts is a risk factor for rotation.
Any enlargement of the ovary is a risk factor for ovarian torsion. The definitive diagnosis is often made in the theatre as ovarian torsion is difficult to diagnose accurately and an operation is often performed before the diagnosis is made.
Q.54. A 34 year old pregnant woman in her first trimester complains of a thick white vaginal discharge 3 days after starting antibiotics which was prescribed by her dentist for a dental abscess. What is the most likely reason for her vaginal discharge?
Correct Answer : C
Pregnant woman and recent use of antibiotics predisposes her to higher risk of developing vaginal candidiasis. She was likely prescribed a broad-spectrum antibiotic which has destroyed the normal flora leading to the development of vaginal thrush.
It is well known that broad-spectrum antibiotics destroy healthy bacteria and disrupt the vagina’s normal flora which can predispose women to develop either vaginal candidiasis due to the change of the natural balance of bacteria in the vagina.
Why pick candidiasis and not Gardnerella While both may be good answers, candidiasis is more likely a better answer as broad-spectrum antibiotics that inhibit lactobacilli also inhibit Gardnerella which makes it less likely to trigger bacterial vaginosis.
Q.55. A 60 year old woman complains of bleeding after having intercourse. In the past month, she has had 3 episodes of mild vaginal bleeding. She had regular withdrawal bleeds until 8 years ago and has not had a bleeding since. Her last cervical smear was 3 years ago which showed no abnormalities. A speculum examination shows a normal cervix and vagina. What is the most likely diagnosis?
Correct Answer : B
The idea here is to think of endometrial cancer. Any woman who has postmenopausal bleeding should have a transvaginal ultrasound to determine the endometrial thickness. If the endometrium is thick, a hysteroscopy with endometrial biopsy would be arranged.
A cervical smear is offered every 5 years if in the age group of 50 to 64 years old. Thus, having a cervical smear that was normal 3 years ago is a usual phenomenon. A repeat cervical smear is not necessary.
ENDOMETRIAL CANCER : Endometrial cancer is classically seen in post-menopausal women.
Classically, endometrial cancer presents as postmenopausal bleeding (PMB), and, although this is not the only cause, it must be excluded.
Risk factors for endometrial cancer:
• Obesity
• Nulliparity
• Early menarche
• Late menopause
• Unopposed oestrogen.
The addition of a progestogen to oestrogen reduces the risk (e.g. In HRT). Additional risk is eliminated if the progestogen is given continuously.
• Diabetes mellitus
• Tamoxifen
• Polycystic ovarian syndrome
Features in exam, they will always present with postmenopausal bleeding.
Investigation :
• First-line investigation is trans-vaginal ultrasound - a normal endometrial thickness (< 4 mm) has a high negative predictive value.
• Hysteroscopy with endometrial biopsy gives the definitive diagnosis.
Management Is beyond the scope of exam.
Q.56. A 38 year old female attends the clinic because of issues of infertility. She also says that her last period was 9 months ago. Lab results show: Follicle stimulating hormone (FSH) 59 U/L Luteinizing hormone (LH) 78 IU/L Prolactin 12 ng/mL Oestradiol 25 pmol/L An FSH was repeated 4 weeks later which was still elevated. What is the most likely diagnosis?
Correct Answer : D
The diagnosis of premature ovarian failure usually needs two raised levels of FSH(more than 40 IU/L) taken at least four weeks apart. In this question, since she is amenorrheic with raised FSH and LH and a normal prolactin level, the most likely diagnosis would be premature ovarian failure. Women with premature ovarian failure also have low estradiol (usually < 50 pmol/l).
PREMATURE OVARIAN FAILURE : Premature ovarian failure (Premature ovarian insufficiency) is defined as the onset of menopausal symptoms and elevated gonadotropin levels before the age of 40 years.
Causes :
• Idiopathic - the most common cause
• Chemotherapy (this can be temporary, as recovery of ovarian function can occur, especially in younger women)
• Radiation
• Autoimmune disease
• Bilateral oophorectomy or surgical menopause
Presentation :
1. The most common presentation is amenorrhoea or oligomenorrhoea (which may not necessarily be accompanied by hot flushes)
2. Infertility
3. Other features are similar to those of the normal climacteric symptoms:
• Hot flashes
• Night sweats
• Irritability
• Poor concentration
• Decreased sex drive
• Dyspareunia
• Vaginal dryness Tests: FSH levels: FSH test should be undertaken in women aged under 40 years in whom menopause is suspected.
• Two raised levels (more than 40 IU/L) taken at least four weeks apart are diagnostic. Serum follicle-stimulating hormone (FSH) measurement alone can be used to diagnose the disease. The anterior pituitary secretes FSH and LH at high levels due to the dysfunction of the ovaries and consequent low estrogen levels.
Management:
• Hormone replacement therapy (HRT) until at least the average age of the menopause (51 years).
• The term early menopause is used for those women who go through their menopause between 40-45 years. Do NOT use premature menopause and premature ovarian failure interchangeably.
• Premature ovarian failure is sometimes referred to as premature menopause, but the two conditions aren't the same. Women with premature ovarian failure may have irregular or occasional periods for years and may even become pregnant. Women with premature menopause stop having periods and can't become pregnant.
Q.57. A 33 year old woman with a background history of sickle cell disease complains of heavy menstrual blood loss over the past year. She is not sexually active and has no plans for children in the near future. What is the most appropriate management?
Correct Answer : C
There is always concern about women with sickle cell disease using hormonal medications as there is the fear that their blood vessels would be blocked by blood clots.
The first step towards picking an answer here is using UKMEC as a guide :
: • Sickle cell disease is considered UKMEC 2 for copper IUD as there are concerns of increased risk of blood loss with its use.
• Sickle cell disease women may use progestogen-only implants, depot medroxyprogesterone acetate (DMPA) or progestogen-only pill (POP) as evidence concludes that these do not have adverse effects on hematological parameters (UKMEC 1)
• Mirena coil (IUS) is also considered UKMEC 1 and is generally associated with reduced blood loss. As COCP and IUD are UKMEC 2, they are not going to be the right options when there are better alternatives (UKMEC 1).
So why pick DMPA over POP or IUS in this question?
Depot medroxyprogesterone acetate (DMPA) is a long-acting injectable contraceptive that may reduce menstrual bleeding or cause amenorrhoea with the additional benefits that it is preferred in women with sickle cell disease because it reduces the frequency and severity of painful crises.
Remember this note:
Whilst all three (POP, IUS, and DMPA) are completely safe to use in patients with sickle cell disease, evidence shows that DMPA reduces the severity of sickle crisis pain.
Q.58. A 56 year old woman who is a heavy smoker is diagnosed with cervical intraepithelial neoplasia grade 2. She is a mother of three children. She is worried of ovarian cancer because her older sister died of ovarian cancer. She has been on hormone replacement therapy for 3 years. What is the most relevant risk factor for ovarian cancer in her case?
Correct Answer : A
A family history of ovarian cancer is an important risk factor. Women with a first-degree relative with ovarian cancer have 3-4 times the risk of developing the disease.
However, only 10% of cases arise in women with a positive family history. Smoking is a risk factor but it is not as important as family history.
It is estimated that 2% of cases may be caused by smoking. HRT increases the risk of developing ovarian cancer but only slightly and it is only seen in patients using HRT for more than five years. About 1% of cases may be linked with taking HRT.
Ovarian Cancer Risk factors :
• Family history: mutations of the BRCA1 or the BRCA2 gene
• Many ovulations: early menarche, late menopause, nulliparity
• Age incidence increases with age
Protective factors against ovarian cancer:
• COCP
• Pregnancy
Q.59. An 18 year old girl who has mild learning difficulties attends the GP surgery seeking advice on contraception. She is sexually active and currently using condoms however she would like to try a different contraceptive method that is more secure. She has no relevant past medical history. What is the most appropriate contraception for her?
Correct Answer : B
The ideal contraception for her would be an etonogestrel implant like NexplBatman. Mirena and Depo-Provera would not be ideal as it is considered UKMEC 2 under 20 years of age whereas POP, COCP, and implants are UKMEC 1 and are recommended as first-line for young women. She has mild learning difficulties and being a teenager she is likely to forget to take regular pills.
Q.60. A 34 year old woman develops a fit 6 hours after having a spontaneous vaginal delivery of a healthy term baby. She has no history of having high blood pressure and has not had a seizure before. What is the most likely diagnosis?
Correct Answer : A
It is very unlikely for eclamptic fits to occur with no history of proteinuria or high blood pressure in the past. But given that she is pregnant and just delivered, it is the most likely given the options. Eclampsia does occur in the postpartum period as well as antenatally.
This is why it is common practice to keep patients with severe pre-eclampsia in the hospital for the next few days post-delivery even though the delivery was uncomplicated.
Q.61. A 27 year old Asian primiparous woman with type 1 diabetes mellitus has delivered a baby weighing 4.5 kg with the help of forceps. The placenta was removed with continuous cord traction and her uterus is well contracted however she continues to bleed heavily. What is the most likely cause of her postpartum haemorrhage?
Correct Answer : C
The most common cause of postpartum haemorrhage is uterine atony however this is not the case here as the uterus is well contracted. The risk factors point towards genital tract trauma. Asian ethnicity, nulliparous, diabetic, and big baby were thrown in these are risk factors for a 3rd and 4th-degree perineal tear which can be the sole cause of the PPH.
Causes for PPH may be considered to relate to one or more of ‘the four Ts’:
• Tone (abnormalities of uterine contraction)
• Tissue (retained products of conception)
• Trauma (of the genital tract)
• Thrombin (abnormalities of coagulation).
The most common cause of primary PPH is uterine atony.
However, clinical examination must be undertaken to exclude other or additional causes:
• Retained products (placenta, membranes, clots)
• Vaginal/cervical lacerations or haematoma
• Ruptured uterus
• Broad ligament haematoma
• Extragenital bleeding (for example, subcapsular liver rupture)
• Uterine inversion
Q.62. A 33 year old diabetic woman at 41 weeks gestation is in labour. She is fully dilated and has been pushing for 1 hour. The fetal head is delivered with no difficulty. The shoulders restitute but with every contraction, the fetal head emerges then retracts immediately following the contraction. What is the most appropriate next action?
Correct Answer : D
The term for the head retracting is called the “turtle sign”. It is seen in shoulder dystocia. At this stage, the first step is to call for help then evaluate for episiotomy and start McRoberts maneuver. There is no need for an episiotomy prior to McRoberts maneuver but it is advisable to perform an episiotomy before any enter rotation maneuvers.
This creates more room for the obstetrician to use his fingers and hands to perform rotation maneuvers. Remember: Shoulder dystocia is a bony impaction, so episiotomy alone will not release the shoulder. The diabetes thrown into this stem is just to highlight that she has risk factors for shoulder dystocia.
RISK FACTORS FOR SHOULDER DYSTOCIA :
The key risk factors to remember for shoulder dystocia can be divided into two categories:
Pre-labour risk factors -
• Fetal macrosomia > 4.5 kg
• Maternal BMI > 30 kg/m2
• Diabetes mellitus
• Previous shoulder dystocia
• Induction of labour
Intrapartum risk factors -
• Prolonged labour
• Oxytocin augmentation
• Assisted vaginal delivery
• Episiotomy
Q.63. A 42 year old primigravid woman who is now 38 weeks pregnant is brought in by her husband because of sudden onset of lower abdominal pain, back pain and vaginal bleeding. She describes blood loss of about 200 ml. She denies any trauma to her abdomen. Her uterus is tender and hard on examination. Uterine contractions can be palpated and there is still evidence of vaginal bleeding. Fetal distress is seen on CTG. She has a pulse rate of 120 beats/minute and a blood pressure of 95/60 mmHg. What is the most likely cause of her symptoms?
Correct Answer : A
It is worth remembering that maternal age is a risk factor for placental abruption and those over 35 years are at greater risk. In this stem, an age of 42 was used. Although trauma may elicit placenta abruption, the majority of abruptions do not have a background history of injury to the abdomen. Back pain can be a presentation of placenta abruption if the placenta is located posteriorly. This needs to be dealt with rather urgently with an emergency caesarean section as fetal distress is often followed by fetal death in abruptions.
PLACENTAL ABRUPTION : Placental abruption is the premature separation of a normally placed placenta resulting in maternal bleedinghemorrhagic behind the placenta or loss through the cervix.
The cause is not known but associated factors include:
• Pre-eclampsia
• Multipolarity
• Trauma
• Maternal age
• Cocaine • Smoking
Clinical features :
- Abdominal pain is constant
• Very tender and tense uterus (woody hard)
• Bleeding, which may be accompanied by pain
• Fetal distress or fetal death
• Maternal signs of hypovolemic shock if bleeding is severe. Severe abruption can result in haemorrhagic shock with acute tubular necrosis from profound hypotension. Disseminated intravascular coagulation can result from the release of tissue thromboplastin into the circulation from the disrupted placenta. One should not look at the extent of vaginal loss as an indicator of the severity of abruption ahemorrhagethe haemorrhage may be much much greater (it is just concealed behind the placenta)
Management :
• Resuscitation and delivery if presence of fetal distress or maternal compromise.
Q.64. A 22 year old woman who was diagnosed with a missed miscarriage a week ago presented to the hospital last night with abdominal pain and vaginal bleeding. Since then, she has passed a small fetus. A transvaginal ultrasound was repeated which showed an empty uterus. The pain is slowly easing off. What is the most likely diagnosis?
Correct Answer : C
A complete miscarriage is a spontaneous abortion with the expulsion of the entire fetus through the cervix. Pain and uterine contractions cease after the fetus has been expelled. An ultrasound scan would show an empty uterus.
Q.65. A 26 year old lady presents with worsening lower abdominal pain and purulent vaginal discharge. She was recently treated for pelvic inflammatory disease with antibiotics as an outpatient but did not complete her course of antibiotics. A urine HCG is negative. Cervical motion tenderness was noted when doing a pelvic examination. She has a temperature of 38.6 C and a pulse rate of 95 beats/minute. What is the most appropriate action?
Correct Answer : D
This patient needs to be admitted for antibiotics. An outpatient therapy has already failed. She has signs and symptoms of pelvic inflammatory disease. She has a high temperature and tachycardia. One of the more common inpatient regimens for pelvic inflammatory disease is IVceftriaxone 2g daily plus IV doxycycline 100mg twice daily (oral doxycycline may be used if tolerated) followed by oral doxycycline 100mg twice daily plus oral metronidazole 400mg twice daily for a total of 14 days.
Intravenous therapy should be continued until 24 hours after clinical improvement and then switched to oral.
Although it’s stated that we use intravenous doxycycline as part of the antibiotic regimen, this is usually not the case as Intravenous doxycycline is not currently licensed. Whilst taking triple swabs is appropriate, we should not wait for results before commencing antibiotics.
Antibiotics should be commenced immediately to avoid complications such as tubo-ovarian abscess or tubal damage leading to infertility. Once culture and sensitivity results are available, a change of antibiotics may be required. The change usually involves ofloxacin as gonorrhoea is increasingly resistant to fluoroquinolone.
OPTIONS FOR MANAGEMENT OF PID :
• IM ceftriaxone stat plus oral doxycycline and oral metronidazole for 14 days; or
• Ofloxacin and metronidazole orally for 14 days Inpatient management of PID
• IV ceftriaxone and IV doxycycline followed by oral doxycycline and oral metronidazole for 14 days; or
• IV ofloxacin and IV metronidazole for a total of 14 days.
Q.66. A 33 year old woman, with 3 previous normal vaginal deliveries complains of urinary leakage when she plays tennis or coughs. What is the most likely diagnosis?
Correct Answer : A
Please see Q-4
Q.67. Which of the following is true regarding treatment with tamoxifen?
Correct Answer : B
Tamoxifen is a risk factor for endometrial carcinoma. Tamoxifen is a Selective estrogen receptor modulator (SERM) used in the treatment of breast cancer. Even though it acts as an antagonist in breast tissue, it acts as an antagonist in the endometrium thus there is an increased risk of endometrial cancer.
There is also an Increased risk of thromboembolism. One benefit of tamoxifen is that it prevents bone loss by acting as an estrogen receptor agonist.
Q.68. A 31 year old woman presents to the emergency department with a lower abdominal pain and per vaginal bleeding one day after having a hysterosalpingography as a part of her infertility treatment. Her blood pressure is 85/50 mmHg and pulse rate is 125 beats/minute. On examination, the abdomen is rigid and tender. What is the most appropriate step in investigation?
Correct Answer : B
A hysterosalpingography is a type of radiographic evaluation that looks at the uterus and fallopian tubes predominantly as part of investigation for infertility. It uses a contrast material that is injected into the cervical canal that appears on real-time X-ray(fluoroscopy) to visualize the fallopian tubes to determine if the tubes are partially fully blocked.
If the fallopian tubes are patent, the contrast medium will fill the tubes and spill out into the abdominal cavity. Complications associated with a hysterosalpingogram include the possibility of an allergic reaction to the dye or infection (endometritis or salpingitis), which are common. Uterine perforation or fallopian tube perforation like in this stem are also possible complications, but these are very rare.
If a perforation were to occur, the patient may have bleeding intraabdominal and an ultrasound scan would be a good start to evaluate the severity of the bleeding.
The picture given in this stem with a low BP, rapid heart rate, abdominal rigidity, and absent rash does point towards a likely intra-abdominal bleed. In a real clinical setting, a laparoscopy or laparotomy would be a more suitable option as she is clinically unstable.
As these options are not provided, ultrasound would be the next best investigation.
Q.69. A 25 year old woman has vaginal discharge, intermenstrual bleeding and post coital bleeding. A vulvovaginal swab was taken which tested positive for Neisseria gonorrhaee. What is the most appropriate management?
Correct Answer : A
Cervicitis management If just cervicitis (Chlamydia)
• Azithromycin 1g single dose (OR doxycycline 100mg bd for 7 days) (both have similar efficacy of more than 95%). The guidelines suggest azithromycin should be used first-line due to potentially poor compliance with a 7-day course of doxycycline If just cervicitis (Neisseria gonorrhoeae)
• Azithromycin 1g PO and ceftriaxone 500mg IM. It is important to note the differences between acute PID and just cervicitis as the management is different.
Q.70. A 21 year old woman had a recent suction curettage to evacuate the contents of the uterus following a miscarriage. The histology shows changes consistent with a hydatidiform mole. What is the most appropriate advice to be given?
Correct Answer : C
Serum and urine samples of hCG concentrations are extremely important. In hydatidiform moles, hCG levels are likely to be raised excessively (especially in incomplete moles). Management would involve surgical evacuation, after which the hCG levels are expected to return to a normal, non-pregnant level. We would like the hCG to go down towards a normal level but If it plateaued or if hCG levels rise after evacuation, chemotherapy is indicated.
This is the reason it is so important not to get pregnant during the time that hCG levels are decreasing if one were to get pregnant, hCG levels would increase again and we would not know if it is due to the hydatidiform mole or the new pregnancy.
The best advice to give is to use barrier contraception until serum hCG is normal and follow-up is complete. Fortunately, women who have a molar pregnancy are enrolled in a national follow-up program where they can have repeated hCG measurements. For example, follow-up for molar pregnancies.
The previous guidance for oral contraception use was to use only once hCG levels have normalized.
However, the advice is now changing and the latest advice is that oral contraception has no role in increasing the risk of invasive mole or choriocarcinoma from developing hence oral contraception may be used after molar evacuation, before hCG returns to normal values.
Q.71. A 30 year old lady presents to the outpatient clinic with difficulty in conceiving for the past 2 years. She and her husband have been trying to achieve pregnancy for more than 2 years and have been unsuccessful. There is no previous history of pelvic inflammatory disease. She has a BMI of 23. She has a regular 32 day menstrual cycle. What is the most appropriate test to perform to assess ovulation?
Correct Answer : A
Serum progesterone (Mid-luteal cycle progesterone) is tested one week before a menstrual period is expected. For example, on day 21 of a 28-day menstrual cycle.
In this case, since she has regular 32-day menstrual cycles, the serum progesterone should be taken on day 25 (32 days - 7 days = day 25). A serum progesterone of more than 30 nmol/L is consistent with ovulation and no further biochemical assessment is required.
As part of the management of infertility, FSH and LH are usually taken in clinics.
However in this context, since her menses are regular, it is less important. It is usually measured if there is menstrual irregularity to help exclude conditions like premature ovarian insufficiency (LH and FSH both raised), polycystic ovarian syndrome (LH: FSH ratio increased), and hypogonadotropic hypogonadism (LH and FSH reduced).
Q.72. A 24 year old lady has lower abdominal pain worsening over the last 2 days. She has vaginal discharge and also complains of deep dyspareunia. A urine HCG is negative. Cervical motion tenderness was noted when doing a pelvic examination. She has a temperature of 38.0 C. Her blood tests show: White cell count 14 x 109/L CRP 50 mg/L She has no significant past medical history. What is the most appropriate antibiotic treatment?
Correct Answer : D
Please see Q-65
Q.73. A 32 year old rhesus negative woman whose previous pregnancy was complicated by recurrent antepartum haemorrhage. At booking she was found to have anti-D antibodies and was referred for obstetric-led care. An ultrasound scan 1 week ago showed normal growth of the fetus. She now presents with reduced fetal movements at 33 weeks gestation. A CTG is normal. What is the most appropriate investigation?
Correct Answer : C
This woman has developed anti-D immunoglobulins (Rhesus isoimmunisation) as a result of recurrent antepartum haemorrhages in a previous pregnancy. The fetus is at risk of these antibodies crossing the placenta, leading to fetal anaemia and hydrops fetalis. Assessing the fetal middle cerebral artery on ultrasound allows estimation of fetal haemoglobin concentrations and therefore the severity of fetal anaemia.
This is usually performed in rhesus-negative women following rhesus is immunized in a previous pregnancy.
Fetal cord blood sampling is an option to directly quantify fetal haemoglobin concentration but is only indicated if the peak systolic velocity (PSV) of the middle cerebral artery (MCA) is abnormal.
A Kleihauer-Betke test is used to confirm and quantify a maternal-fetal haemorrhage in the prevention of Rhesus isoimmunization. It has no role in women who are already sensitized.
Q.74. A 55 year old woman presents with dysuria, frequency and urinary incontinence. She complains of dyspareunia. Urine culture has been done and is sterile. What is the most appropriate course of action?
Correct Answer : A
One of the many causes of dyspareunia is atrophic vaginitis (vaginal atrophy). Oestrogen deficiency after menopause causes atrophic changes within the urogenital tract and is associated with urinary symptoms, such as frequency, urgency, nocturia, incontinence, and recurrent infection.
These symptoms may coexist with those of vaginal atrophy, including dyspareunia, itching, burning, and dryness. Intravaginal oestrogens are the treatment choice for vaginal atrophy.
Alongside helping with the vaginal dryness, it can help with symptoms of urgency, urge incontinence, frequency, and nocturia. Note as the symptoms are local (in the vagina), you would not prescribe a systemic hormone like oral oestrogen or HRT.
Q.75. A 24 year old woman has right iliac fossa pain and vaginal spotting. Her last menstrual period was 8 weeks ago. She is pyrexial. A bimanual examination reveals cervical excitation. What is the most likely diagnosis?
Correct Answer : A
Salpingitis, endometriosis, ovarian torsions, and ovarian tumours are not associated with amenorrhoea. Patients' pelvic pain and vaginal bleeding with peritonism and cervical excitation point towards ectopic pregnancy.
Q.76. A 38 year old woman requires long term contraception. She has 3 healthy children and does not wish to have any more children in the near future. Upon examination, she is found to have extensive fibroids which are distorting her uterine cavity. She says she has difficulty in remembering to take pills. What is the best contraception for her?
Correct Answer : B
The key to choosing the correct answer here is to take into account firstly the fact that this woman has fibroids which are distorting her uterine cavity and the fact that any type of pill is not an option. Depo-Provera, even though a viable option, isn’t the correct option for this stem.
Depo-Provera has a dosing interval of 13-16 weeks which is a pretty long time, but out of all the options is not the longest time.
An Intra-Uterine System (Mirena) which is the favorite of is not the choice here because insertion of an intra-uterine device would be difficult due to the fibroid uterus that is distorting the uterine cavity.
The use of an intra-uterine system (Mirena) is contraindicated in women with congenital or acquired uterine anomalies, including fibroids if they distort the uterine cavity.
In fact and in clinical practice, having a large fibroid that distorts the uterine cavity is NOT a contraindication for insertion of a Mirena coil. Gynaecologist still use mirena coils for patients with large fibroids that distort the cavity.
While it is true that the risk of expulsion of a Mirena coil is greater if the fibroid is large, there is no reason why it cannot first be tried. However, for the exam, since the prescribing leaflet does mention that it is contraindicated if fibroids distort the uterine cavity, please do not choose the Mirena coil as the answer. NexplBatman is the only contraceptive implant.
NexplBatman is a 4 cm flexible rod containing 68 mg etonogestrel (a progestogen) which is released slowly into the systemic circulation following subdermal insertion in the upper arm. It must be removed after three years when it can be replaced immediately.
Progestogen-only subdermal implants (POSDIs) such as NexplBatman are suitable for:
• Those who want a reliable but reversible form of contraception that does not require daily vigilance or action at the time of intercourse.
• Women who have contra-indications to oestrogen therapy.
Q.77. A 39 year old woman has had no menstrual periods for the last 11 months. Prior that she had regular menstrual cycles. She recently has had hot flashes and night sweats. She is also experiencing feelings of anger and helplessnes. FSH was done and it was raised on two separate occasions. What is the most appropriate management?
Correct Answer : C
Hormone replacement therapy is an important part of management for women with premature ovarian failure to reduce the risk of osteoporosis, and cardiovascular disease and maintain sexual health and quality of life. This should be continued until the average age of menopause which is 51.
Q.78. A 21 year old woman comes to your clinic with the complaint of per vaginal spotting. This has occurred 3 times in the last week. She was commenced three weeks ago on the combined oral contraceptive pill. Upon further questioning, she says that she has been taking the pill regularly and a pregnancy test has been shown to be negative. She also gives no history of pain, dyspareunia, abnormal vaginal discharge or postcoital bleeding. She is in a long term, stable relationship. What is the best management for this patient?
Correct Answer : A
Irregular bleeding whilst taking hormonal contraception is a common problem. A small percentage of women may also experience breakthrough bleeding or spotting however, the bleeding usually settles with time, and it is therefore recommended that women preserve for three months before considering changing their method of contraception.
Q.79. A 29 year old primigravida at 36 weeks gestation is found to have a blood pressure of 150/100 mmHg on routine check-up. Her booking blood pressure was 120/80 mmHg. She was brought to the obstetric unit where her blood pressure was repeated twice and was found to be 150/105 mmHg and 158/110 mmHg. A urinalysis shows 2+ protein. She is not experiencing any symptoms and feels well. What is the best management for her?
Correct Answer : C
Labetalol is the most studied antihypertensive in pregnancy with the safest profile. Although this woman has pre-eclampsia and would benefit from magnesium sulphate to prevent seizures, you must first stabilize her blood pressure to prevent intracerebral bleeding.
According to current guidelines IV magnesium sulphate is administered for:
• Women in a critical care setting who have severe hypertension or severe preeclampsia who have or previously had an eclamptic fit.
• Women with severe preeclampsia who are in a critical care setting if birth is planned within 24 hours.
PRE-ECLAMPSIA : Pre-eclampsia is a condition seen after 20 weeks gestation characterized by pregnancy-induced hypertension in association with proteinuria (> 0.3g / 24 hours). Oedema used to be the third element of the classic triad but is now often not included in the definition as it is not specific.
Risk factors :
• Pre-existing hypertensive disease in pregnancy
• Type 1 or 2 diabetes
• Chronic kidney disease
• Chronic hypertension
• Autoimmune disease (e.g. systemic lupus erythematosus or antiphospholipid syndrome)
• > 40 years old or teenager
• Family history (mother or sister)
• Obesity
• Multiple pregnancy
• Pregnancy interval more than 10 years
Symptoms :
• Headache
• Visual disturbance (flashing lights)
• Epigastric or right upper quadrant (RUQ) pain
• Rapid oedema (especially on the face)
Note: Symptoms usually occur only with severe disease
Signs :
• Hypertension (>140/90; severe if >/=160/110)
• Proteinuria (>300 mg in 24 hours)
• Hyperreflexia
Management :
• Guidelines recommend treating blood pressure > 150/100 mmHg although many clinicians have a lower threshold.
• Oral labetalol is now first-line following the 2010 guidelines. Nifedipine and hydralazine would also be an option has them in the question.
• Cure is delivery of placenta. Thus the definitive management is to deliver the baby. Unfortunately this needs to be balanced out with gestation as we would not want to deliver a baby too prematurely.
Q.80. A 42 year old complains of heavy blood loss per vaginum. An ultrasound shows uterine thickness of more than 12 mm. There were no polyps or benign lesions seen on hysteroscopy. Histology reveals the diagnosis of simple endometrial hyperplasia without atypia. She has two children and is not currently planning for another child. What is the most appropriate management for her?
Correct Answer : D
Endometrial hyperplasia is a premalignant condition, that can predispose to, or be associated with, endometrial carcinoma. It is characterized by the overgrowth of endometrial cells and is caused by excess unopposed oestrogens, either endogenous or exogenous, similar to endometrial cancer, with which it shares a common aetiology.
Presentation :
• Usually presents clinically as abnormal vaginal bleeding (intermenstrual, polymenorrhoea or postmenopausal)
• It is most commonly diagnosed in women over 40 years old with irregular menstruations or in those with post-menopausal bleeding.
Investigation:
• Transvaginal ultrasound (TVUS) is an appropriate first-line procedure. In general, the thicker the endometrium seen on ultrasound, the higher the likelihood of important pathology, ie endometrial cancer, being present.
• Endometrial sampling or formal endometrial curettage is necessary for diagnosis.
Management of endometrial hyperplasia (no atypia) : It largely depends on the age of the patient, histology, symptoms, and desire for retaining fertility.
Both continuous oral progestogens and levonorgestrel-releasing intrauterine systems are effective in achieving regression of endometrial hyperplasia without atypia. However, the Royal College of Obstetrics and Gynaecology states that levonorgestrel-releasing intrauterine system should be the first-line medical treatment because compared with oral progestogens it has a higher disease regression rate with a more favorable bleeding profile and it is associated with fewer adverse effects.
Q.81. A 30 year old 34 weeks of gestation primiparous woman attends the GP surgery for her routine antenatal clinic appointment. She feels well herself with no complaints other than slight swelling of her feet. She is happy with baby movements and the fetal heart is heard using a handheld doppler. She has a blood pressure of 148/95 mmHg and her urinalysis shows 3+ protein. Her blood pressure was repeated again in clinic and was 143/93. Her booking blood pressure was 130/80 mmHg. What is the most appropriate action?
Correct Answer : D
She is classified as a person with a new onset of hypertension (mild pre-eclampsia in this case since there is proteinuria). In pregnancy, we treat this very seriously. She should be asked to see the obstetric team on the same day for further assessment, blood test and to further quantify protein in the urine.
If her blood test comes back at an acceptable level and she is asymptomatic, she would be advised to take blood pressure measurements at least four times a day at home and to come back if the blood pressure is higher than 150/100 as this figure is the cut off where we would start antihypertensive treatment (usually oral labetalol if in an outpatient setting).
Q.82. A 32 year old woman was induced at 41+2 weeks gestation. She had a long labour which lasted 24 hours. The uterus is still palpable above the umbilicus after an hour from delivering the placenta. What is the most likely cause for her postpartum haemorrhage?
Correct Answer : A
Uterine Atony is the most common cause of excessive postpartum bleeding.
Risk Factors for uterine atony include:
• Rapid or protracted labour (most common)
• Chorioamnionitis
• Overdistended uterus e.g. Macrosomic baby
Clinical Findings : A soft uterus is palpable above the umbilicus.
Management : Uterine massage and uterotonic agents ( e.g., oxytocin)
Q.83. A 23 year old woman comes to the A&E with severe abdominal pain. Her blood pressure is 120/85 mmHg and temperature is 38.9 C. The abdomen is rigid. Cervical excitation is noticed during a vaginal examination. She gave a past history of pelvic inflammatory disease 3 years ago which was successfully treated with antibiotics. What is the most appropriate investigation?
Correct Answer : B
The possible diagnosis here is a pelvic abscess or tubo-ovarian abscess which are complications of PID. A high vaginal swab or endocervical swab can take days to return with results. As this is an A&E case, an ultrasound would be more appropriate as this would lead to a diagnosis.
Ultrasound scan is the diagnostic imaging method of choice for acute pelvic pain in gynaecology. It can easily diagnose sequelae of PID (including pyosalpinx and tuboovarianabscess). Note that even if no PID history was given in this question, an ultrasound scan would still be the most appropriate as it would rule out ovarian cysts or adnexal torsion.
Q.84. A 24 year old lady presents with lower abdominal pain for the last 3 months, dysuria, dyspareunia and vaginal discharge. Urine HCG is negative. She has no significant past medical history. What is the most appropriate next step in management?
Correct Answer : C
Women of her age group (< 25 years old) are at greater risk for pelvic inflammatory disease as they are more sexually active during this period. An endocervical swab is the first test to do to help diagnose PID.
Q.85. A 25 year old woman is concerned about cervical cancer as her mother was recently diagnosed with cervical cancer. She is sexually active and would like to know which method of contraception would decrease the risk of cervical cancer?
Correct Answer : B
Condoms reduce the risk of HPV infections and hence reduce the risk of developing cervical cancer.
Q.86. A 27 year old lady has had an uncomplicated pregnancy so far. She is now 40 weeks gestation. She came to the hospital 2 hours ago after her waters broke. She has regular and painful uterine contractions. PV examination reveals a 4 cm dilated cervix. Her vital signs are normal. What stage of labour is she in?
Correct Answer : C
Please see Q- 50
Q.87. A 33 year old woman who is 11 weeks gestation attends her booking appointment with questions regarding vaccinations in pregnancy. What vaccines are offered to women who are pregnant?
Correct Answer : B
There are two vaccines that are specifically recommended for pregnant women: the flu (influenza) vaccine and whooping cough (pertussis) vaccine. For whooping cough, the best time to get vaccinated is between 20 weeks and 32 weeks gestation.
This maximizes protection for the baby through antibody transfer.
Note that there is no whooping cough-only (pertussis) vaccine. The vaccine is usually combined with polio, diphtheria, and tetanus.
Q.88. A 23 year old woman presents with offensive vaginal discharge. A vaginal pH was taken and reads 5.6. What is the most likely causative organism?
Correct Answer : D
Please see Q-16
Q.89. A 34 year old primigravida cocaine user who is 30 weeks pregnant presents to the labor ward with a history of constant abdominal pain for the last 8 hours. She gives a history of having had lost a cupful of fresh blood per vagina before the pain started. She has not felt any movements since the pain started. She has a tender lower abdomen on examination. She has a pulse rate of 105 beats/minute. Fetal heart is unfortunately not seen on the ultrasound scan. What is the most likely diagnosis?
Correct Answer : D
The absence of a fetal heart seen on an ultrasound suggests intrauterine death which could be a complication of most of the given options however the presentation of bleeding and constant abdominal pain indicates placental abruption.
There are no signs and features suggestive of preeclampsia.
Cocaine use in pregnancy is one of the risk factors for placental abruption.
A point worth remembering as it is commonly asked. It is extremely rare for a primigravid woman to have a ruptured uterus in the absence of any previous uterine scar. The stem would usually include past histories of caesarean sections or myomectomies for the question writers would want you to pick uterine rupture as the answer.
Q.90. A 49 year old woman who is a heavy smoker is worried of ovarian cancer because her mother died of ovarian cancer. She has been on hormone replacement therapy. She used to take combined oral contraceptive pills for a few years during her twenties. She underwent menopause when she was 46 years old. What is the most relevant factor for ovarian cancer in her case?
Correct Answer : A
Please see Q-58
Q.91. A 31 year old woman who had a normal delivery 4 weeks ago is complaining for feeling tired. A full blood count was taken and results show: Hb 9.3 g/dL MCV 79 fL What is the most appropriate management?
Correct Answer : C
Iron deficiency anaemia is very common in pregnancy. The values of anaemia differ in pregnancy as compared to a nonpregnant woman .
Anaemia in pregnancy is defined as the following values Hb levels of: <11.0g/dl in the first trimester <10.5 g/dl in the second and third trimesters <10.0 g/dl in the postpartum period.
Since her Hb level is below 10 g/dL, she should be on oral iron.
Q.92. A 23 year old woman presents with offensive, homogenous grey-white vaginal discharge. Clue cells are demonstrated on a saline smear. What is the most likely diagnosis?
Correct Answer : D
Please see Q-16
Q.93. A 24 year old woman who is 15 weeks pregnant presents with pain in her lower abdomen for the past couple of hours. She has some vaginal spotting. On examination, abdomen is tender, and cervical os is closed. A tansvaginal ultrasound scan shows no fetal heartbeat or fetal activity. What is the most likely diagnosis?
Correct Answer : B
It is important to note that missed miscarriage may present with heavy vaginal bleeding or none at all. But if there is no fetal heart seen, at this stage of pregnancy, it is a missed miscarriage.
Note that in normal pregnancy the fetal heart is seen usually at 6 weeks. So you should not be diagnosing a missed miscarriage if a 4-week pregnant lady has no fetal heartbeat seen on a transvaginal ultrasound.
There are more specific ultrasound criteria to diagnose missed miscarriage but are beyond what will be asked in the exam.
Q.94. A 33 year old woman has vaginal spotting 2 days ago that is painless. She is worried of cervical cancer. She is currently on combined oral contraceptives and had a cervical smear last year which was reported as normal. Her last menstrual period was 14 days ago. Cervical ectropion is diagnosed on examination. There was no bleeding from the cervix on touch. What is the most appropriate next step?
Correct Answer : C
There is no screening test needed for cervical ectropion as cervical ectropion is not linked to the development of cervical cancer or any other condition that causes cancer. Treatment can be offered if the cervical ectropion is causing problems such as bleeding or pain during or after sex.
However, in this case, the cervix is not bleeding on touch thus no treatment is needed.
.Remember: An asymptomatic cervical ectropion should be left alone.
Cervical ectropion : This occurs when the columnar epithelium of the endocervix is displayed beyond the os. The stratified squamous epithelium that normally lines the vaginal part of the cervix (ectocervix) is replaced by columnar epithelium, which has migrated from the endocervix.
• The cervix enlarges under the influence of oestrogen and as a result, the endocervical canal is everted. Exposure to high levels of oestrogen usually occurs at certain times (e.g. puberty, in pregnancy or women on COCP).
• It is seen on examination as a red ring around the os and is so common as to be regarded as normal.
• It is generally an asymptomatic condition but patients occasionally present with bleeding or excessive discharge.
• The discharge if present is usually clear, watery in consistency and without odour.
• Once a normal cervical smear has been confirmed, it is actively managed only if there are symptoms.
• After stopping any oestrogen-containing contraceptive, treatment options include diathermy or cryotherapy.
CERVICAL ECTROPION : Cervical ectropion occurs when the columnar epithelium of the endocervix is displayed beyond the cervical os.
The stratified squamous epithelium that usually lines the vaginal part of the cervix (ectocervix) is replaced by columnar epithelium, which has migrated from the endocervix. Cervical ectropion – red ring around the os. The cervix enlarges under the influence of estrogen, and as a result, extends the endocervical canal. Exposure to high levels of oestrogen usually is seen in pregnant women on COCP.
It is usually asymptomatic however women occasionally present with post-coital bleeding or excessive non-purulent discharge.It is managed if symptoms are bothersome. Treatments include cautery with silver nitrate, diathermy, and cryotherapy.
That being said, it is essential to obtain a cervical smear and ensure it is normal prior to any treatments.
Q.95. A 28 year old primiparous woman, with no previous history of infection with herpes zoster, is 18 weeks pregnant. She had significant contact with a young girl with widespread chicken pox 8 days ago. Serum stored from an antenatal booking blood sample was sent for serology and came back negative for VZV IgG. She has no rash at present. What is the most appropriate management?
Correct Answer : A
The incubation period between exposure and the first skin lesions is around 10 to 14 days but can be as long as 21 days. She was only exposed 8 days ago. The best management here is to administer varicella-zoster immunoglobulin (VZIG) as it is effective when administered up to 10 days after contact. Chickenpox exposure in pregnancy. Chickenpox is caused by primary infection with varicella-zoster virus.
Shingles are the reactivation of dormant viruses in dorsal root ganglion. In pregnancy, there is a risk to the mother and also the fetus, a syndrome now termed fetal varicella syndrome.
Fetal varicella syndrome (FVS) :
• Features of FVS include skin scarring, eye defects (microphthalmia), limb hypoplasia, microcephaly, and learning disabilities. Other risks to the fetus shingles in infancy: 1-2% risk if maternal exposure in the second or third-trimester severe neonatal varicella: if the mother develops rash between 5 days before and 2 days after birth there is a risk of neonatal varicella, which may be fatal to the newborn child in around 20% of cases.
Management of chickenpox exposure :
Exam usually would test your knowledge on 3 of these scenarios:
1. Who gets checked for Varicella antibodies?
If the woman’s immunity to chickenpox is unknown and if there is any doubt about previous infection, or if there is no previous history of chickenpox or shingles, serum should be tested for VZV IgG.
This can usually be performed within 24–48 hours and often within a few hours if the laboratory can access serum stored from an antenatal booking blood sample. At least 80% of women tested will have VZV IgG and can be reassured.
2. Who gets VZIG?
If the pregnant woman is not immune to VZV and has had significant exposure, she should be offered VZIG as soon as possible. VZIG is effective when given up to 10 days after contact.
Note: If the immune status of the woman is unknown, the administration of VZIG can be delayed until serology results are available.
Note: VZIG has no therapeutic benefit once chickenpox has developed and should therefore not be used in pregnant women who have developed a chickenpox rash.
3. Who gets oral aciclovir?
Oral aciclovir should be prescribed for pregnant women with chickenpox if they present within 24 hours of the onset of the rash and if they are 20+ weeks of gestation or beyond.
In summary:
1. Pregnant exposed to chicken pox - Check women’s immunity (previous infection, varicella antibodies)
2. Not immune - Administer VZIG
3. If develop chicken pox rash - Administer oral aciclovir.
Q.96. A 22 year old woman is brought into the Emergency Department by her husband with severe abdominal cramping. Her abdomen is very tender. Serum beta human chorionic gonadotrophin (hCG) was measured at 1400 IU/litre. A transvaginal ultrasound reveals an empty uterine cavity with a small right adnexal mass measuring 20 mm and free fluid in the pelvis. No fetal heart activity was noted. Her systolic blood pressure was 110 mmHg on admission but has dropped to 80 mmHg an hour later. Intravenous fluids have been prescribed. What is the most appropriate next course of action? (A serum hCG above 25 IU/litre is considered positive for pregnancy)
Correct Answer : C
It is clear here that she has an ectopic pregnancy. Laparotomy would be the choice here as she is haemodynamically unstable. An open approach is quicker than a laparoscopic approach.
If she was haemodynamically stable, a laparoscopic approach to the surgical management of tubal pregnancy would be preferred as this has less post-surgical complications and reduced length of hospital stay.
Q.97. A 24 year old woman who is 18 weeks pregnant presents to the Early Pregnancy Unit with pain in her lower abdomen for the past 12 hours. She has some vaginal spotting a couple of hours ago. On examination, abdomen is tender, and cervical os is closed. An ultrasound scan shows fetal heart beat. What is the most likely diagnosis?
Correct Answer : A
Please see Q-2
Q.98. A 43 year old woman who is currently 34 weeks pregnant presents to the maternal assessment unit with headache, mild epigastric pain and slight nausea. Her symptoms started in the monring. She complains of visual disturbance which include flashing lights. A dipstick shows 2+ protein. Her heart rate is 105 beats/minute. She has a blood pressure of 158/105 mmHg and 150/90 mmHg. A CTG was connected and the trace is reassuring. What is the most appropriate initial management?
Correct Answer : C
This lady has pre-eclampsia. The first clue in this question stems from her age.
One of the risk factors of preeclampsia is an age over 40 or a teenager. Extremes of both ages. Headaches, epigastric pain, and flashing lights are all symptoms of preeclampsia and are confirmed by having protein in the urine with a BP > 140/90.
The first thing to do here is to lower the blood pressure.
Management of pregnancy with pre-eclampsia for moderate hypertension (150/100 to 159/109 mmHg) starts with oral labetalol as first-line treatment. Magnesium sulphate is important here as well however labetalol oral should be given first.
Remember, the question is asking for the most appropriate INITIAL management. Magnesium sulphate takes a while to prepare. It is an intravenous medication and usually needs consultant approval and also cardiac monitoring when giving the intravenous MgS04.
Oral labetalol does not require any of those and it is part of management as she is hypertensive in this stem.
When is magnesium sulphate the answer?
According to current guidelines IV magnesium sulphate is administered for:
• Women in a critical care setting who have severe hypertension or severe pre-eclampsia who have or previously had an eclamptic fit.
OR women with severe pre-eclampsia who are in a critical care setting if birth is planned within 24 hours.
Hospitals have their local guidelines and many do not follow the above guidance.
Q.99. A 30 year old female who has had 3 previous miscarriages, all before 10 weeks gestation. Antiphospholipid syndrome has been diagnosed. She now presents to the antenatal clinic asking if there is any treatment that she coud have that could prevent another miscarriage. What is the most appropriate management?
Correct Answer : D
The diagnosis here is antiphospholipid syndrome in which case aspirin plus heparin is indicated. As there is no option for both aspirin and heparin, pick aspirin.
Q.100. A 23 year old woman who has been using an intrauterine system (Mirena coil) for one year now complains of lower abdominal pain and menstrual irregularities. She has no significant past medical history. Which is the most likely cause of her symptoms?
Correct Answer : B
Intrauterine contraceptive devices are a risk factor for pelvic inflammatory disease. Women of her age group (<25 years old) are at greater risk for pelvic inflammatory disease as they are more sexually active during this period. Other options are less likely because: Endometriosis, adenomyosis, and fibroids. Are less likely as an intrauterine system is likely to benefit symptoms and not worsen them.
Asherman syndrome are adhesions of the endometrium often associated with dilation and curettage of the intrauterine cavity. It results in infertility. Often, they experience menstrual irregularities.
But in this question, there is no relevant past medical history meaning she did not have any dilation and curettage thus this option is improbable.
Q.101. A 30 year old woman attends clinic asking for a reversible form of contraception. Her obstetric history is significant for a previous caesarean section one year ago. She is known to have menorrhagia and dysmenorrhoea. What is the most appropriate contraceptive for her?
Correct Answer : C
A previous caesarean is not a contraindication for a levonorgestrel intra-uterine system. Among the options, the levonorgestrel intra-uterine system (Mirena coil) is the best treatment to reduce menorrhagia. It is currently the first-line treatment for menorrhagia.
Copper intrauterine contraceptive devices and ImplBatman are more prone to irregular heavy bleedings compared to levonorgestrel intra-uterine system (Mirena coil).
Q.102. A 32 year old multigravida at 32 weeks’ gestation is woken up in the middle of the night with a pool of blood. She presents to the maternity unit with bleeding that has now stopped. She has no pain or uterine contractions. Fetal heart rate is regular at 145 beats/min. Examination of the uterus shows the fetus to be in a transverse lie. She has a pulse of 120 beats/minute, a blood pressure of 110/70 mmHg and a respiratory rate of 29 breaths/minute. What is the most likely diagnosis?
Correct Answer : D
Painless vaginal bleeding is consistent with placenta praevia. Placental abruption is associated with abdominal pain. Placenta accreta and vasa praevia are less common than placenta praevia. There is no indication that she is in labour.
Q.103. A 51 year old woman presents with a 9 month history of prolonged, slightly irregular menstrual periods. On physical examination, a normal size uterus with no adnexal masses is felt. What is the most likely diagnosis?
Correct Answer : A
The average age for menopause is 51. For this question, we must go back to the definitions of menopause and perimenopause.
Menopause is the permanent cessation of menstruation. It is recognized to have occurred after 12 consecutive months of amenorrhoea for which no other obvious pathological or physiological cause is present. Peri-menopause includes the period beginning with the first clinical, biological, and endocrinological features of the approaching menopause, such as vasomotor symptoms and menstrual irregularity. As the above question presents irregular menstruation and absent menstruation for a period of 12 months, perimenopause is the correct answer.
SYMPTOMS OF MENOPAUSE: The experience of each woman varies widely -
• Some may be asymptomatic
• Some may experience symptoms while menstruating
• Some may not experience symptoms until a year or more after their last period.
Symptoms of menopause include:
• Hot flushes and night sweats (80% of women) – these are the hallmark symptoms.
• Sleep disturbance
• Menstrual irregularities
• Vaginal dryness
• Loss of libido
• Urinary problems which include recurrent lower urinary tract infections & urinary incontinence.
Q.104. A 33 year old woman has complaints of heavy menstrual bleeding and chronic pelvic pain. A transvaginal ultrasound reveals a thick walled unilocular cyst with acoustic enhancement with diffuse homogeneous ground-glass echoes located on the left ovary. What is the most likely diagnosis?
Correct Answer : C
A thick-walled cystic structure containing homogeneous ground-glass echos are ultrasound findings of an endometrioma. Ovarian endometriomas are ovarian cysts lined by endometriotic tissue.
Remember that the ground-glass appearance often describes the cyst fluid in an ovarian endometrioma. The cyst fluid is usually a thick chocolate coloured fluid which differentiates it from a simple haemorrhagic cyst.
Q.105. A 31 year old woman, gravida 5 para 4, presents to the emergency room with vaginal bleeding. She has a history of amenorrhoea for 12 weeks. Pregnancy test was done in the emergency department and it was positive. Symphyseal-fundal height measurement corresponds to 22 weeks gestation. Ultrasound of the pelvis reveals bilateral cystic masses. No fetal parts are seen during the ultrasound examination. The cervix is closed. Which is the most likely diagnosis?
Correct Answer : B
The ultrasound findings of the bilateral cystic masses represent the large theca lutein cysts. Uterus large for dates and vaginal bleeding are typical features of hydatidiform mole.
Another term worth remembering for complete molar pregnancies is the “Snowstorm” appearance of mixed echogenicity which represents hydropic villi and intrauterine haemorrhage.
Q.106. A 23 year old primigravida woman comes into the antenatal unit with painless vaginal bleeding at 37 weeks of pregnancy. She describes the bleeding amount as half a cup full. She has no uterine contractions. The fetal heart tones are regular at 140 beats/minute. On examination, abdominal palpation identifies the fetus to be in a transverse lie and the uterus is nontender. A speculum examination reveals a closed cervix with no polyps or lacerations identified. She has a pulse rate of 90 beats/minute, a blood pressure of 110/60 mmHg and a respiratory rate of 19 breaths/minute. What is the most appropriate action?
Correct Answer : D
A transverse lie at 37 weeks in a primigravid woman is the first clue that there is a mass in the way. In this case, it is the placenta. Painless vaginal bleeding is consistent with placenta praevia. Transvaginal ultrasounds are preferred for the diagnosis of placenta praevia although abdominal ultrasound scans may also be used.
Q.107. A 16 year old girl who is normally fit and healthy attends her GP complaining of very painful menstrual periods. She has a regular 28 day menstrual cycle. She denies being sexually active. What is the most appropriate management?
Correct Answer : A
Dysmenorrhoea is very common among this age group. Mefenamic acid is usually the first tried management as the pain during periods may sometimes lessen over the next couple of months to years.
Dysmenorrhoea can be divided into two:
• Primary dysmenorrhoea: the pain has no obvious cause.
• Secondary dysmenorrhoea: the pain is due to an underlying condition.
Primary dysmenorrhoea Management:
• NSAIDs such as mefenamic acid with each period is usually the first treatment.
• Combined oral contraceptive pills are used second line if the only symptom is pain.
• Mirena IUS demonstrates benefit
Secondary dysmenorrhoea common aetiology :
• Endometriosis
• Adenomyosis
• PID
• Management - Treat the underlying condition.
Q.108. A 28 year old lady presents with lower abdominal pain and increased vaginal discharge. A pregnancy test was performed and it was negative. She has a temperature of 38.5 C and also complains of deep dyspareunia. She has a pulse rate ofe 90 beats/minute. What is the most appropriate antibiotic regimen?
Correct Answer : C
OPTIONS FOR MANAGEMENT OF PID :
• IM ceftriaxone stat plus oral doxycycline and oral metronidazole for 14 days OR
• Ofloxacin and metronidazole orally for 14 days Inpatient management of PID
• IV ceftriaxone and IV doxycycline followed by oral doxycycline and oral metronidazole for 14 days OR
• IV ofloxacin and IV metronidazole for a total of 14 days.
Q.109. A 29 year old woman who is 33 weeks gestation attends the antenatal clinic. Her full blood count was taken when she was 28 weeks as part of an antenatal screen for anaemia. The results show: Haemoglobin 9.6 g/dL Mean cell volume 75 fL She is asymptomatic. What is the most appropriate management?
Correct Answer : C
The values of anaemia differ in pregnancy as compared to a non-pregnant woman.
Anaemia in pregnancy is defined as the following values - Hb levels of: <11.0g/dl in the first trimester <10.5 g/dl in the second and third trimesters <10.0 g/dl in the postpartum period. Since her Hb level is below 10.5g/dL, she does need iron tablets.
Q.110. A 35 year old woman has just discovered that she is pregnant. Her last menstrual period was 7 weeks ago. She has been on anti-epileptic medication for the past 3 years. What is the most important supplement for her to start to prevent teratogenic effects in her unborn child?
Correct Answer : A
Advise women who are at high risk of having a child with neural tube defects to take folic acid (5 mg/day) until 12 weeks of gestation to reduce the risk of having a baby with a neural tube defect. This can be started even before conception.
Women who are at high risk include:
• Diabetes
• Receiving antiepileptic medication
• Previous pregnancy with neural tube defects
• Sickle-cell disease (folic acid given throughout pregnancy)
• Thalassaemia or thalassaemia trait (folic acid given throughout pregnancy)
In addition, guidelines also recommends using 5 mg/day of folic acid for those who have:
• BMI more than 30 kg/m2
• Family history of an NTD If the woman has a low risk of conceiving a child with neural tube defects, then she should be advised to take a smaller dose of folic acid (400 mcg/day) until 12 weeks of gestation.
Q.111. A 31 year old woman has vaginal spotting after her last intercourse which was a day ago. Her last menstrual period was 10 days ago and she usually has a regular 28 day menstrual cycle. A cervical smear performed 6 months ago was shown to be normal. A speculum examination shows cervical ectropion which does not bleed on touch. What is the most appropriate action?
Correct Answer : D
There is no screening test needed for cervical ectropion as cervical ectropion is not linked to the development of cervical cancer or any other condition that causes cancer.
Treatment can be offered if the cervical ectropion is causing problems such as bleeding or pain during or after sex. However, in this case, the cervix is not bleeding on touch thus no treatment is needed.
Q.112. A 41 year old woman presents with an offensive malodorous vaginal discharge. The discharge is clear in colour and has a distinctive fishy odour. A vaginal pH was taken and found to be 5.7. What is the most likely causative organism?
Correct Answer : B
Bacterial vaginosis and Trichomonas vaginalis can give foul-smelling discharge. Bacterial vaginosis which is mostly caused by an overgrowth of Gardnerela vaginalis causes vaginal discharge which is gre-white and has a “fishy” smell.
The characteristic “fishy smell” is a clincher and one should pick Bacterial vaginosis (Gardnerella vaginalis) as the answer. In trichomonas vaginalis, it can be greenish and frothy along with vulvovaginitis i.e. strawberry cervix.
The discharge of Chlamydia and Gonorrhea is not usually foul-smelling. Candida albicans (vaginal candidiasis) has a white, ‘cheesy’ discharge. The discharge is non-offensive.
Q.113. A 33 year old woman with 2 healthy children comes to you to discuss contraceptive methods. She is fit and well. Her two children were born by vaginal deliveries. She has a stable partner and both of them do not want any further children. Which of the options below has the lowest contraceptive failure rate?
Correct Answer : C
To understand failure rates of contraception, one would need to understand the Pearl index. The Pearl index is defined as the number of pregnancies occurring per 100 women years (a woman year is defined as 13 menstrual cycles).
For example, if the Pearl index is 2 for contraception X, this means that if 100 women use contraception X for 1 year, 2 of the 100 women would end up pregnant in that year.
Q.114. A 42 year old woman complains of heavy bleeding and prolonged menstrual period. She is not planning for children at the moment as she already has 2 children. She smokes 20 cigarettes a day. What is the most appropriate management?
Correct Answer : D
Levonorgestrel intra-uterine system (Mirena) is the first-line pharmaceutical treatment for menorrhagia. Smoking is not a contraindication for use for the Mirena coil.
Q.115. A 24 year old lady has lower abdominal pain worsening over the last 7 days. She has vaginal discharge and also complains of deep dyspareunia. Her last menstrual period was 2 weeks ago. Cervical motion tenderness was noted when doing a pelvic examination. She has a temperature of 38.2 C. Her blood tests show: White cell count 15 x 109/L CRP 55 mg/L She has no significant past medical history. What is the most likely diagnosis?
Correct Answer : B
This is a very straightforward question. Her symptoms and signs all point towards pelvic inflammatory disease (PID). A raised WBC and CRP is also consistent with PID.
Q.116. A 33 year old woman has vaginal discharge and bleeding. An endocervical swab was taken which tested positive for Chlamydia. What is the most appropriate antibiotic to give?
Correct Answer : B
Please see Q-69
Q.117. A 27 year old waitress has pelvic pain, dysmenorrhoea and increasingly heavy periods over the last 9 months. The pain is worse when she is standingfor long periods of time. She also complains of dyspareunia. A pelvic ultrasound was reported as normal. A diagnostic laparoscopy was performed which did not show any abnormalities. What is the most likely diagnosis?
Correct Answer : A
In pelvic venous congestion, there are dilated pelvic veins believed to cause a cyclical dragging pain. It is worse premenstrually and after prolonged periods of standing and walking. Dyspareunia is also often present.
Non-organic dyspareunia + with symptoms similar to premenstrual syndrome + aggravated by standing = Pelvic congestion syndrome.
Pelvic congestion syndrome is a chronic medical condition in women caused by varicose veins in the lower abdomen.
The condition causes chronic pain, often manifesting as a constant dull ache, which can be aggravated by standing. It is a diagnosis of exclusion where other organic causes of dyspareunia have been excluded.
It may present as pain during intercourse that may be deep within the vagina with symptoms similar to premenstrual syndrome. It is caused by the accumulation of blood during arousal without the occurrence of orgasm. Achieving orgasm (by intercourse, masturbation, or use of a vibrator) may help to alleviate this congestion.
Q.118. A 32 year old woman presents at 39 weeks gestation of her third pregnancy. She reports having a vaginal loss of clear viscous fluids 4 days ago. She did not attend the delivery suite as she had planned for a home birth. Over the past 3 hours, she complains of feeling feverish and sweaty. Examination of the patient’s abdomen reveals tenderness suprapubically. The symphysis-fundal height is 35 cm. She has a temperature of 38.3 C. The CTG shows a baseline fetal tachycardia of 170 beats/minute for the past 30 minutes. Her blood tests show: Haemoglobin 105 g/L White cell count 19 x 109/L Platelets 250 x 109/L CRP 219. What is the most likely diagnosis?
Correct Answer : D
Prolonged rupture of membranes (PROM) is a risk factor for chorioamnionitis. Although endometritis is a possibility, this is a more common complication in the postpartum period.
Q.119. A 33 year old lady presents with clear, watery discharge. On examination, a red ring is seen around the cervical os. The diagnosis of cervical ectropion is made. What is the most accurate description to define cervical ectropion?:
Correct Answer : A
Please see Q-94
Q.120. A 53 year old woman complains of dyspareunia and vaginal dryness. On a speculum examination, an atrophic vaginitis is seen. Her last menstrual period was one year ago. What is the most appropriate management?
Correct Answer : C
Topical oestrogen is advisable as first-line for women with vaginal atrophy. A vaginal oestrogen cream or pessary would be appropriate here since the patient only had symptoms of vaginal dryness without the other symptoms of menopause like hot flushes.
If she had vasomotor symptoms such as flushing, including sleep, mood disturbance, and headaches, then a systemic hormone replacement therapy like the oestrogen plus progestogen patch would be a better pick.
Q.121. A 41 year old lady who is 37 weeks pregnant was brought to A&E. On arrival, she has a seizure. Her husband says a few hours ago she complained of headache, visual disturbance and abdominal pain. What is the most appropriate management?
Correct Answer : D
Eclampsia is defined as the occurrence of a tonic-clonic seizure in association with a diagnosis of pre-eclampsia. Eclampsia is an obstetric emergency. Every hospital should have an eclampsia protocol and eclampsia box with all the drugs for treatment.
Prevention and control of seizures:
• Magnesium sulfate should be considered when there is concern about the risk of eclampsia. It is used to prevent seizures as well as control it. • To control a seizure, a loading dose of 4 g MgSO4 in 100 ml 0.9% normal saline is given by infusion pump over 5-10 minutes. This is followed by a further infusion of 1 g/hour maintained for 24 hours after the last seizure.
• Recurrent seizures should be treated with either a further bolus of 2 g of magnesium sulfate or an increase in the infusion rate to 1.5 g or 2.0 g/hour.
Q.122. A 31 year old woman who is 32 weeks pregnant attends the antenatal clinic. Her full blood count was taken when she was 28 weeks which results show a Hb of 10.7 g/dL, MCV = 91. What is the most appropriate management?
Correct Answer : A
Explained already.
Q.123. A 33 year old woman comes to the emergency department complaining of right sided abdominal pain for the last day. She vomited once earlier today. She gives a history of missing a period. A urine pregnancy test was found to be positive. A transvaginal ultrasound scan reveals an empty uterus. On examination, she is found to be tender at the right iliac fossa with no signs of peritonism. She is afebrile and observations are stable. What is the most appropriate next step in management?
Correct Answer : C
It is clear here that she has an ectopic pregnancy. The be more specific, this is a presentation of an unruptured ectopic pregnancy. The fact that there are no signs of peritonism, no shoulder tip pain or per vaginal bleeding and observations are normal means that a ruptured ectopic is unlikely.
As she is haemodynamically stable with severe right abdominal pain, a laparoscopic approach to the surgical management of tubal pregnancy is warranted however we would need to obtain a serum beta-hCG test first.
With the results of the serum beta hCG, we would be able to plan the next step in management. If the serum beta-hCG was less than 1500 IU/litre and the patient is clinically stable with pain resolving, then we would prefer expectant management where we would just observe.
The reason behind this is that one cannot be sure of the diagnosis of an ectopic pregnancy when the serum beta-hCG is less than 1500 IU/litre as it could very well be an intrauterine pregnancy that is just too small to see on a scan at the moment. If a beta-hCG was more than 1500 IU/litre, we would expect to see a gestational sac in the uterus.
Meaning if the beta-hCG was more than 1500 IU/litre and nothing can be found in the uterus on transvaginal ultrasound, the diagnosis of an ectopic can be certain.
Laparotomy would be the choice if the patient is haemodynamically unstable. The reason for this is laparotomy is quicker than a laparoscopy. Culdocentesis was previously used to diagnose a ruptured ectopic pregnancy by the presence of free fluid in the pouch of Douglas. However, ultrasonography is noninvasive and has largely replaced culdocentesis where available.
Q.124. A 26 year old woman is now 21 days postpartum and would like contraception. She has a fear of needles and would like a contraception that is reversible as she wants to coceive again in 6 months. She is currently breast feeding. What is the most appropriate contraception?
Correct Answer : B
Intrauterine system and progestogen-only implants are not suitable for use in this woman as she would like to become pregnant in 6 months. She is afraid of needles, thus contraceptive injections such as the Depo-Provera injections are not suitable. Combined oral contraceptives should not be used in any woman less than 6 weeks postpartum.
In breastfeeding women, COCP is considered UKMEC 4 if less than 6 weeks postpartum and UKMEC 2 if between 6 weeks to 6 months postpartum. In a nonbreastfeeding woman, it is considered UKMEC 3 if less than 3 weeks postpartum and UKMEC 2 between 3 to 6 weeks postpartum.
For ease, just remember that the safest time to prescribe COCP postpartum is after 6 weeks for nonbreastfeeding mothers and after 6 months for breastfeeding mothers. There is no evidence that progestogen-only pills affect breast milk or infant growth and thus this can be started at any time.
Ideally, we should delay starting POP until 21 days postpartum as there is no use starting it before and she would not require contraception during that time.
POSTPARTUM CONTRACEPTION : Menstrual periods usually return 5 to 6 weeks after birth if the mother is not breastfeeding. If the mother is breastfeeding, the menstrual cycle usually returns once the breastfeeding is less often. It is important to remember that, women can become pregnant BEFORE their periods return because ovulation occurs prior to menstrual bleeds.
For women who are not breastfeeding, it is reasonable to start using contraception from 3 weeks (21 days) after birth. Remember, no contraception is needed until 21 days postpartum.
Summary of postpartum contraception :
• Breastfeeding mothers – COCP after 6 months
• Nonbreastfeeding mothers – COCP after 6 weeks
• In both cases, during the period before they can start using COCP, they can use condoms or progesterone-only preparations.
Women should be advised that although contraception is not required in the first 21 days after childbirth, POP can be safely initiated immediately. There is usually no need for any contraception use until day 21 postpartum as ovulation can only take place on day 28 and sperms can only survive 7 days.
• IUS/IUCD unless fitted within 48 hours of birth, delay until after 28 days postpartum (delay until 28 days as if inserted before may risk uterine perforation)
Q.125. A 24 year old woman has a 5 month history of vaginal discharge, intermenstrual bleeding and post coital bleeding. She is sexually active and does not use any form of contraception. What is the most appropriate investigation?
Correct Answer : C
The likely diagnosis here is cervicitis caused by either chlamydia or Neisseria gonorrhoeae. The endocervix is the principal site to be tested. Swabs of the endocervix can be taken during a speculum examination or indirectly by a vulvovaginal swab. These samples are suitable to be sent for nucleic acid amplification tests (NAATs), cultures, or microscopy. A high vaginal swab (HVS) is only worthwhile where there are recurrent symptoms, treatment failure, or in pregnancy, postpartum, post-abortion, or post-instrumentation.
Cervical cytology is a useful tool to screen for cervical cancers however it is a screening tool for asymptomatic patients. There is no role for cervical smears for symptomatic patients. Furthermore, cervical screening starts at age 25. Cervical cancer is extremely rare under 25 years of age.
CERVICITIS (CHLAMYDIA AND NEISSERIA GONORRHOEAE) DIAGNOSIS
• Usually asymptomatic
• Can present with vaginal discharge, low abdominal pain, intermenstrual bleeding, or postcoital bleeding.
Diagnosis :
• Endocervical or vulvovaginal swab with NAAT, culture, or microscopy. Screening asymptomatic heterosexual patients for gonorrhoea involves using NAAT. A first-pass urine is collected for males and a vulvovaginal swab (which may be self-taken) is collected for females.
If NAAT results show positive for gonorrhoea, a culture needs to be sent prior to starting antibiotics if possible. This is to test for susceptibility and resistant strains.
Diagnosis in detail :
• Endocervical swab in transport medium (charcoal preferably) is to diagnose gonorrhoea.
• Endocervical swab for a chlamydia nucleic acid amplification test (NAAT) is to diagnose chlamydia.
• If examination is declined, a self-taken vulvovaginal swab for C. trachomatis and N. gonorrhoeae for NAAT may be an option and is more sensitive in women than urine testing.
Q.126. A 34 year old African woman has been trying to conceive for the past 2 years. She has suffered from heavy menstruations for the past 3 years and a recent transvaginal ultrasound shows two large submucosal fibroids and one intramural fibroid. Her partner has had a sperm analysis which was found to be normal. What is the most appropriate management?
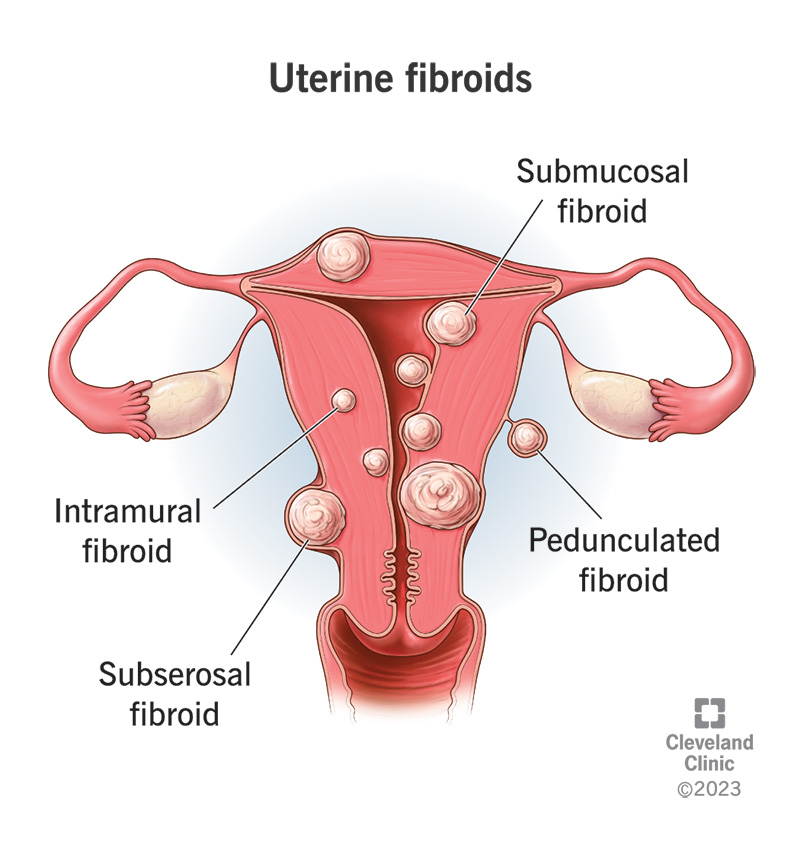
Correct Answer : D
This woman is trying to conceive. The only option to preserve fertility here is a myomectomy.Endometrial ablation is a very good option to decrease menorrhagia however the procedure involves using electrical currents or heated water to destroy the endometrium which could result in infertility.
This procedure is therefore NOT recommended for women who still want children. It is also important to note that endometrial ablation is not used in patients with large fibroids. It is primarily used in patients with heavy menstrualbleeding due to endometrial hyperplasia without fibroids, but it can also be used to treat small submucosal fibroids.
Uterine artery embolization (UAE) is an alternative procedure to a hysterectomy or myomectomy for treating fibroids. It is performed by a radiologist and involves embolizing the uterine arteries to shrink the fibroids.
It is recommended for women with large fibroids however it is not recommended if the woman is trying to conceive as it reduces blood to the uterus significantly.The levonorgestrel intrauterine system (LNG-IUS) is a small, plastic, t-shaped device placed in your uterus that slowly releases progestogen. It also acts as a contraceptive and thus should not be used for a woman trying to conceive. GnRH analogues essentially shrink the fibroids however they would grow back once the medication is stopped. Its primary use is so that it is easier to remove the fibroids during surgery. As GnRH analogues inhibit ovulation, it would prevent pregnancy from occurring. This would be a suitable option given that it was combined with a myomectomy.
It is also important to note that if she does decide to go for a myomectomy, she would need to be counseled on the risk of uterine rupture in the future if she becomes pregnant, especially during labour. Her obstetrician would need to weigh the risks and benefits of normal delivery and consider a cesarean section due to the risk of a uterine rupture.
FIBROID LOCATIONS :
Submucosal fibroids - Are located beneath the endometrium and bulge into the uterine cavity
Intramural fibroids - Are located within the muscular uterine wall
Most common type of fibroid : Subserosal fibroids - Located on the external surface of the uterus and projected to the outside of the uterus.
Q.127. A 27 year old woman has pre-eclampsia and was delivered by C-section. She is now complaining of right upper quadrant pain. What is the most appropriate immediate investigation?
Correct Answer : C
This lady has pre-eclampsia and now has RUQ pain. This could be a potential HELLP syndrome. A liver function test would help us with the diagnosis.
Q.128. An 11 week pregnant woman presents with severe persistent vomiting and nausea. She has been feeling nauseous for the past few days. A urinalysis shows 2+ ketones. She has a pulse rate of 100 beats/minute. What is the most appropriate action?
Correct Answer : B
This is a case of hyperemesis gravidarum.
Intravenous fluids are the most important part of management to ensure that the patient is not dehydrated. As this has already been given and dehydration managed, intravenous antiemetics is the next best answer since only intramuscular cyclizine has been given.
Regular antiemetics such as promethazine or cyclizine are often tried first in many early pregnancy units. If this fails, prochlorperazine intramuscularly or orally can be added on. If the patient continues to vomit, intravenous metoclopramide or ondansetron can be used on top of the already prescribed regular antiemetics. Advice such as to eat little and often should be given.
Thiamine is also used in hyperemesis gravidarum and should ideally be given to all women admitted with prolonged vomiting. This is to prevent Wernicke’s encephalopathy which is due to vitamin B1 (thiamine) deficiency. However, the importance of thiamine in an acutely vomiting woman is less compared to having intravenous antiemetics.
HYPEREMESIS GRAVIDARUM : Nausea and vomiting are common in early pregnancy. When it is severe or prolonged it is called hyperemesis gravidarum.
Symptoms usually begin between 6-8 weeks; peaks at 12 weeks and usually resolve by 20 weeks.
Symptoms :
• Nausea
• Vomiting
• Food and fluid intolerance
• Lethargy
Signs -
• Ketonuria
• Weight loss > 5%
• Tachycardia
• Signs of dehydration: Decreased skin turgor , Prolonged capillary refill, Sunken eyes
Management :
• IV fluids : If potassium is found to be low i.e. < 3.5 mmol, sodium chloride 0.9% with 20:40 mmol/litre potassium chloride (KCl) is usually added.
• Antiemetics : 1st line- Promethazine, Cyclizine, Prochlorperazine, Chlorpromazine. 2nd line - Metoclopramide & Ondansetron. 3rd line - Corticosteroids.
Q.129. A 22 year old pregnant woman is admitted at 37 weeks gestation with a blood pressure of 165/95 mmHg and symptoms of visual disturbances and epigastric pain. A few hours after administration of IV magnesium sulphate and IV labetalol, she develops a fit. What is the most appropriate IV therapy to prevent further fits?
Correct Answer : B
Please see Q-121
Q.130. A 23 year old woman who is 28 weeks pregnant presnts with vaginal bleeding. She has lost about 200 ml of blood vaginally. On examination, she has a soft abdomen, but has lower abdominal tenderness. A full blood count and a group and hold has been taken. Intravenous fluids has been started. Her observations are currently stable. What is the most important investigations to establish a diagnosis?
Correct Answer : A
Antepartum haemorrhage is seen here. Two of the most common causes are placental abruption and placenta praevia. Other causes include local causes like bleeding from the vulva, vagina, or cervix (cervical polyp or cervical carcinoma).
It is not uncommon to fail to identify a cause for APH (over 30% of APH are of unknown origin). The most important investigation is an ultrasound. This helps us rule out causes such as placenta praevia if the placenta is seen to be high.
Usually, pregnant women would have had a scan at 20 weeks which would show the location of the placenta. Note that placenta praevia is usually painless bleeding.
Placenta abruption is a clinical diagnosis and should be considered if the pain is continuous. The abdominal pain usually has a sudden onset. Vasa praevia would also be in the differential as it is another cause of painless bleeding vaginally.
Kleihauer is an important test to perform for any woman with a significant antepartum haemorrhage who is rhesus negative. It is a blood test used to measure the amount of fetal haemoglobin transferred from a fetus to a mother’s bloodstream.
Note however that this question is asking about investigations that would lead to a diagnosis. The Kleihauer test will not provide any input for a differential.
It is merely a test to determine the required dose of anti-D immunoglobulins to inhibit the formation of Rh antibodies in a Rh-negative mother to prevent Rh disease in future pregnancies with a Rhesus-positive fetus.
It is worth mentioning that if the question was asking for the SINGLE best action and a CTG was within one of the options, that would usually be the best action.
The reason behind this is placenta abruption is part of the differential and if the CTG shows fetal distress, the baby would need to be delivered immediately. There is no time to wait around for an ultrasound. with a Rhesus-positive fetus.
Q.131. A 35 year old female presents to the gynaecology clinic for investigations of infertility. She has menstrual cycle which she counted as being 35 days. She is on long term medications. She demonstrates enthusiasm about her job as a journalist and claims that she is experiencing no stress at home or at work. She drinks alcohol socially and smokes around 10 cigarettes a day. A blood sample was taken from the patient and her results are as follows: Follicle-stimulating hormone (FSH) 5 U/L Luteinizing hormone (LH) 3 U/L Prolactin 300 mU/L Oestradiol 800 pmol/L 21 day Progresterone 10 ng/dL. What is the most likely reason for the results above?
Correct Answer : D
Before you go any further, remember that progesterone should be taken 7 days prior to her menstrual bleeding. This woman has a 35-day menstrual cycle. For her hormone levels to be accurately interpreted, we would need to take a blood sample from her on day 28 of her menstrual cycle.
This is equivalent to day 21 of a standard 28-day menstrual cycle.
To get the best day to measure progesterone levels you take (total length of the cycle) – 7 days. For example, in this patient, it would be 35 (her total cycle length) – 7 days = 28.
The progesterone levels are low because it is not taken on the appropriate day.
Premature ovarian failure would have persistently elevated FSH and LH levels. Polycystic ovary syndrome would usually have elevated levels of LH.
Q.132. A 66 year old woman had two episodes of post-coital vaginal bleeding in the last week. She has not had any withdrawal bleeds for more than 12 years. Her last cervical smear was 3 years ago which showed no abnormalities. What is the most appropriate initial action?
Correct Answer : A
The idea here is to think of endometrial cancer. Any woman who has postmenopausal bleeding should have a transvaginal ultrasound to determine the endometrial thickness. If the endometrium is thick, a hysteroscopy with endometrial biopsy would be arranged.
The hormone replacement therapy in this scenario has no relevance as HRT (progesterone and oestrogen) is not a risk factor for endometrial cancer.
Only unopposed oestrogen would be a risk factor for endometrial cancer.
A cervical smear is offered every 5 years if in the age group of 50 to 64 years old. Thus, having a cervical smear that was normal 3 years ago is a usual phenomenon. A repeat cervical smear is not necessary.
Q.133. A 33 year old 39 weeks pregnant nulliparous woman with a previous history of gestataional hypertension is in labour. Her membranes had ruptured earlier in the day. She was assessed by the midwife and her cervix was found to be soft, mid-position with an os 3 cm dilated. The fetus is in cephalic position. A vaginal examination was performed 4 hours later and the cervical os still remains at 3 cm dilated. Cardiotocography is reassuring and she is contracting less than three times in 10 minutes. What is the most appropriate action?
Correct Answer : B
There is an obvious delay in the first stage of labour since there has been no cervical change over the last 4 hours. Amniotomy, oxytocin infusion and reassessment in 2 hours should always be considered in nulliparous women.
Since her waters have already been broken. It would be appropriate to start oxytocin (syntocinon).
Some causes of poor progress in the 1st stage :
• Inefficient uterine activity ( power - commonest cause)
• Malposition, malpresentation, or large baby (passenger)
• Inadequate pelvis (passage). Oxytocin will increase the frequency and strength of her contractions.
Q.134. A 23 year old woman has vaginal discharge and bleeding. An endocervical swab was taken which tested positive for Chlamydia. What is the most appropriate antibiotic to give?
Correct Answer : D
Please see Q-69
Q.135. A 39 year old woman presents to the GP surgery with concerns that she had no menstrual bleeds for the past 12 months. She used to have them on a regular basis. For the past few weeks she also has been experiencing hot flashes and night sweats. What is the most appropriate test to perform?
Correct Answer : A
The woman needs to be investigated for premature ovarian failure. That is done by having two raised FSH levels taken 4 weeks apart.
Q.136. A 38 year old female with lymphoma was treated with chemotherapy. She says she has been amenorrhoeic for the last 8 months. Lab results show: Follicle-stimulating hormone (FSH) 60 IU/L Luteinizing Hormone (LH) 77 IU/L Prolactin 13 ng/mL Oestradiol 26 pmol/L An FSH was repeated 4 weeks later was still elevated. What is the most likely diagnosis?
Correct Answer : D
The diagnosis of premature ovarian failure usually needs two raised levels of FSH (more than 40 IU/L) taken at least four weeks apart.
In this question, since she is amenorrhoeic with raised FSH and LH and a normal prolactin level, the most likely diagnosis would be premature ovarian failure. Women with premature ovarian failure also have low estradiol (usually < 50 pmol/L).
Q.137. A 32 year old woman, primigravida and now 39 weeks gestation attends the antenatal day unit with sudden onset of epigastric pain associated with nausea and vomiting. On physical examination, there is right upper quadrant tenderness. Her temperature is 36.8 C, blood pressure is 165/95, heart rate 90 bpm and respiratory rate 19/min. Her blood tests show: Haemoglobin 87 g/L Platelets 90 x 109/L Alanine transferase 219 U/L Aspartate transaminase 180 U/L Lactate dehydrogenase 720 U/L. What is the most likely diagnosis?
Correct Answer : B
Increased LDH levels suggest haemolysis. The decreased haemoglobin level, elevated liver enzymes, and low platelets give rise to the diagnosis of HELLP syndrome. This is supported by the fact that she has a high BP and epigastric pain that is associated with nausea and vomiting.
HELLP syndrome: This is a serious complication regarded by most as a variant of severe pre-eclampsia which manifests with haemolysis (H), elevated liver enzymes (EL), and low platelets (LP).
Liver enzymes usually increase and platelets decrease before haemolysis occurs. The syndrome is usually self-limiting, but permanent liver or renal damage may occur. Note that eclampsia may co-exist.
Signs and Symptoms:
• Epigastric or RUQ pain and tenderness
• Nausea and vomiting
• Urine is ‘tea-coloured’ due to haemolysis.
• Increased BP and other features of pre-eclampsia
Management :
• Delivery
• Supportive and as for eclampsia (magnesium sulfate (MgSO 4 ) is indicated)
• Although platelet levels may be very low, platelet infusions are only required if bleeding, or for surgery and <40.
Q.138. A 42 year old African lady presents with bloading and heavy, regular periods. Her uterine size correlates to a 14 weeks pregnant uterus. What is the most likely diagnosis?
Correct Answer : C
One must remember that uterine fibroids are more commonly found in Afro-Caribbean women. Menorrhagia and a uterus of 14 weeks in size are highly suggestive of a fibroid. A transvaginal ultrasound scan should be performed to assess the fibroid.
Q.139. A 19 year old lady with primary amenorrhoea has the following blood results Follicle stimulating hormone (FSH) 11 IU/L Luteinizing hormone (LH) 15 IU/L Prolactin 13 ng/mL Oestradiol 50 pmol/L. What is the most likely diagnosis?
Correct Answer : A
A normal LH, FSH, oestradiol, and prolactin rule out polycystic ovary syndrome (PCOS). In PCOS there would be an increased LH, increased FSH, and normal oestradiol. The LH: FSH ratio is usually 2:1 or 3:1.
In premature ovarian failure, LH and FSH are raised. Turner syndrome and absent ovary would have blood with low estradiol, high FSH, and LH. Thus, the only answer possible here would be an absent uterus.
Q.140. A 31 year old female presents to the infertility clinic with her husband. They have been trying to conceive for 3 years. Her BMI is 31 kg/m2. She has dark pigmentation on her neck and severe acne on her face. There is also thinningof hair. Blood test reveals elevated insulin levels, elevated LH levels and moderately elevated testosterone levels. What is the most appropriate diagnostic test to confirm the diagnosis?
Correct Answer : A
The most likely diagnosis here is Polycystic ovarian syndrome (PCOS).
Elevated insulin levels, elevated LH levels, and moderately elevated testosterone levels can be seen in PCOS. The scenario of acne on her face points towards an excess of androgens (Hirsutism, alopecia, and acne are all manifestations of hyperandrogenism). And not to mention that her initial complaint was infertility which is one of the diagnostic criterion for PCOS.
The dark pigmentation on her neck is called acanthosis nigricans which is characterized by brown to black hyperpigmentation of the skin found in body folds, such as the axilla, nape of the neck, and groin is a marker of insulin resistance.
Ultrasound pelvis is the most appropriate as seeing 12 or more follicles on the ovaries can help make the diagnosis.
Q.141. A 31 year old woman complains of increased urinary frequency and urinary urgency. She also describes painful voiding. She complains of dyschezia, dysmenorrhooea, sacral backache with menses and deep dyspareunia which has been worsening over the last year. What is the most likely diagnosis?
Correct Answer : D
This is a very uncommon presentation of endometriosis. Note that in some patients with endometriosis, along with the typical symptoms of endometriosis such as dysmenorrhoea and dyspareunia, they have increased urinary frequency, urgency, and painful voiding.
Symptoms such as dysuria may be due to the involvement of the bladder, peritoneum, or invasion of the bladder.
Sacral backache with menses is due to the growth and bleeding of the ectopic endometrium. These cyclic symptoms usually precede menses (24 to 48 hours) and continue throughout and after the flow. Dyschezia refers to pain on defaecation. It is a symptom of endometriosis and is seen when there are endometriotic lesions in the Pouch of Douglas or the recto-vaginal septum.
Q.142. A 38 year old woman has had no menstrual periods for the last 11 months. Prior to that, she had regular menstrual cycles. FSH was found raised (more than 40 IU/L) on two separate occasions a month apart. Her Thyroid-stimulating hormone (TSH) and prolactin are within normal limits. Her pregnancy test was negative. What is the most likely diagnosis?
Correct Answer : B
The blood results of increased levels of FSH on two separate occasions with prolonged amenorrhoea suggest premature ovarian failure.
Polycystic ovarian syndrome (PCOS) is incorrect as raised FSH makes PCOS unlikely. She also has no features of hyperandrogenism. Early menopause is used for those women who go through their menopause between 40-45 years.
Q.143. A 42 year old pregnant woman at 38 weeks gestation has an eclamptic fit in the labour ward which has been ongoing and started 10 minutes ago. She had severe pre-eclampsia which was diagnosed when she was 35 weeks gestation. She was given a loading dose of magnesium sulphate several hours ago and is currently on a maintenance dose. When she was last examined, there was loss of patellar reflexes and she was feeling nauseous and warm. What is the most appropriate next step?
Correct Answer : C
This lady is having a seizure but at the same time, she is experiencing signs and symptoms of magnesium sulphate toxicity.
Magnesium sulphate toxicity is characterized by confusion, loss of reflexes (deep tendon reflexes), respiratory depression, and hypotension. In obstetric women with magnesium sulphate toxicity, the following needs to be performed:
If only loss of patellar reflex or a respiratory rate less than 10 breaths/minute:
1. Stop magnesium sulphate maintenance infusion
2. Send magnesium sulphate levels to the laboratory urgently
3. Consider administration of intravenous calcium gluconate 1 g (10 ml) over 10 minutes if there is concern over respiratory depression. Calcium gluconate is the antidote.
4. Withhold further magnesium sulphate until patellar reflexes return or blood magnesium sulphate level known.
If cardiorespiratory arrest (due to magnesium sulphate toxicity) :
1. Crash call
2. Position woman in the left lateral tilt position and initiate CPR
3. Stop magnesium sulphate maintenance infusion
4. Administer intravenous calcium gluconate 1 g (10 ml) over 10 minutes. Calcium gluconate is the antidote.
5. Intubate immediately and manage with assisted ventilation until the resumption of spontaneous respirations
6. Send magnesium sulphate levels to the laboratory urgently In general, we do not use diazepam or phenytoin as an alternative to magnesium sulphate in women with eclampsia. However, since she is still having a fit, and magnesium sulphate toxicity is suspected, we are not able to use magnesium sulphate and thus diazepam would be the option here.
Note however, that we would only use it as a single dose since prolonged use of diazepam is associated with an increase in maternal death. If there were no features of magnesium sulphate toxicity in this question, recurrent seizures are treated with either a further bolus of 2 g magnesium sulphate or an increase in the infusion rate to 1.5 g or 2.0 g/hour.
The fetus should be continuously monitored with CTG.
The woman in this stem is 38 weeks pregnant, and so plans for delivery should be made once stabilized but there is no particular hurry, and a delay of several hours to make sure the correct care is in hand is acceptable assuming that there is no acute fetal concern such as fetal bradycardia.
Q.144. A 39 year old woman has not had her period for 10 months. She feels well but is anxious as her mother had an early menopause. What is the most appropriate initial investigation?
Correct Answer : C
Serum FSH/LH would be useful. Serum follicle-stimulating hormone (FSH) measurement alone can be used to diagnose premature ovarian failure.
Q.145. A 39 year old woman attends the GP for advice on contraception. Her medical history includes hypertension which is well controlled with ramipril. She is a non-smoker and has had 2 vaginal deliveries in the past. Which of the following contraception methods is LEAST appropriate?
Correct Answer : A
There are a few points worth remembering when it comes to questions on combined oral contraceptive pills.
Combined oral contraceptive pills are UNLIKELY to be the appropriate choice of contraception in the following scenarios in the exam.
• History of VTE or family history of VTE
• Migraine with aura
• BMI more than 30 kg/m2.
• Smoker or ex-smoker
• History of Breast cancer - It is alright to use COCP in patients with a family history of breast cancer as long as the patient does not have a history of breast cancer and is not a carrier of known gene mutations associated with breast cancer (e.g. BRCA1/BRCA2)
• Hypertension (even if adequately controlled)
Mnemonic: "Vitamins Make Boys Sleep Better Hours"
Q.146. A 51 year old, nulliparous professor comes to GP clinic with irregular heavy vaginal bleeding for the past 6 months. She complains of hot flushes and night sweats which began a few months ago. She feels tired most of the time and also having difficulty in sleeping. She states that her job is demanding and stressful at times. She has no significant past medical history. What is the most appropriate initial investigation?
Correct Answer : B
This patient may just be having signs and symptoms of perimenopause. If so, we could easily just do nothing and have no investigations performed. As this is not an option given, the next best option would be to arrange a transvaginal ultrasound scan.
Transvaginal ultrasounds are useful as an initial investigation for irregular heavy vaginal bleeding even in the perimenopausal period with its primary use to look at endometrial thickness as a thick endometrium would prompt a referral for a hysteroscopy and endometrial biopsy to exclude endometrial cancer.
The reason we say that she is perimenopausal and not menopausal is because perimenopause includes the period beginning the first clinical, biological, and endocrinological features of the approaching menopause, such as vasomotor symptoms and menstrual irregularity whereas menopause is defined as 1 year of amenorrhoea after the age of 50 years old (alternatively 2 years of amenorrhoea after the age of 45). Fibroids may also be a cause of irregular heavy bleeding, but at this age group, it has less of an impact as fibroids tend to decrease in size once reaching perimenopause and menopause. This is because of the decrease in oestrogen and progesterone which are hormones involved in stimulating the growth of the fibroids.
The confusion that people have with this question is that they are looking for a test that is used to diagnose menopause. A key point worth remembering from guidelines in 2015 is that the diagnosis of menopause in healthy women above the age of 45 years should be based on symptoms and menopausal patterns and thus we should NOT routinely check FSH.
FSH levels tend to fluctuate in the perimenopausal period and so are unhelpful in diagnosing menopause in women above the age of 45. When is FSH useful? It is useful in the diagnosis of premature ovarian failure or early menopause (< 45 y).
Two FSH levels would be required and they are taken 4 to 8 weeks apart. FSH also has its use in decisions regarding stopping contraception however it is unlikely to be raised. Serum estradiol and progesterone are not helpful and it is not recommended by NICE in diagnosing menopause.
The key point to remember in this question: A transvaginal ultrasound scan may be considered for women with atypical symptoms of menopause which would involve heavy irregular bleeding.
Q.147. A 68 year old nulliparous woman presents to her general practitioner with a six-month history of poorly-localised abdominal discomfort and a constant feeling of bloatedness. On pelvic examination you find a nontender, 7 cm solid, irregular, fixed left adnexal mass. Her last examination was 1 year ago, which was normal, and in included a normal Pap smear. What is the most appropriate initial investigation?
Correct Answer : D
This is a classic presentation of ovarian cancer.
Concerns should be raised with any pelvic mass that is identified after menopause. Ovaries in the postmenopausal age group should be atrophic, and anytime they are enlarged, the suspicion of ovarian cancer arises.
The term “nulliparous” was thrown into the question to help guide you toward the suspicion of ovarian cancer as nulliparity is a risk factor.
In a woman of this age with persistent symptoms of abdominal discomfort and bloating it is essential to consider the possibility of ovarian cancer. Due to the nonspecific nature of symptoms of this disease, you should have a low threshold for initiating investigations. Serum CA125 is a tumour marker that is used in the investigation of possible ovarian cancer, though it is not 100% sensitive or specific for this disease.
Guidelines state that serum CA 125 should be performed if a woman
- Especially if aged 50 years old or over
- Has any of the following symptoms regularly
• Abdominal distension or 'bloating'
• Early satiety or loss of appetite
• Pelvic or abdominal pain
• Increased urinary urgency and/or frequency.
Q.148. A 28 year old female has had 3 consecutive miscarriages. All her miscarriages happened before 10 weeks. Cytogenetic analysis performed on products of conception of the third miscarriage shows no abnormalities. She comes to clinic inquiring if it is safe for another pregnancy. What is the most appropriate investigation to perform?
Correct Answer : A
All women with recurrent first-trimester miscarriages and all women with one or more second-trimester miscarriages should be screened before pregnancy for antiphospholipid antibodies.
Parental peripheral blood karyotyping of both partners should be performed in couples with recurrent miscarriages where testing of products of conception reports an unbalanced structural chromosomal abnormality.
But in this case, cytogenetic analysis performed on products of conception shows no abnormalities thus there is no need for parental karyotyping. There is currently no satisfactory objective test that can identify women with cervical weakness in the non-pregnant state.
Hence, the option for transvaginal ultrasound for cervical length is incorrect.
Q.149. A 37 year old woman has irregular menstrual cycles for the last 9 months accompanied by hot flashes and night sweats. She also complains of pain during sexual intercourse. What is the most appropriate initial investigation?
Correct Answer : C
Serum follicle-stimulating hormone (FSH) measurement alone can be used to diagnose premature ovarian failure Note that Anti-Mullerian hormone can also be used to help diagnose premature ovarian failure as it is a measure of reduced ovarian reserve. However, it is usually only undertaken if there is diagnostic uncertainty.
Q.150. A 25 year old woman had an emergency lower segment Caesarean section after a prolonged labour 4 days ago due to fetal distress. She now complains of intermittent vaginal bleeding and foul smelling discharge. Her O2 saturation is 98% on air, blood pressure is 124/88 mmHg, pulse of 84 beats/minute and temperature of 37.9 C. The midwife tells you that the obstetric surgeons had difficulty in removing the placenta from the uterus in the operating theatre. What is the most likely complication of this woman from the Caesarean section?
Correct Answer : D
Although retained products of conception may be an option. Endometritis fits more perfectly with the scenario given the fever, the history of an emergency C-section, prolonged labour, and the foul discharge.
Uterine infection (endometritis) Is the most common cause of postpartum fever.
Predisposing factors :
• Emergency caesarean section
• Prelabour rupture of membranes
• Prolonged labour
• Multiple pelvic examinations.
• Internal fetal monitoring - use of scalp electrodes/ intrauterine
Signs and symptoms :
• Fever usually in proportion to the extent of infection.
• Foul smelling, profuse, and bloody discharge.
• Tender bulky uterus on abdominal examination
Management :
• Antibiotics
Q.151. A 33 year old woman with 3 previous normal vaginal deliveries is diagnosed with stress incontinence. She has tried pelvic floor exercises and lifestyle modifications but they have not been successful. Her BMI is 29. What is the most appropriate management?
Correct Answer : A
Stress incontinence is a leak of small amounts of urine when coughing or laughing. Usually with a history of many vaginal deliveries as this would weaken the pelvic floor muscles. The next management here would be surgical. A tension-free vaginal tape would be appropriate.
The other options are less likely the correct answer: Bladder training is used for women with urgency or mixed urinary incontinence. It is not used for stress incontinence.
Oestrogens do not offer systemic hormone replacement therapy for the treatment of urinary incontinence Intermittent urethral catheters. This is primarily for people with urinary retention rather than stress incontinence Antimuscarinic medications are used to treat overactive bladder and not stress incontinence.
Q.152. A 29 year old woman has chronic cyclical pelvic pain, and dysmenorrhoea over the last 9 months in which she takes NSAIDs for. She complains of pain during sexual intercourse. A trial of combined oral contraceptive pills was given but there was no reported benefit. She denies any urinary or bowel symptoms. What is the most definitive diagnostic test?
Correct Answer : C
The likely diagnosis here is endometriosis. A laparoscopy would be the gold standard to diagnose it. A laparoscopy would also be able to identify any other pathologies that may be causing the chronic pelvic pain such as adhesions. Serum CA125 may be seen elevated with endometriosis, however, there is no evidence that it is a useful screening test for this endometriosis. Ultrasound pelvis may help detect ovarian endometriosis but is unable to detect peritoneal disease.
Remember, pelvic ultrasound scans are likely to be normal but are still requested in some cases to help to diagnose an ovarian endometrioma (cyst) associated with endometriosis.
NICE clearly states that pelvic MRI should NOT be performed as a primary investigation to diagnose endometriosis.
An MRI can be considered before operative laparoscopy in women with suspected deep endometriosis involving bowel, bladder, or ureter which is not the case here.
A hysteroscopy has no value in diagnosing endometriosis as the presence of endometrial-like tissue is outside of the uterine cavity.
Q.153. A 23 year old woman has had intermittent abdominal pain in the left iliac fossa for 6 weeks. Over the past 48 hours, she had had severe abdominal pain and fever of 39 C. Urine HCG is negatibve. She also has cervical motion tenderness. Pelvic ultrasound shows a 6.5 cm multilocular complex adnexal mass. Her WBC and CRP are raised. What is the most likely diagnosis?
Correct Answer : D
This question describes Tubo-ovarian abscess which is a complication of PID. The ultrasound findings of a tubo-ovarian abscess usually show a multilocular complex adnexal mass with debris, septations, and irregular thick walls.
Endometriosis : Does not present as a mass in the US.
Ovarian cancer : Unlikely as she is very young and she has signs of an infection.
Ectopic pregnancy : Unlikely as urine BHC is negative and signs and symptoms point towards PID.
Dermoid cyst : Typically an ovarian dermoid is seen as a cystic adnexal mass with some mural components. Most lesions are unilocular.
Q.154. A 52 year old woman has hot flashes, night sweats and insomnia. She also complains of vaginal dryness and symptoms of urinary frequency. Her last menstrual period was 11 months ago. Her medical history includes having a myocardial infarction when she was 48 years old. What is the most appropriate management for her?
Correct Answer : B
Hormone replacement therapy like oestrogen and progestogen patches are indicated here as she is having menopausal symptoms. This systemic treatment can also alleviate symptoms of vaginal dryness and symptoms of urinary frequency. A vaginal oestrogen cream or pessary would be appropriate if the patient only had symptoms of vaginal dryness without the other symptoms of menopause like hot flushes. In such cases, there is no need for a systemic treatment as topical treatment can alleviate symptoms.
The history of a myocardial infarction is irrelevant. The relation between HRT and cardiovascular disease is controversial. The National Institute for Health and Care Excellence (NICE) states that HRT does not increase cardiovascular risk when started in women aged under 60 years and does not affect the risk of dying from cardiovascular disease and hence the presence of cardiovascular risk factors is NOT a contraindication to HRT.
Q.155. A 23 year old woman has vaginal discharge and bleeding. An endocervical swab was taken which tested positive for Neisseria gonorrhoeae. What is the most appropriate management?
Correct Answer : A
Please see Q- 69
Q.156. A 55 year old woman presents to the clinic with an itchy, tender white plaque on her vulva. The itch is especially worse at night and often disturbs her sleep. Her past medical history includes type 1 diabetes mellitus. She has no family history of cancer. What is the most likely diagnosis?
Correct Answer : B
Lichen sclerosus is a chronic inflammatory dermatosis that usually affects the skin of the anogenital region in women. It presents with general itching and is seen as white atrophic plaques. It occurs in little girls or middle-aged women. It is thought to have an autoimmune mechanism in the pathogenesis. The main complaint is itching which is worse at night.
Dyspareunia and pain may be seen in cases of erosions or fissures. Topical steroids are used as part of the management. Follow-up is important and is recommended at three and six months, to ensure responses to treatment. This is because long-standing, untreated cases show a 4% incidence of malignant change (association with development of squamous cell carcinoma of the vulva).
Q.157. A 27 year old lady presents with lower abdominal pain in the emergency department. 2 weeks ago, she came to the hospital with fever, suprapubic tenderness and vaginal discharge. Pelvic inflammatory disease (PID) was confirmed and she was sent home on oral doxycycline and oral metronidazole. She now presents with abdominal tenderness, temperature of 39.0 C, heart rate of 98 bpm and a blood pressure of 130/85 mmHg. What is the most appropriate next course of action?
Correct Answer : C
The possible diagnosis here is a pelvic abscess or tubo-ovarian abscess which are complications of PID. A high vaginal swab or endocervical swab can take days to return with results.
As this is an A&E case, an ultrasound would be more appropriate as this would lead to a diagnosis. Ultrasound scan is the diagnostic imaging method of choice for acute pelvic pain in gynaecology.
It can easily diagnose sequelae of PID (including pyosalpinx and tuba ovarian abscess). Laparoscopy would be the next step after finding a mass on ultrasound. Abdominal X-ray has no part in the diagnosis of a pelvic abscess.
Q.158. A 30 year old multiparous woman has just delivered a term male baby. She is group A (-) and her husband’s blood group is unknown. She does not remember having any intramuscular injections in her previous pregnancy. The infant boy develops severe jaundice within a few hours after being born. What is the most likely diagnosis?
Correct Answer : D
The mother did not receive any Anti-D injections in her previous pregnancy. The stem is trying to tell you that she was immunized during her last pregnancy when delivered a Rhesus (+ve) baby. This woman now has antibodies against fetal RBC.
They attack fetal red blood cells causing a bilirubin build up leading to jaundice. Other common causes of jaundice which present within 24 hours of birth are ABO incompatibility, G6PD, and sepsis. However, the stem does not provide any information that would point you to pick any of them.
Q.159. A 36 year old primigravida who is 32 weeks pregnant is brought in by ambulance because she is experiencing sudden constant abdominal pain which started 3 hours ago. She denies any blood loss vaginally. Her uterus is tender and hard. Fetal distress is seen on CTG. Her blood pressure is 100/70 mmHg. What is the most likely diagnosis?
Correct Answer : A
Abruption of the placenta can still occur despite no evidence of vaginal bleeding. This type of abruption is called concealed abruption and it occurs in less than 20% of all placental abruptions.
Q.160. A 20 year old pregnant woman attends labour ward at 37 weeks of gestation with lower abdominal pain which started several hours ago with small amounts of bleeding. The abdominal pain is now settled and there is no uterine activity. On examination, the size of uterus is compatible with dates. What is the most appropriate initial investigation?
Correct Answer : B
Although the clinical scenario here looks like placenta abruption, one important diagnosis that we need to rule out as well as a placenta praevia for which initial the investigation of choice is an ultrasound. An ultrasound cannot exclude placental abruption, which is a clinical diagnosis. Placenta praevia usually presents with a painless vaginal bleed however the abdominal pain in this stem could very well be mild contraction pains.
With every episode of bleeding, a rhesus-negative woman should have a Kleihauer test and be given prophylactic anti-D immunoglobulin however this should not be done in an acute setting as the first investigation. A Kleihauer-Betke test can wait.
It is worth mentioning that if the question was asking for the best action and a CTG was within one of the options, that would usually be the best action. The reason behind this is placenta abruption is part of the differential and if the CTG shows fetal distress, the baby would need to be delivered immediately. There is no time to wait around for an ultrasound. Speculum examination is important to exclude a cervical cause of bleeding such as chlamydia but ideally, this should be done after the ultrasound scan rules out placenta praevia.
Q.161. A 16 year old girl has complaints of dysmenorrhoea, menorrhagia and irregular menstrual cycles. These complaints started a few years ago and has gotten worse with time. Her period pain is so intense that she occasionally has to skip school to stay at home. She has not tried any medication to manage her symptoms. She is not sexually active. What is the most likely management to treat her symptoms?
Correct Answer : C
Combined oral contraceptive pills suppress the production of gonadotrophins and are thought to reduce menstrual blood loss by up to 50%. It can improve dysmenorrhoea, lighten periods, regulate the cycle, and improve premenstrual symptoms, COCP is very useful in adolescence. Also, note that tranexamic acid is also effective. Although the levonorgestrel intra-uterine system is the first line for menorrhagia, it is difficult to fit in a nulliparous woman as her cervix has not yet been dilated before.
However, there has been more and more research regarding the use of levonorgestrel intrauterine systems in nulliparous women and some clinicians would prefer levonorgestrel intra-uterine system to combined oral contraceptives. They argue that the levonorgestrel intra-uterine systems such as Jaydess may be fitted more easily, as the frame is smaller and narrower compared to the Mirena IUS.
In this situation, she is not sexually active so preference should go towards combined oral contraception to control the bleeding as a girl her age might feel uncomfortable with a speculum examination. NSAIDS such as mefenamic acid may decrease menstrual blood loss by up to 20–30% and also significant decreases in dysmenorrhoea.
But it will not regulate her periods whereas COCP will regulate an irregular cycle.
NICE has suggested that this medical management of heavy menstrual bleeding should be considered in the following order:
1. Levonorgestrel-releasing hormone
2. Tranexamic acid or non-steroidal anti-inflammatory drugs (NSAIDs) or combined oral contraceptives
3. Norethisterone (15 mg) daily from days 5 to 26 of the menstrual cycle or infected long-acting progestogens
There are certain situations where one might choose a different order.
The summary to answering these types of questions is as below:
• Dysmenorrhoea in a young girl – Mefenamic acid
• Dysmenorrhoea, menorrhagia, and irregular menstrual cycles in a young girl – COCP
• Dysmenorrhoea, menorrhagia, and irregular menstrual cycles in sexually active women (or para 1 or more) – Levonorgestrel intra-uterine system.
Q.162. A 23 year old pregnant woman is admitted at 38 weeks gestation with a history of an eclamptic fit at home. Her blood pressure is 155/90 mmHg. She is conscious and observations are stable. What is the most appropriate IV therapy to prevent further list?
Correct Answer : C
Please see Q-121
Q.163. A 32 year old female with type 2 diabetes mellitus would like to know about vitamins and supplements in pregnancy. Which most likely vitamin prevents teratogenic effects in an unborn child?
Correct Answer : A
Advise women with diabetes who are planning to become pregnant to take folic acid (5 mg/day) until 12 weeks of gestation to reduce the risk of having a baby with a neural tube defect.
Q.164. A 28 year old woman has been admitted at 38 weeks gestation. Her blood pressure is 190/120 mmHg and proteinuria is seen on urinalysis. Immediately following admission, she has a grand-mal seizure. What is the most appropriate initial management?
Correct Answer : D
Intravenous magnesium sulphate is the most important initial management. Fetal CTG is also needed, but MgSO4 comes first. Delivery should follow after stabilizing the mother.
Q.165. A 65 year old female patient diagnosed with breast cancer was given tamoxifen. Which symptoms would be the most alarming?
Correct Answer : B
Tamoxifen is a risk factor for endometrial carcinoma. So vaginal bleeding will be of concern for us.
Q.166. A 39 year old female was on combined oral contraceptive pills which she stopped 9 months ago. She has not had her periods since then. Lab results show: Follicle stimulating hormone (FSH) 55 U/L Luteinizing Hormone (LH) 75 U/L Prolactin 14 ng/mL Oestradiol 30 pmol/L What is the most likely diagnosis?
Correct Answer : A
The diagnosis of premature ovarian failure usually needs two raised levels of FSH (more than 40 IU/L) taken at least four weeks apart.
In this question, since she is amenorrheic with raised FSH and LH and a normal prolactin level, the most likely diagnosis would be premature ovarian failure.
Women with premature ovarian failure also have low estradiol (usually < 50 pmol/l).
Q.167. A 23 year old lady with a BMI of 30 kg/m2 attends the GP surgery with complaints of facial hair growth and has a history of amenorrhoea for the past 6 months. Blood tests were requested and the results show: Follicle-stimulating hormone (FSH) 22 IU/L Luteinizing hormone (LH) 54 IU/L Prolactin 60 ng/mL Oestradiol 117 pmol/L Progesterone 100 ng/dL What is the most likely diagnosis?
Correct Answer : D
Obese, amenorrhoea, and hirsutism are consistent with Polycystic ovary syndrome (PCOS). She has high LH, normal FSH, and slightly high prolactin levels.
These are not diagnostic for PCOS but among the choices given, the lab results reflect PCOS. Serum LH levels are elevated in approximately 40% of women with PCOS, owing to increased production (increased amplitude and frequency of LH pulses). Prolactin may be mildly elevated in PCOS.
It has been described by some authors that women with polycystic ovary syndrome (PCOS) may have elevated levels of prolactin. However, a diagnostic criterion is to rule out other possible causes, including hyperprolactinemia.
This is because high prolactin levels have many of the same symptoms as PCOS and need to be ruled out to be certain of a PCOS diagnosis.
Q.168. A 35 year old lady at her 28th week gestation attends her antenatal clinic for a routine check-up. She feels well and has no complaints. Her blood pressure is 160/95 mmHg and her urine dipstick shows a 3+ protein. What is the most likely diagnosis?
Correct Answer : C
The definitions for hypertensive disease in pregnancy are important. Pre-eclampsia is where a 20 weeks of gestation woman has a blood pressure more than 140/90 mmHG and proteinuria (> 0.3 g/24 hours).
Q.169. A 32 year old primigravida at 28 weeks gestation presents with a blood pressure of 152/105 mmHg. A second blood pressure reading was taken 10 minutes later which read 153/108 mmHg. She is asymptomatic and otherwise well. A urinalysis was negative for protein. She has no history of high blood pressure in the past. What is the most likely management?
Correct Answer : B
Labetalol is the most studied antihypertensive in pregnancy with the safest profile.
Pregnancy Induced Hypertension :
The general management for gestational hypertension can be summarized below -
Degree of hypertension: Mild hypertension (140/90 to 149/99 mmHg) - No Treatment.
Moderate hypertension (150/100 to 159/109 mmHg) - With oral labetalol as first-line treatment to keep
• Diastolic blood pressure between 80-100 mmHg
• Systolic blood pressure less than 150 mmHg
Severe hypertension (160/110 mmHg or higher) - Admit to hospital.
Treat with oral labetalol as first-line treatment to keep.
• Diastolic blood pressure between 80-100 mmHg
• Systolic blood pressure less than 150 mmHg.
Commonly used medicines in pregnancy are methyldopa and nifedipine.
Q.170. A 26 year old woman has been found to have mild dyskariosis on a routine cervical screening test. She is a heavy smoker. What is the most appropriate next step in action?
Correct Answer : A
The first step is understanding that the screening result of mild dyskaryosis would follow samples being sent for HPV testing. If mild dyskaryosis is present but there is an absence of HPV testing, then this case should be referred to colposcopy. This means that if HPV testing was part of the options, that would be a better answer compared to colposcopy.
The second step is understanding what a colposcopy includes.
A colposcopy involves visualising the cervix using a microscope. A speculum is used to open the vagina and the cervix is stained with acetic acid in the area of the transformation zone (TZ) to identify the site, grade, and shape of any abnormal area of cells.
Iodine is then gently applied to the rest of the cervix to identify the complete area of abnormality.
A small biopsy is usually taken to be sent to the laboratory. When an area of abnormality extends into the cervical canal beyond the area that can be seen with the colposcope, a cone biopsy is indicated. We need a colposcopy first before we can be certain if a cone biopsy is required, hence the option for cone biopsy is incorrect.
Large loop excision of the transformation zone (LLETZ) takes place at the end of colposcopy if abnormality is obvious on colposcopy or for women who have had a positive biopsy result. Therefore if the option for colposcopy is present, that would take priority over the option for LLETZ since the question is asking for “the next step in action”.
Endocervical swabs have no value in the management of cervical screening tests. Endocervical swabs are used to diagnose chlamydia or gonorrhoea.
SUMMARY OF MANAGEMENT OF CERVICAL SCREENING TEST RESULTS :
Negative – Recall for screening as appropriate for a negative result Inflammatory.
– Repeat cervical swab in 6 months, consider taking swabs for infection if severe inflammation
Inadequate – Repeat sample
– If results are still persistently inadequate, assess using colposcopy
Borderline – Perform HPV testing on these samples – If HPV positive, refer for colposcopy.
Mild dyskaryosis – Perform HPV testing on these samples – If HPV positive, refer for colposcopy.
Note: If mild dyskaryosis and absence of HPV testing or HPV results are unreliable or inadequate, refer for colposcopy.
Moderate dyskaryosis or Severe dyskaryosis – Refer for urgent colposcopy for suspected cancer (two-week wait).
Q.171. A 64 year old woman has been on hormone replacement therapy for 5 years. She had regular withdrawal bleeds until 3 years ago and has not had a bleeding since. Recently she noticed a brown vaginal discharge on her underpants. Her last cervical smear was 3 years ago which showed no abnormalities. What is the most appropriate initial investigation?
Correct Answer : C
The idea here is to think of endometrial cancer. Any woman who has postmenopausal bleeding should have a transvaginal ultrasound to determine the endometrial thickness.
If the endometrium is thick, hysteroscopy with endometrial biopsy would be arranged. The hormone replacement therapy in this scenario has no relevance as HRT (progesterone and oestrogen) is not a risk factor for endometrial cancer.
Only unopposed oestrogen would be a risk factor for endometrial cancer.
A cervical smear is offered every 5 years if in the age group of 50 to 64 years old. Thus, having a cervical smear that was normal 3 years ago is a usual phenomenon. A repeat cervical smear is not necessary.
Q.172. An 8 week pregnant woman presents with persistent nausea and vomiting and a history of weight loss. She has a pulseof 110 beats/minute. Her dehydration has been managed with sodium chloride 0.9% with added potassium chloride. She continues to vomit several times during the day despite being given intramuscular cyclizine. What is the next most appropriate management?
Correct Answer : C
This is a case of hyperemesis gravidarum. Intravenous fluids is the most important part of management to ensure that the patient is not dehydrated. As this has already been given and dehydration managed, intravenous antiemetics is the next best answer since only intramuscular cyclizine has been given. Regular antiemetics such as promethazine or cyclizine are often tried first in many early pregnancy units.
If this fails, prochlorperazine intramuscularly or orally can be added on. If the patient continues to vomit, intravenous metoclopramide or ondansetron can be used on top of the already prescribed regular antiemetics. Advice such as eat little and often should be given.
Thiamine is also used in hyperemesis gravidarum and should ideally be given to all women admitted with prolonged vomiting.
This is to prevent Wernicke’s encephalopathy which is due to vitamin B1 (thiamine) deficiency.
However, the importance of thiamine in an acutely vomiting woman is less compared to having intravenous antiemetics. Intravenous corticosteroids is NOT the answer here.
Corticosteroids may be used for intractable cases of severe hyperemesis gravidarum in secondary care but this is usually a consultant decision and all other measures such as intravenous antiemetics have been taken to attempt to manage the patient's vomiting.
Q.173. A 45 year old waitress complains of pelvic pain which worsens pre-menstrually. The pelvic pain is usually worse when standing and has been present for the last one year. She also complains of post-coital ache that is felt deep within the vagina. There was no discharge on vaginal examination. A diagnostic laparoscopy was performed which did not show any abnormalities. What is the most likely diagnosis?
Correct Answer : B
Non-organic dyspareunia + with symptoms similar to premenstrual syndrome + aggravated by standing = Pelvic congestion syndrome
Q.174. A 37 year old woman presents with heavy vaginal bleeding for the past several months. A transvaginal ultrasound scan shows a 4 cm anterior subserosal fibroid and a 6 cm fundal intramural fibroid. She has been trying to conceive with her husband for the past year with no success and wants a management that would preserve her fertility. What is the most appropriate management?
Correct Answer : B
Abdominal myomectomy is the most appropriate in this situation. As the fibroids are seen to be subserosal and intramural, an abdominal incision would give us access to these fibroids. A vaginal approach using a hysteroscopy would be a choice for submucosal fibroids but not for intramural and subserosal fibroids.
Myomectomy and uterine artery embolization are both uterine-sparing surgeries and can both preserve her fertility but myomectomies are usually the better choice. If myomectomy has failed, uterine artery embolization may be attempted. Generally, women with fibroids causing infertility are offered myomectomies. The other options given will affect the patient's fertility.
Q.175. A 29 year old woman experienced severe blood loss shortly after delivery of a stillborn vaginally, following a major placental abruption. Given the risk factors, what is the most likely predisposing factor for developing postpartum haemorrhage in this woman?
Correct Answer : D
Although the incidence of DIC as a cause of postpartum haemorrhage is low. This question is giving all the risk factors that would lead to disseminated intravascular coagulation (DIC) With severe abruption, severe disseminated intravascular coagulation (DIC) may occur.
Fetal demise is also a risk factor for DIC resulting from the release of tissue thromboplastin from deteriorating fetal organs. Other causes of pregnancy-related DIC are eclampsia, retention of a dead fetus, amniotic fluid embolism, retained placenta, or bacterial sepsis.
Q.176. A 28 week pregnant lady presents with painless vaginal bleeding after sexual intercourse. The cervical os is closed. On ultrasound, placenta is noted to be anterior and high. Fetal movements and fetal heart is seen on scan. Abdomen is soft and nontender. What is the most likely diagnosis?
Correct Answer : B
Postcoital bleeding could be a symptom of either placenta praevia or cervical ectropion. As the placenta is noted to be high, it is not placenta praevia. A fetal heart was seen which excludes the diagnosis of missed miscarriage.
Placenta abruption would present a hard, tender abdomen. There are no signs or symptoms of disseminated intravascular coagulation. Cervical ectropion would be the most likely diagnosis.
Q.177. A 34 year old pregnant woman at 28 weeks gestation is seen in her antenatal appointment with a blood pressure of 165/120 mmHg. She was seen at her booking appointment at 10 weeks with a blood pressure of 110/80 mmHg. She feels well herself and has no complaints. A 24-hour protein was requested following a urinalysis which showed proteinuria. The 24-hour urine protein results show protein level of 0.2 g. What is the most accurate diagnostic term for this patient?
Correct Answer : A
For a formal diagnosis of pre-eclampsia, one would need to have more than 0.3 g of protein in urine in a 24-hour urine sample. Nowadays a 24-hour urine sample is rarely taken. Instead, a urine protein to creatinine ratio (urine PCR) may be ordered on a random urine sample if there is evidence of significant proteinuria on a urinalysis.
This urine protein to creatinine ratio is used to estimate the daily urine protein excretion. However, it is still important to remember that pre-eclampsia in the past was defined as having new hypertension (140/90) presenting after 20 weeks with significant proteinuria (> 0.3 g in 24 hours).
As the protein in this stem is less than 0.3 g, this patient would be labeled as having gestational hypertension. Gestational hypertension is new hypertension presenting after 20 weeks without significant proteinuria.
Q.178. An 18 year old female presents to her GP with the complaint of a vaginal discharge. She complains of the discharge being present for the past three weeks. When asked about her sexual history, she mentions that she is now in a new relationship. When prompted further, she also admits that she experiences post-coital bleeding. The patient has no significant past medical or gynaecological history. She is currently using the combined oral contraceptvie pill as a method of contraception. Her last menstrual period was two weeks days ago. On clinical examination, the vulva and the cervix appear to be red and inflamed. Examination of the pelvis elicited tenderness however an abdominal examination was normal. What is the most likely diagnosis in this patient?
Correct Answer : B
The patient has symptoms of cervicitis. Cervicitis describes any infection, irritation, or inflammation of the cervix, and the most likely cause, in this case, is an infection with chlamydia – an infection seen in young women with new sexual partners. Cervical ectropion usually does not cause any problems other than post-coital bleeding and most of them go away spontaneously without any medical intervention.
If intervention is required, it usually involves cauterising with silver nitrate. Given her age, cervical cancer is unlikely. Endometrial polyps tend to be asymptomatic however they can present with post-coital bleeding, intermenstrual bleeding, or menorrhagia. They do not cause vaginal discharge.
Q.179. A 30 year old woman visits her GP with concerns of vaginal spotting. She has had a Mirena coil inserted for contraceptive use 6 weeks ago. Her last menstrual period was 2 weeks ago. She denies abdominal pain or abnormal vaginal discharge. Her last cervical smear was 2 years ago. A speculum examination reveals a healthy looking cervix with the Mirena coil threads visible. What is the most appropriate action?
Correct Answer : D
Erratic bleeding is common after the insertion of a Mirena coil. In the first 3 to 6 months, periods may be irregular and heavy at first. Spotting is common during this period and reassurance is all that is required. By 1 year, most would have infrequent bleeding or amenorrhoea.
Q.180. A 53 year old woman complains of unbearable hot flushes and night sweats for the past month. She gives a history of having had a laparoscopically assisted vaginal hysterectomy 3 years ago. She smokes around 10 cigarettes a day for the past 20 years. What is the most appropriate treatment for her symptoms?
Correct Answer : C
Women who need treatment for vasomotor symptoms postmenopausally should be given hormone replacement therapy (HRT) for up to 5 years after discussing the long-term benefits and risks.
The rationale behind prescribing combined hormone replacement therapy for a woman who still has a uterus is to prevent endometrial hyperplasia which could lead to endometrial cancer if only an oestrogen preparation is used.
As she has had a hysterectomy, an oestrogen-only hormone replacement therapy would be suitable as she is no longer at risk of endometrial cancer. Smoking is not a contraindication for HRT use.
A transdermal approach would be preferred here as smoking can reduce the efficacy of orally administered oestrogens. Transdermal HRT does not increase the risk of venous thromboembolism whereas an oral HRT is seen to increase venous thromboembolism by 2 to 3 folds. Since she is a smoker, it would be wise to prescribe a transdermal HRT instead of oral to reduce her risk of venous thromboembolism. A point to remember in case the question asks specifically for the preferred route of HRT administration. Clonidine used to be popular for the treatment of vasomotor symptoms however it should not be used as first-line treatment of vasomotor symptoms as there is limited evidence of its efficacy and has many side effects. To recap, there are three types of HRT used.
Oestrogen-only HRT :
• Used on women who have a hysterectomy or an intrauterine system in situ.
Sequential (cyclical) combined HRT :
• Used in peri-menopausal women who are still menstruating or are within 12 months of their last period.
• Sequential combined HRT is where oestrogen is taken every day, and progestogen is taken sequentially (usually for the last 14 days of the menstrual cycle) to induce a bleed.
• Patients are often switched to continuous combined hormone replacement therapy after 12 months.
Continuous combined HRT :
• Used in menopausal women (i.e. women who have had their last period more than 12 months ago)
• As the name suggests, continuous combined HRT is where oestrogen and progestogen doses are taken daily.
Q.181. A pregnant lady came with pain in her calf muscle with local rise in temp to the antenatal clinic. What treatment should be started?
Correct Answer : B
Injections with low molecular weight heparin (LMWH) are usually used to treat pregnant women with DVT. LMWH prevents the blood clot getting bigger. It does not affect the developing baby.
Q.182. A 32-year-old woman of 39 weeks gestation attends the antenatal day unit feeling very unwell with sudden onset of epigastric pain associated with nausea and vomiting. Her temperature is 36.7C. Examination: she is found to have RUQ tenderness. Her blood results show mild anemia, low platelets, elevated liver enzymes and hemolysis. What is the most likely diagnosis?
Correct Answer : D
HELLP syndrome is a life-threatening liver disorder thought to be a type of severe preeclampsia.
It is characterized by Hemolysis (destruction of red blood cells), Elevated Liver enzymes (which indicate liver damage), and Low Platelet count. The main treatment is to deliver the baby as soon as possible, as early as after 34 weeks if multisystem disease is present.
Q.183. A female with type 1 DM would like to know about a deficiency of vitamins in pregnancy that can be harmful. A deficiency of which vitamin can lead to teratogenic effects in the child?
Correct Answer : A
Frequently associated with neural tube defect.
Q.184. A 23-year-old lady was prescribed with azithromycin 1 gm for her chlamydial pelvic infection. She has got a new partner for the last 2 months. She has recently started contraception to avoid conception. Which of the following contraception method will be affected by azithromycin?
Correct Answer : C
None of them!
COCPs are not affected by azithromycin.
• Enzyme-inducing antibiotics like rifampin reduce COCP effectiveness by increasing hepatic metabolism of estrogen, but azithromycin is not enzyme-inducing.
• Barrier methods and IUCD are non-hormonal and have no interaction with antibiotics.
Q.185. A 27-year-old lady has had an uncomplicated pregnancy so far. She came to the hospital 2 hours ago after her water broke. The midwife is looking at her now. She has regular contractions. P.V exam revealed 2 cm dilated cervix. Vital signs are normal. What stage of labour is she in?
Correct Answer : B
First stage starts with softening of cervix with start of opening of cervix and ends when cevix is fully dilated (i.e. 10 cm dilated).
Q.186. A 29-year-old woman had just delivered a still born vaginally, following a major placental abruption. Choose the most likely predisposing factor for developing PPH in this lady?
Correct Answer : B
Pregnancy itself is a risk factor for DIC. Placental abruption increases the risk of DIC further. Other causes of pregnancy related DIC are: eclampsia, retention of a dead fetus, amniotic fluid embolism, retained placenta or bacterial sepsis.
Q.187. A 28-year-old woman has delivered with rotational forceps after an 8 hours labor and 3 hours second stage. Choose the single most likely predisposing factor for PPH for this patient?
Correct Answer : B
Cervical/vaginal trauma - complication of forceps delivery.
Q.188. A 3-year-old woman has delivered after an induced labor which lasted 26 hours. choose the most likely predisposing factor for postpartum hemorrhage?
Correct Answer : A
Atonic uterus. Prolonged labour is a risk factor for PPH secondary to atonic uterus.
Q.189. A 25-year-old woman presented to her GP on a routine checkup. Upon vaginal examination, she was fine except for finding of cervical ectropion which was painless but mild contact bleeding on touch. What is the next management?
Correct Answer : B
25 year is the age when 1st smear is offered. Cervical smear is a screaning service which follows its own schedule and cannot be done unless it is due or overdue. As the Lady is of 25 years and has ectropion and contact bleeding smear is the best option here as 1st smear is offered at 25 yrs.
Q.190. A 32-year-old had a normal vaginal delivery 10 days ago. Her uterus has involuted normally. Choose the most likely predisposing factor for PPH?
Correct Answer : C
Uterine infection. Normal involution excludes retained product.
Q.191. A 41-year-old woman who has completed her family, has suffered from extremely heavy periods for many years. No medical treatment has worked. She admits that she would rather avoid open surgery. After discussion, you collectively decide on a procedure that wouldn’t require open surgery or GA. Select the most appropriate management for this case?
Correct Answer : D
Uterine artery embolization is done by interventional radiologist expert in arterial embolization technique. Particles are placed in uterine artery to block circulation to uterine body.
Q.192. A 25-year-old had an LSCS (lower segment cesarean section) 24hr ago for fetal distress. She now complains of intermittent vaginal bleeding. Observations: O2 saturation 98% in air, BP 124/82mmHg, pulse 84bpm, temperature 37.8C. Themidwife tells you that she had a retained placenta, which required manual removal in the OT.Choose the most appropriate C-Section complication in this case?
Correct Answer : C
Endometritis - Excessive handling of retained placenta lead to endometritis which is the cause of intermittent vaginal bleeding and raised temperature.
Q.193. A 25-year-old woman with type 1 diabetes mellitus has delivered a baby weighing 4.5kg. Her uterus is well contracted. Choose the most likely predisposing factor for PPH from the options?
Correct Answer : B
Cervical/vaginal trauma. The baby is a big baby. If patient’s uterus was not well contracted we would fear of atonic uterus! But as uterus is well contracted it is not atonic uterus. Rather most likely cause is trauma during delivery of this big baby.
Q.194. A 28-year-old woman at 39 weeks gestation is in labor. She develops abdominal pain and HR 125bpm, BP 100/42mmHg, temp 37.2C and saturation 99%. Examination: lower abdomen is exquisitely tender. CTG previously normal, now showing reduced variability and late deceleration with slow recovery. She has had 1 previous LSCS (lower segment cesarean section) for a breech baby. Choose the most appropriate CS (cesarean section) complication for this lady?
Correct Answer : D
Features of shock, exquisitely tender lower abdomen with abdominal pain, previously normal CTG now becoming non-reassuring and previous history of LSCS makes the diagnosis of uterine rupture.
Q.195. A 45-year-old waitress complains of pelvic pain which worsens pre-menstrually and on standing and walking. She also complains of post-coital ache. Select the most likely cause leading to her symptoms?
Correct Answer : C
Women with pelvic congestion syndrome experience a constant pain that may be dull and aching, but is occasionally more acute.
The pain is worse at the end of the day and after long periods of standing, and sufferers get relief when they lie down. The pain is worse during or after sexual intercourse, and can be worse just before the onset of the menstrual period.
Cause is attributed to female hormone estrogen induced vascular (venous) changes. So it is usually seen in females.
Q.196. A 35-year-old lady who has been using IUCD for one year now complains of pelvic pain and heavy painful periods. Select the most likely cause leading to her symptoms?
Correct Answer : A
The given picture may have D/D of PID or fibroid. As IUCD is a risk factor for PID, it is the most likely diagnosis of given picture. Menorrhagia for fibroids is usually painless.
Q.197. A 64-year-old woman has been on HRT for 9 years. She had regular withdrawal bleeds until 3 years ago and since then has been taking a no bleed preperation. Recently she noticed a brown vaginal discharge. Choose the most appropriate initial investigation?
Correct Answer : D
Transvaginal US to determine endometrial thickness. In a postmenopausal woman with vaginal bleeding, the risk of cancer is approximately 7.3% if her endometrium is thick (> 5 mm) and < 0.07% if her endometrium is thin (5 mm).
In postmenopausal women without vaginal bleeding, the risk of cancer is approximately 6.7% if the endometrium is thick (> 11 mm) and 0.002% if the endometrium is thin (11 mm).
Q.198. A 20-year-old young lady comes to the GP for advice regarding cervical carcinoma. she is worried as her mother past away because of this. She would like to know what is the best method of contraception in her case?
Correct Answer : B
Spermatozoa itself acts as a carcinogen. So barrier method is the best protection from the given options.
Q.199. A 44-year-old woman complains of heavy bleeding per vagina. Transvaginal US (ultra sonography) was done and normal. Which of the following would be the most appropriate investigation for her?
Correct Answer : C
Transvaginal US is normal i.e. no endometrial hyperplasia, no fibroid or obvious cause for heavy bleeding was found. So now most appropriate investigation should be coagulation profile.
Q.200. A 24-year-old woman presents with deep dyspareunia and severe pain in every cycle. What is the initial investigation?
Correct Answer : B
The likely diagnosis is endometriosis. Endometriosis is a condition where tissue similar to the lining of the womb starts to grow in other places, such as the ovaries and fallopian tubes. There may be pelvic pain that is worse during period. Period pain that stops the patient from normal activity. There may be dyspareunia, menorrhagia and difficulty getting pregnant.
Q.201. A 38-year-old woman, 10 day postpartum presents to the GP with history of passing blood clots per vagina since yesterday. Examinatio: BP 90/40mmhg, pulse 110bpm, temperature 38C, uterus tender on palpation and fundus 2cm above umbilicus, blood clots +++. Choose the most likely diagnosis.
Correct Answer : D
Secondary PPH is defined as abnormal or excessive bleeding from the birth canal between 24 hours and 12 weeks postnatally.
Q.202. A 32-year-old female with 3 previous 1st trimester miscarriages is diagnosed with antiphospholipid syndrome. Anticardiolipin antibodies +ve. She is now 18 weeks pregnant. What would be the most appropriate management?
Correct Answer : C
Aspirin & heparin
Q.203. A 23-year-old presents with vomiting, nausea and dizziness. She says her menstrual period has been delayed 4 weeks as she was stressed recently. There are no symptoms present. What is the next appropriate management?
Correct Answer : D
Likely diagnosis is pregnancy. Features like vomiting, nausea and dizziness are consistent with early pregnancy supported by delayed menstruation.
Q.204. A 16-year-old girl came to the sexual clinic. She complains of painful and heavy bleeding. She says she doesn’t have a regular cycle. What is the most appropriate management?
Correct Answer : B
Combined pill
Q.205. Which method of contraception can cause the risk of ectopic pregnancy?
Correct Answer : B
IUCD
Q.206. A 31-year-old woman who is 32 weeks pregnant attends the antenatal clinic. Lab investigations: Hgb 10.7, MCV 91. What is the most appropriate management for this patient?
Correct Answer : D
No treatment required. According to NICE, cut offs for iron supplements: at booking (8-10 weeks)- if less than 11 at 28 weeks and further- if less than 10.5 if less than these values=> give iron.
Q.207. A 32-year-old woman of 39 weeks gestation attends the antenatal day unit feeling very unwell with sudden onset of epigastric pain along with nausea and vomiting. Temperature 36.7C. Examination: right upper quadrant tenderness. Bloods: mild anemia, low platelets, elevated LFT (liver function test) and hemolysis. What is the most likely diagnosis?
Correct Answer : D
HELLP syndrome.
H=hemolysis, EL=elevated liver enzyme, LP=low platelet count.
Q.208. A 57-year-old woman presents with dysuria, frequency and urinary incontinence. She complains of dyspareunia. Urine culture has been done and is sterile. What is the most appropriate step?
Correct Answer : C
Topical estrogen.
There may be UTI like symptoms and dyspareunia in atrophic vaginitis for which topical oestrogen can be used.
Q.209. A patient came to the emergency department with severe lower abdominal pain. Vitals: BP 125/85 mmHg, Temp 38.9C. Examination: abdomen rigid, very uncomfortable during per vaginal. She gave a past history of PID (pelvic inflammatory disease) 3 years ago which was successfully treated with antibiotics. What is the appropriate investigation?
Correct Answer : A
Patient had previous PID. Current symptoms of severe cervical motion tenderness with significant rise of temperature is very much suggestive of pelvic abscess.
Q.210. A 24-year-old 18 week pregnant lady presents with pain in her lower abdomen for the last 24h. She had painless vaginal bleeding. Exam: abdomen is tender, os is closed. What is the most probable diagnosis?
Correct Answer : A
Threatened miscarriage.
Gestational age 18 weeks, lower abdominal pain, tender abdomen, closed os and painless vaginal bleeding indicates threatened abortion.
Q.211. A 32-year-old female who has had 3 previous miscarriages in the 1st trimester now comes with vaginal bleeding at 8 weeks. US (ultrasound) reveals a viable fetus. What would be the most appropriate definitive management?
Correct Answer : B
Early miscarriage is more common in antiphospholipid syndrome and treated with heparin or aspirin when become pregnant.
Q.212. A 27-year-old 34 week pregnant lady presents with headache, epigastric pain and vomiting. Examination: Pulse 115, BP 145/95 mmHg, proteinuria ++. She complains of visual disturbance. What is the best medication for the treatment of the BP?
Correct Answer : D
No treatment.
Here, question specifically asked for treatment of BP. In case of BP of 145/95 mmHg no treatment for BP is needed.
Q.213. A 24-year-old lady who is 37 weeks pregnant was brought to the emergency department. Her husband says a few hours ago she complained of headache, visual disturbance and abdominal pain. On arrival at the emergency department she has a fit. What is the next appropriate management for this patient?
Correct Answer : A
4g MgSO4 in 100ml 0.9%NS in 5mins.
Diagnosis is eclampsia.
Q.214. A 24-year-old girl comes to the woman sexual clinic and seeks advice for contraception. She is on sodium valproate.
Correct Answer : D
She can use COCP. Sodium valproate has no effect on COCP.
Q.215. A 27-year-old lady came to the emergency department 10 days ago with fever, suprapubic tenderness and vaginal discharge. PID was diagnosed. She has been on the antibiotics for the last 10 days. She presents again with lower abdominal pain. Temperature 39.5C. What is the most appropriate next management?
Correct Answer : C
USG.
Initial presentation was of PID. But recurrance of symptoms suggests resistant condition like abscess formation.
Q.216. A 27-year-old presents with abdominal pain, bleeding, vomiting and diarrhea. Her LMP was 7 weeks ago. Examination: abdominal tenderness, BP 90/60mmHg. What is the next appropriate management?
Correct Answer : A
Immediate laparotomy.
BP is low. Patient is in shock and abdominal tenderness warns us about probable rupture.
Q.217. Which of the following is NOT a physiological change during pregnancy?
Correct Answer : A
Tidal volume 500ml
Q.218. A patient presents with complete anuria following prolonged hypotension and shock in a patient who bled profusely from a placental abruption. What is the most probable diagnosis?
Correct Answer : C
Acute cortical necrosis. There are 2 reasons for this acute cortical necrosis.
i) Significant diminished arterial perfusion of the kidneys due to spasm of the feeding artery secondary to profuse bleeding from placental abruption
ii) DIC secondary to placental abruption.
Q.219. A 45-year-old lady came to family planning clinic for contraception advice. She is not keen to be pregnant for the next 3 years. Her recent US showed multiple small submucosal fibroid. What is the best method of contraception for her?
Correct Answer : C
IUS gives 3-5 yrs long contraception. It also helps to shrink the fibroid. IUS is contraindicated if fibroids distord the uterine cavity but if not distorted as here with small fibroids it is still the contraception of choice.
Q.220. A lady presents with abdominal pain, dysuria, dyspareunia and vaginal discharge. What is your next step in management?
Correct Answer : B
High vaginal swab.
Probable diagnosis is PID.
Q.221. A 28-year-old pregnant woman with polyhydramnios and SOB (shortness of breath) comes for an anomaly scan at 31 weeks. US absence of gastric bubble. What is the most likely diagnosis?
Correct Answer : B
Oesophageal atresia
Q.222. A 20-year-old pregnant 32 weeks by date presents to the antenatal clinic with history of painless vaginal bleeding after intercourse. Examination: P/A – soft and relaxed, uterus dates, CTG reactive. Choose the single most likely diagnosis?
Correct Answer : C
Placenta previa
Q.223. A 65-year-old presents with dyspareunia after sex. She has attained menopause. She complains of bleeding after sex. What is the most probably diagnosis?
Correct Answer : B
Endometrial carcinoma. In post menopausal women, vaginal bleeding is likely due to endometrial carcinoma.
Q.224. A 24-year-old primigravida who is 30 week pregnant presents to the labor ward with a history of constant abdominal pain for the last few hours. She also gives a history of having lost a cupful of fresh blood per vagina before the pain started. Abdominal examination: irritable uterus, CTG reactive. Choose the most likely diagnosis?
Correct Answer : B
Antepartum hemorrhage.
Though presentation indicates abruption placenta but abrutio placenta 2nd to pre-eclampsia can’t be the option as no features are suggestive of pre-eclampsia here. So better option is B. Antepartum hemorrhage which also includes abruption placenta. Only bleeding cannot indicate whether it is concealed, mixed or revealed.
Q.225. A primiparous woman with no previous infection with herpes zoster is 18 weeks pregnant. She had recent contact with a young 21 year old patient having widespread chicken pox. What is the most suitable management for the pregnant lady?
Correct Answer : D
If the pregnant woman is not immune to VZV and she has had significant exposure, she should be offered varicella-zoster immunoglobulin (VZIG) as soon as possible. VZIG is effective when given up to 10 days after contact (in the case of continuous exposures, this is defined as 10 days from the appearance of the rash in the index case). RCOG guidelines.
Q.226. What is the most appropriate antibiotic to treat uncomplicated chlamydial infection in a 21 year old female who isn’t pregnant?
Correct Answer : D
Doxycycline 100 mg twice daily for seven days or a single dose of 1 g of azithromycin or Erythromycin 500 mg twice daily for 14 days or four times daily for seven days or Ofloxacin 200 mg twice-daily or 400 mg once daily for 7 days.
In pregnant Azithromycine 1g single dose is recommended then erythromycin 500 mg twice daily for fourteen days or four times daily for seven days. Then amoxicillin 500 mg three times daily for 7 days.
Q.227. A 39-year-old woman has not had her period for 10 months. She feels well but is anxious as her mother had an early menopause. Choose the most appropriate initial investigation?
Correct Answer : B
Here serum oestrogen is also important as :
i) low oestrogen + low FSH + low LH suggest hypothalamic amenorrhoea and
ii) low oestrogen + high FSH + high LH suggest premature ovarian failure!
So the main determinant is serum FSH/LH.
The likely cause here is premature ovarian failure.
Q.228. A 23-year-old woman with painless vaginal bleeding at 36 weeks pregnancy otherwise seems to be normal. What should be done as next step?
Correct Answer : A
Painless vaginal bleeding at 36 weeks indicates the diagnosis of placenta previa, which can be better evaluated by vaginal US. Previously any vaginal procedure was not done in suspected placenta previa which has no longer found harmful now like vaginal ultrasound even in advanced pregnancy.
Q.229. A 24-year-old woman has 8 weeks amenorrhea, right sided pelvic pain and vaginal bleeding. She is apyrexial. Peritonism is elicited in the RIF. Vaginal examination reveals right sided cervical excitation.What is the most probable diagnosis?
Correct Answer : A
Patient with pelvic pain and vaginal bleeding, peritonism, and cervical excitation points towards Ectopic pregnancy.
Salpingitis, Endometriosis, and ovarian torsions are not associated with amenorrhoea.
In ovarian tumour three main features are :
i) Increased abdominal size and persistent bloating (not bloating that comes and goes)
ii) Persistent pelvic and abdominal pain
iii) Difficulty eating and feeling full quickly, or feeling nauseous.
Q.230. A 26-year-old woman with regular menses and her 28-years-old partner comes to the GP surgery complaining of primary infertility for 2 years. What would be the best investigation to see whether she is ovulating or not?
Correct Answer : D
Day 21 progesterone.
Mid-luteal progesterone level to assess ovulation: If low, it may need repeating, as ovulation does not occur every month. The blood test is taken seven days before the anticipated period, that is on day 21 of a 28-day cycle. However, this day will need to be adjusted for different lengths of cycle.
Q.231. A 23-year-old woman is being followed up 6 weeks after a surgical procedure to evacuate the uterus following a miscarriage. The histology has shown changes consistent with a hydatidiform mole. What is the most appropriate investigatigation in this case?
Correct Answer : D
The key is D. Serum B-HCG.
When you are first diagnosed with a hydatidiform mole, your hCG level will be raised. When the hydatidiform mole is treated (removed), the hCG level will usually return to a normal, non-pregnant amount and should remain so.
If you develop GTN (gestational trophoblastic neoplasia), the hCG level can remain elevated or continue to risefurther. So, this blood test is a good way to check for the possible development of GTN (Gestational trophoblastic neoplasia).
Q.232. A 28-year-old woman has been admitted at 38 weeks gestation. Her BP is 190/120 mmHg and proteinuria +++. Immediately following admission she has a grand-mal seizure. What is the most appropriate initial management?
Correct Answer : D
Magnesium sulphate IV.
The patient has established eclampsia. So she should be treated with Magnesium sulphate as with 4g magnesium sulfate in 100mL 0.9% saline IV over 5min + maintenance IV of 1g/h for 24h.
Beware depressed respiration. If recurrent seizure give 2g IVI magnesium sulfate over 5 min. Check tendon reflexes and respiratory rate every 15 minutes. Stop magnesium sulfate IVI if respiratory rate <14/min tendon reflex loss, or urine output <20mL/h.
Q.233. A 27-year-old woman had pre-eclampsia and was delivered by C-section. She is now complaining of RUQ (right upper quadrant) pain different from wound pain. What investigation will you do immediately?
Correct Answer : B
In a post ceasarian patient having pre-eclampsia RUQ pain different from wound pain points towards the diagnosis of HELLP syndrome. So immediate investigation to be done is LFT.
Q.234. A 34-year-old female presents with a foul smelling discharge. What set of organisms are we looking for to be treated here?
Correct Answer : D
Here smelling discharge is caused by gardenella. So the most acceptable answer is E. Gardenella only.
Q.235. A 39-year-old woman will undergo tubal sterilization and she wants to know the failure rate of this type of sterilization.
Correct Answer : B
The key is B. 1:200
Q.236. A patient with previous history of HTN (hypertension), the membranes have ruptured and the cervix is 3 cm dilated. 4 hours later on examination showed that the cervix was still 3 cm dilated. What is the single appropriate management for her labor?
Correct Answer : D
IV syntocinon drip. There is no progress of labour in 4 hours. Hence syntocinon drip should be given.
Q.237. A 27-year-old waitress has pelvic pain, dysmenorrhea and increasingly heavy periods. She also complains of dyspareunia. There is generalized pelvic tenderness without peritonism. Pelvic US is normal. What is the most likely diagnosis?
Correct Answer : C
Pelvic congestion syndrome.
In pelvic congestion syndrome there develops varicose veins in the lower abdomen from prolonged standing (as occurred here in a waitress who remains standing for long) with some pain syndromes like pelvic pain, dysmenorrea, dyspareunia and generalized pelvic tenderness without peritonism. Also there may be associated menorrhagia.
Q.238. A 14-year-old girl is clinically obese. She has not started her periods yet and has severe acne. Among her investigations, a high insulin level is found. What is the most probable diagnosis?
Correct Answer : D
It is not Cushing’s as insulin levels in Cushing’s are not usually raised! Here obesity, primary amenorrhea, acne, and a particularly high level of insulin make the likely diagnosis of PCOS.
Q.239. An 18-year-old girl with primary amenorrhea complains of severe abdominal pain every 4-8 weeks which is now getting worse. Examination: lower abdominal mass is felt. What is the most probable diagnosis?
Correct Answer : C
Hematometrium. Primary amenorrhea and periodic pain indicate hematometrium either secondary to imperforated hymen or vaginal septum.
Q.240. A 32-year-old woman P3 of 39 weeks gestation reports having spontaneous ROM (rupture of membrane) 4 days ago. She didn’t attend the delivery suite as she knew that would happen and had already decided on a home birth. Today she feels very hot and sweaty. She thought that she was starting to have labour pains but she describes the pain as more constant. Exam: uterus is tender throughout. Blood tests show raised CRP and WBC. Select the most likely diagnosis?
Correct Answer : B
Prolonged rupture of membrane can lead to chorioamnionitis.
Q.241. A 42-year-old overweight smoker comes with heavy periods. A scan reveals a normal uterus. She would like a long term treatment with minimal side effects that would offer treatment for the menorrhagia and provide contraception. She is unsure whether she would like more children. She is adamant that she doesn’t want surgery as she is terrified of the prospect. Select the best management for her menorrhagia?
Correct Answer : C
IU/systemic progesterone.
As the patient is a smoker, COCP should be avoided. Copper-containing IUCD worsens bleeding. In the given case option C. i.e.mirena is most suitable.
Q.242. You are called to see a 20 year old woman 2 hour post-LSCS (lower segment cesarean section). She has not passed urine since her operation. She denied any urinary symptoms preoperatively. Examination: appears unwell, temp 37.5C, BP 94/73 mmHg, pulse 116 bpm, saturation 97%. Her abdomen is distended with tenderness in the left flank and suprapubic region. Bowel sounds are not audible. What is the most appropriate post caesarean section complication for this lady?
Correct Answer : B
Urinary tract injury
Q.243. A 40-year-old teetotaler woman is recovering from a hysterectomy 2 days ago. At night she becomes agitated and complains of seeing animals and children walking around the ward. What is the most likely diagnosis?
Correct Answer : B
Toxic confusional state. This is not delirium tremens as the women is a teetotaler.
Q.244. A 28-year-old woman who is 32 weeks pregnant in her 3rd pregnancy is diagnosed as a case of placental abruption. After all the effective measures, she is still bleeding. What is the underlying pathology?
Correct Answer : A
Clotting factor problem
Q.245. A 28-year-old pregnant lady presents with severe lower abdominal pain with excessive per vaginal bleeding at 34 weeks of gestation. What should be the initial investigation of choice?
Correct Answer : B
Likely case of abruption placenta (as excessive bleeding probably revealed type) for which initial investigation of choice is US abdomen. Other features that will favour abruption are a hard uterus and evidence of fetal distress. It will be difficult to feel the fetal parts.
Q.246. A 33-year-old female presents with sudden severe colicky abdominal pain in her RIF (right iliac fossa). A mobile mass is felt on examination. What is the most likely diagnosis?
Correct Answer : C
Ovarian torsion
Q.247. A 35-year-old primigravida post Cesarian-section complains of inability to void. She denies dysuria but complains of fullness. She was treated with an epidural for analgesia. What is the most appropriate investigation?
Correct Answer : B
C. US KUB. It is also correct!
This is a case of POUR (post-operative urinary retention). We should do the US to know the urinary volume (urine volume in bladder). If <400ml we shall observe. When volume is >600ml we should do catheterization.
Q.248. A 53-year-old lady presents with hot flash and night sweats. Her LMP was last year. She had MI recently. What is the most appropriate management for her?
Correct Answer : D
Clonidine. COCP is absolutely contraindicated in recent MI patients.
Q.249. A young girl presented to OB-GYN assessment unit with lower abdominal pain and per vaginal bleeding after a history of hysterosalpingograph as a part of her infertility treatment. Observation: BP 90/50 mmHg, pulse 120 bpm, exam revealed rigid abdomen. What is the most appropriate next investigation?
Correct Answer : C
Likely cause of bleeding and shock is ruptured fallopian tube for which appropriate next investigation is US abdomen.
Q.250. A 21-year-old woman who is on COCP had to take azithromycin. What should be advised for her contraception?
Correct Answer : D
No extra precaution. Before it was thought that antibiotics like azithromycin reduce the efficacy of COCP. But later it was established that practically no significant changes occurred so no need for any extra precaution.
Q.251. Pregnant lady had her antenatal screening for HIV and Hep B. What other antenatal infections should she be screened for?
Correct Answer : A
Rubella and syphilis
Q.252. A 26-year-old lady came with abdominal pain, vaginal discharge and low grade fever. What is the most likely diagnosis?
Correct Answer : B
Acute PID (Pelvic inflammatory disease)
Q.253. A 26-year-old lady presents with high fever, lower abdominal pain and purulent vaginal discharge. She looks very unwell. What is the most appropriate management?
Correct Answer : C
IV Ceftriaxone 2g with doxycycline 100mg. The disease is severe needing inpatient management with IV Ceftriaxone 2g + IV doxycycline 100 mg.
Q.254. A 39 weeks pregnanct woman came to labor suite 3 days after an obstructed labour presents with pain and swelling of one leg. Exam: leg has blue mottling and is cold. What is the diagnosis?
Correct Answer : C
Embolus
Q.255. A 28-year-old lady presents with dyspareunia and dysmenorrhea. She is very obese. She now wants reversible contraceptive method. Which of the following will be most suitable for her?
Correct Answer : A
Mirena has beneficial effects on both dyspareunia and dysmenorrhea but with some degree of weight gain (nearly 3.1 kg after 5 years of use which is less than weight gain with other methods like depot provera (8.2 kg) and 4.9 kg with copper IUD.
Q.256. A young lady who is 28 weeks pregnant presents with vaginal bleeding. She has lost about 200 ml of blood. Examination: uterus is tender. Resuscitation has been done. What is the most important investigation to establish the diagnosis?
Correct Answer : A
Antepartum hemorrhage. The most important investigation to establish the diagnosis is US.
Q.257. A 32-year-old woman wants reversible form of contraception. She has one child delivered by emergency C-section. She also suffers from migraine and heavy periods. What is the most suitable form of contraception for this lady?
Correct Answer : C
IUCD
Q.258. A 27-year-old lady after C-section developed epigastric pain after 8 hours. What is the appropriate investigation?
Correct Answer : C
Epigastric pain is a warning sign of HELLP syndrome. So to rule out HELLP syndrome Liver enzymes should be done.
Q.259. An 8 weeks pregnant lady is brought to the emergency department due to severe vomiting. She was administered IV fluids and oral anti-emetics. She still can’t tolerate anything orally. What is the next best treatment?
Correct Answer : B
If oral antiemetics are not tolerated IV antiemetics are tried.
Q.260. A patient came with dyskaryosis to the OPD. She is a heavy smoker and alcoholic. Cervical smear shows abnormal cells. What is the best advice for her?
Correct Answer : A
Colposcopy. Patient with dyskaryosis should go for colposcopy.
Q.261. A lady came for OB-GYN assessment unit with history of 8 weeks pregnancy and bleeding per vagina for last 2 days. On bimanual examination, uterus 8 weeks in size. On speculum examination, cervical os is closed. How do you confirm the viability of the fetus?
Correct Answer : A
Viability of the fetus is better assessed with transvaginal The US. TVU can be done throughout pregnancy even if there is vaginal bleeding. It should be avoided once the membrane is ruptured to avoid the chance of fetal infection.
Q.262. A 21-year-old female in her first pregnancy at 38 weeks was brought to the emergency department with generalized tonic clonic seizure. IV MgSO4 was given but fits was not controlled. She is having fits again. What is the most important immediate management of this patient?
Correct Answer : D
Treat a first seizure with 4g magnesium sulfate in 100mL 0.9% saline IV over 5min + maintenance IVI of 1g/h for 24h. Beware of respiration. If recurrent seizure give 2g IVI magnesium sulfate over 5 min.
Check tendon reflexes and respiratory rate every 15min. Stop magnesium sulfate IV if respiratory rate <14/min or tendon reflexloss, or urine output <20mL/h.
Have IV calcium gluconate ready in case ofMgSO4 toxicity: 1g (10mL) over 10 min if respiratory depression. Use diazepam once if fits continue (eg 5–10mg slowly IV). If seizures continue, ventilate and consider other causes.
Q.263. A 24-year-old lady with BMI 30 complains of facial hair growth and history of amenorrhea. FSH 10.9, prolactin 400 IU, estradiol 177.8 mmol/l, progesterone normal, LH 33.2. What is the most probable diagnosis?
Correct Answer : A
Clinical features : obesity, hirsutism, amenorrhea, etc are consistent with PCOS. We know in PCOS LH: FSH ratio is 2:1 or 3:1. Here LH is 33.2 and FSH is 10.9 which also supports the diagnosis of PCOS.
Q.264. A lady comes with a missing IUCD thread. Her LMP was 2 weeks ago. What is the most appropriate next step in management?
Correct Answer : D
LOST THREAD: First confirm the thread is not in position by vaginal examination. If not present ultrasound should be arranged to locate the device.
If ultrasound does not locate the device and there is no definite history of expulsion then abdominal X-ray should be performed to look for an extrauterine device. Expulsion should not otherwise be assumed. Hysteroscopy can be helpful if ultrasound is equivocal. Surgical retrieval of an extrauterine device is advised.
Q.265. A 32-year-old woman presents with history of lower abdominal pain and vaginal discharge. She had her menses 4 weeks ago. She has a temp of 38.6C. What is the most suitable diagnosis?
Correct Answer : B
Acute PID. Fever, lower abdominal pain, and vaginal discharge are features of PID.
Q.266. A 40-year-old female was on COCP which she stopped 6 months ago. But she has not had her periods since then. Labs: FSH 22, LH 24, prolactin 700, estradiol 80. What is the most appropriate diagnosis?
Correct Answer : D
Premature ovarian failure.
FSH and LH are raised in ovarian failure; an FSH level 20 IU/l in a woman aged around 40 with secondary amenorrhoea indicates ovarian failure. In POF there is also a mild to moderate rise in prolactin.
Q.267. A 37-year-old lady stopped taking COCP 18 month ago and she had amenorrhea for 12 month duration. Laboratory findings: FSH 8, LH 7, prolactin 400, estradiol 500. What is the cause?
Correct Answer : D
Post pill amenorrhea.
Post pill amenorrhea= failure to resume menses within 6 months of stopping pill, she was amenorrheic for 12 months.
Q.268. A patient presents with mild dyskaryosis. 1 year ago smear was normal. What is the most appropriate next step?
Correct Answer : D
Colposcopy.
In mild dyskaryosis colposcopy should be done with HPV (human papilloma virus) test.
Q.269. A patient presents with mild dyskaryosis. 1 year ago smear was normal. What is the most appropriate next step?
Correct Answer : D
Colposcopy.
In mild dyscariosis, colposcopy should be done with HPV test.
Q.270. An African lady presents with heavy but regular periods. Her uterine size correlates to 14 weeks pregnancy. What is the most appropriate diagnosis?
Correct Answer : C
Fibroids.
Regular heavy menstruation in a uterus of 14 wk size is highly suggestive of fibroid.
Q.271. A 29-year-old at 38 weeks GA presents with a 2 hour history of constant abdominal pain. She then passes 100ml of blood per vagina. What is the next appropriate investigation?
Correct Answer : A
Clinical case of abruption placenta. If patient is not in labour serial USS for fetal growth should be performed as in present case. If patient is in labour CTG.
Q.272. A 26-year-old woman had amenorrhea for 10 weeks and is pregnant. She experiences hyperemesis. Now she presents with vaginal bleed. Examination: uterus 16 weeks, closed os. What is the most probable diagnosis?
Correct Answer : D
Molar pregnancy.
In hydatidiform mole uterus becomes more in size than the actual gestational age and due to the production of a large amount of gonadotrophin by moles patient suffers from severe vomiting i.e. hyperemesis. There also occurs vaginal bleeding.
Q.273. A pregnant woman of G2, GA 11 weeks presents with heavy vomiting, headache and reduced urine output. Urine analysis shows ketonuria. Choose the next best step?
Correct Answer : D
IV fluids.
Hyperemesis gravidarum with oliguria and ketonuria. IV fluid should be started to prevent renal failure.
Q.274. A patient had inflammatory changes on cervical smear. There is no vaginal discharge, no pelvic pain and no fever. What is the next step?
Correct Answer : A
Repeat smear in 6 months.
Q.275. A 37-years-old infertile lady with 5 cm subserosal and 3 cm submucosal fibroid is trying to get pregnant. Which is the most suitable option?
Correct Answer : C
Myomectomy.
Fibroids are preventing from her being pregnant. So myomectomy is the most suitable option to let her get pregnant.
Q.276. A woman who is on regular COCP presented to you for advice on what to do as she has to now start to take a course of 7 days antibiotics. What would you advice?
Correct Answer : A
Continue regular COCP.
Before it was thought that antibiotics alter the gutflora and ethinyloestradiol is not conjugated. There is more ethinyl oestradiol passed in the stool. So pregnancy and breakthrough bleeding can occur. But later it was established that thechanges of gut flora are usually negligible for COCP conjugation to occur and hepatic enzymeinduction may be a more relevant reason.
But it was also proved that for strong enzyme inducerlike Rifampicin and Rifabutin, there may need extra protection but other antibiotics practicallydoes not reduce the potency of COCP and hence excepts only drugs like rifampicin or rifabutin forother antibiotics no additional precautions are needed.
Q.277. A lady presents with hot flashes and other symptoms of menopause. What is the treatment option?
Correct Answer : B
HRT
Q.278. A 28-year-old woman at 34 weeks GA (gestational age) for her first pregnancy attends antenatal clinic. Her blood results: Hgb 10.6, MCV 95, MCHC 350. What do you do for her?
Correct Answer : D
Explain this is physiologic hemodynamic anemia.
According to NICE, cut offs for iron supplements: at booking (8-10 weeks)- if less than 11 at 28 weeks and further- if less than 10.5 if less than these values=> give iron.
Q.279. A 34-year-old woman who never had fits or high BP developed fits 6 hours after delivery of a term healthy child. What is the most likely diagnosis?
Correct Answer : A
In eclampsia seizers occur within 24 hours mostly and the majority within 12 hours. Also, single seizure doesn’t support epilepsy strongly. So the likely answer is Eclampsia.
Q.280. A-30-year old lady who already has one child through a previous C-section demands a reversible contraception. She presently experiences heavy and painful periods. What is the most appropriate contraceptive you will recommend for her?
Correct Answer : D
Mirena
Q.281. A 32-year-old woman comes with intermenstrual bleeding. Her last cervical smear was 1 year ago and was negative. What test would you recommend for her initially?
Correct Answer : C
Endocervical swab.
Smear can only be done if it is due or overdue, not at any time, or not on an as-needed basis. Here patients next smear will be due after 2 more years. In reproductive years cervisitis due to infection particularly with chlamydia is very common. So initially we shall take an endocervical swab to rule out infection.
Q.282. A 20-year-old woman has had abdominal pain in the LIF (left iliac fossa) for 6 weeks duration. Over the past 48 hour, she has severe abdominal pain and has a fever of 39.1C. Pelvic US shows a complex cystic 7 cm mass in the LIF. What is the most likely diagnosis?
Correct Answer : D
Tubo-ovarian abscess
Q.283. A woman is 16 weeks pregnant and she is worried about abnormal chromosomal anomaly in her child. What is the definitive investigation at this stage?
Correct Answer : A
Amniocentesis is done between 14 to 16 weeks of gestation. CVS is done prior to 15 weeks. So the option is Amniocentesis.
Q.284. A 39-year-old woman in her 36th weeks of GA (gestational age) with acute abdominal pain is rushed for immediate delivery. Her report: BP 110/60 mmHg, Hgb low, bilirubin 22, AST 35, Platelet count 60, APTT 60, PT 30, Fibrinogen 0.6. What is the cause?
Correct Answer : B
It is not HELLP syndrome as the liver enzyme is not elevated. Acute abdominal pain may indicate concealed abruption placenta which may lead to DIC.
Q.285. A 36 weeks pregnant woman presents with sudden onset of uterine pain and bleeding, uterus is tender, no previous LSCS. What is the most appropriate cause?
Correct Answer : C
Painful bleeding at 36th week is placental abruption (either revealed or mixed type).
Q.286. A 28 weeks pregnant woman presents with uterine bleeding after sexual intercourse. What is the most appropriate cause?
Correct Answer : C
Post coital bleeding can be either placenta previa or cervical ectropion. But as ectropion is commoner in pregnancy it is the option here.
Q.287. A 6 weeks pregnant woman presents with abdominal pain. She has previous history of PID. What is the most likely diagnosis?
Correct Answer : D
PID is a recognized risk factor for ectopic pregnancy. Also, pain without bleeding at the 6th week supports the diagnosis of ectopic pregnancy.
Q.288. A 33 weeks pregnant woman presents with vaginal bleeding, low Hgb, low platelet, increased bilirubin, AST normal, APTT & PT increased. What is the most likely diagnosis?
Correct Answer : B
DIC
Q.289. A 25-year-old lady at her 28th weeks of GA (gestational age) came for check up. Her BP is 160/95 mmHg, protein in urine is 6 g/d. What is the most likely diagnosis?
Correct Answer : D
Preeclampsia
Q.290. A 32-year-old woman has a history of spontaneous abortions at 6 weeks, 12 weeks, and 20 weeks. She is now keen to conceive again. Which of the following would you prescribe for the next pregnancy?
Correct Answer : B
Patient of antiphospholipid syndrome had 3 fetal losses and no thromboembolic event and now wants to be pregnant. In such cases prophylactic treatment with low-dose aspirin is indicated.
Q.291. A 42-year-old woman who smokes 20 cigarettes/day presents with complains of heavy bleeding and prolonged menstrual period. What is the most appropriate treatment for her?
Correct Answer : A
Tranexamic acid
Q.292. A 17-year-old senior school girl with complain of prolonged irregular menstrual period and heavy blood losses. What is the most appropriate treatment for her?
Correct Answer : B
In irregular periods: COCP except the contraindications for it and in that case POP should be used.
Q.293. A 32-year-old presents with heavy blood loss, US (ultrasound): uterine thickness >14 mm. What is the most appropriate treatment for her?
Correct Answer : D
IU system (Mirena).
Simple endometrial hyperplasia without atypia responds to high-dose progestogens, with repeat histology after three months. This can be effectively delivered by the levonorgestrel intrauterine system (IUS).
Q.294. A 37-year-old woman presents with heavy bleeding. Investigation show subserosal fibroid 4cm and intramural fibroid 6cm. Which is the most appropriate treatment?
Correct Answer : D
Abdominal myomectomy.
As the patient is young we should go for myomectomy. Hysteroscopic myomectomy is suitable for mainly submucosal fibroids. We should go for Abdominal myomectomy which will deal with both subserosal and intramural fibroids.
Q.295. A woman with sickle cell disease complains of heavy menstrual blood loss. What is the most appropriate treatment?
Correct Answer : C
Depot provera.
Hormone and barrier methods are all acceptable choices but intrauterine devices are not recommended, as they may be associated with uterine bleeding and infection. Depot contraceptives (Depo-Provera) are safe and have been found to improve the blood picture and reduce pain crises.
Q.296. A 17-year-old girl comes to see her GP after having unprotected sex 2 days ago. She asks if her GP can explain to her how this prescribed procedure would work by helping her not to get pregnant.
Correct Answer : B
It helps in preventing or delaying ovulation.
There are two types of pills:
1. 1.5 mg of levonorgestrel pill : It should be taken within 72 hours (three days). It is thought to work mainly by preventing or delaying the release of an egg from your ovary, which normally happens each month (ovulation).
2. Ulipristal acetate is a type of emergency contraceptive pill. It is taken as one single tablet. Take the pill as soon as possible after unprotected sex. The earlier you take the pill, the more effective it is.
It can be taken up to 120 hours (five days) after having unprotected sex. It is a type of hormone that seems to work by stopping or delaying the release of an egg (ovulation). IUCD prevents implantation. As she is sexually active hymen is ruptured and IUCD can be given to her. But with IUCD chance of ectopic pregnancy is much more!
Q.297. A 16-year-old girl who is normally fit and well attends her GP complaining of heavy and painful periods. She is requesting treatmen for these complaints. She denies being sexually active. Select the most appropriate management for her menorrhagia?
Correct Answer : D
NSAIDs (mefenamic acid).
NSAIDS are first-line if there is dysmenorrhea and also very effective for menorrhagia and considered as potent as tranexamic acid in controlling menorrhagia.
Q.298. A 36-year-old woman came with uterine bleeding. Vaginal US reveals uterine thickness 12 mm. What is the most probable diagnosis?
Correct Answer : B
Endometrial Ca.
Actually, there is endometrial thickening and in general, 12 mm means hyperplasia which may suggest endometrial Ca in this woman.
Q.299. A 30-year-old woman has PID (pelvic inflammatory disease) which was treated with metronidazole and cephalosporin. It is getting worse. What is the next best investigation?
Correct Answer : B
US. Probable tubo-ovarian abscess.
Q.300. A pregnant patient with Rh –ve who hasn’t been previously sensitized delivers her first baby without any problem. What would be the latest time to administer antisensitization?
Correct Answer : D
72h PP (72 hours postpartum).
Q.301. A 30-year-old primigravida who is in her 30th weeks of GA (gestational age) presents to the L&D (labour and delivery unit) with absent fetal movements. She also complains of severe headache, heartburn and seeing floaters before her eyes for the last few days. Examinations: BP 170/110 mmHg, urine protein ++++, rock hard uterus, no visible signs of fetal movements. What's the most likely diagnosis?
Correct Answer : A
Abruption of placenta 2nd pre-eclampsia and IUFD. Both are correct!
Q.302. A 38-year-old woman, 10 days post partum, presents to her GP with a history of passing blood clots per vagina since yesterday. Examinations: BP 90/40 mmHg, pulse 110 bpm, temperaturex6 38C, uterus tender on palpation and fundus is 2cm above umbilicus, blood clots +++. What's the most likely diagnosis?
Correct Answer : D
Secondary PPH.
Secondary PPH occurs from 24 hours after delivery. Usually occurs between 5 and 12 days.
Q.303. A 22-year-old lady who is in her last trimester of pregnancy comes with history of exposure to a child diagnosed with chicken pox 1 day ago. She was investigated and was +ve for varicella antibody. What is the most appropriate management?
Correct Answer : D
Reassure.
If you have antibodies in your blood, this means you have had chickenpox in the past, or have been immunised. No further action is then needed.
Q.304. A 22-year-old woman who is 20 weeks pregnant came with pain and bleeding per vagina. Examination: os is not open. What is the most likely diagnosis?
Correct Answer : A
Threatened abortion
Q.305. A 32-year-old lady G1 (gravida 1), 28 weeks GA (gestational age) came to her ANC (antenatal care) with a concern about pain relief during labour. She has no medical illnesses and her pregnancy so far has been uncomplicated. She wishes to feel her baby being born but at the same time she wants something to work throughout her labour. What method of pain relief best matches this lady’s request?
Correct Answer : C
Entonox.
This is a mixture of oxygen and nitrous oxide gas. Gas and air won't remove all the pain, but it can help to reduce it and make it more bearable.
Q.306. A primipara at fullterm in labor has passed show and the cervix is 3 cm dilated. What is the most appropriate management for her labor?
Correct Answer : A
Repeat vaginal examination in 4h.
Q.307. A woman comes to the emergency department complaining of pain in the right side of the abdomen, she has 7 weeks amenorrhea. Her pregnancy test is +ve and US scan shows an empty uterus. What is the next step?
Correct Answer : A
Laparoscopy.
Surgery should be offered to those women who cannot return for follow up after methotrexate or to those who have any of the following:
• Significant pain
• Adnexal mass 35 mm
• Fetal heartbeat visible on a scan
• Serum hCG level 5000 IU/L
A laparoscopic approach is preferable. A salpingectomy should be performed unless the the woman has other risk factors for infertility, in which case a salpingotomy should be undertaken.
If HCG >6000IU/L and an intrauterine gestational sac is not seen on the trans-abdominal US, ectopic pregnancy is very likely, as is the case if HCG 1000–1500IU/L and no sac is seen on transvaginal ultrasound.
Q.308. A 68-year-old woman presents with post-coital bleeding following her first episode of sexual intercourse in 10 years. What is the most likely cause that has led to post-coital bleeding?
Correct Answer : B
Atrophic vaginitis
Q.309. A 28-year-old woman 8 weeks GA (gestational age) had PID (pelvic inflammatory disease) treated previously and now comes with vaginal bleeding, rigid abdomen, BP 80/50 mmHg, pulse 140 bpm. What is the most probable diagnosis?
Correct Answer : D
Tubal pregnancy.
Previous PUD is a risk factor for tubal pregnancy. The presented case is a case of ruptured ectopic pregnancy as there is vaginal bleeding, rigid abdomen, and shock.
Q.310. A 24-year-old woman has had lower abdominal pain for 12 hours. She is otherwise well. She is at 10 weeks GA (gestational age) in a planned pregnany. What is the most appropriate test to investigate the cause of acute abdomen in this lady?
Correct Answer : D
Transvaginal US.
D/D: ectopic pregnancy, renal colic, torsion of ovarian cyst, appendicitis, etc. The transvaginal US will give better results in case of lower abdominal pain.
Q.311. An 8-weeks pregnant woman presents with persistent vomiting and weight loss. Examination: HR(heart rate) 110 bpm. Dehydration was corrected with NS infusion and K+. The condition didn’t improve so IM cyclizine was given. She is still vomiting. What is the next appropriate management?
Correct Answer : B
IV antiemetics may be tried in patients of hyperemesis gravidarum not responding to IM antiemetics.
Q.312. A patient is at term and in labour, the membranes have ruptured, the liquor contains meconium but the CTG is normal. The cervix is 3 cm dilated. What is the most appropriate action?
Correct Answer : B
Till CTG is normal we should not switch to other options but continuing CTG. If CTG shows fetal distress then we have to do fetal scalp blood sampling to make the decision about probable cesarean section. (Only abnormal CTG is not enough to take a decision of cesarean section).
Q.313. A patient is at term and labor. The head has been delivered and you suspect shoulder dystocia. What is the most appropriate action?
Correct Answer : B
Episiotomy
Q.314. A 29-year-old female at 28 weeks of GA (gestational age) presents to you with complains of hard stools and constipation for last 2 weeks. CTG shows fetal tachycardia. What is the most appropriate treatment?
Correct Answer : B
Fiber diet.
Changes to diet and lifestyle are often recommended as the first treatment for constipation. It includes a high-fiber diet and plenty of fluid, regular exercise, etc.
Q.315. A 16-year-old girl presents with heavy bleeding. What is the most appropriate initial investigation?
Correct Answer : D
Pelvis US
Q.316. A woman who is 7 weeks pregnant presents with excessive and severe vomiting and put on IV fluids and anti-emetic (ondansteron). She is complaining of severe headache and can’t take oral fluids. What is the most appropriate management?
Correct Answer : D
IV hydrocortisone.
Termination is the last resort! Before it, IV hydrocortisone is tried. 1st oral antiemetics if parenteral antiemetics if fail iv hydrocortisone. The last resort is termination.
Q.317. A young lady with primary amenorrhea has normal LH, FSH, estradiol and prolactin. Choose the most likely diagnosis?
Correct Answer : C
Absent uterus.
Normal LH, FSH, estradiol, and prolactin rule out PCOS; increased LH, increased FSH, normal oestrogen, LH: FSH ratio is 2:1 or 3:1
In POF, LH & FSH raised, FSH > 20 IU/L,
Absent ovary will lead to low estradiol, high FSH, and LH.
Turner’s syndrome: gonadal streaks, and absent ovaries.
Q.318. An obese lady presents with primary amenorrhea. She has high LH, normal FSH and slightly high prolactin levels. Choose the most likely diagnosis?
Correct Answer : A
High LH, high or normal FSH with slight rise in prolactin levels in an obese lady is suggestive of PCOS.
Q.319. A 38-year-old lady presents with amenorrhea has very high LH and FSH levels, normal prolactin and low estradiol. Choose the most likely diagnosis?
Correct Answer : B
High LH and FSH, normal prolactin, and low estrogen in secondary amenorrhea in a lady under age 40 is highly suggestive of POF.
Q.320. A 65-year-old lady presents with dyspareunia. What will you give for her condition?
Correct Answer : C
Estrogen gel.
Seems to be atrophic vaginitis for which estrogen gel can be given.
Q.321. A 35-year-old lady with subserosal fibroid 4cm and submural fibroid 6cm is planning for a child. How will you remove the fibroids?
Correct Answer : C
Abdominal myomectomy.
Subserosal fibroid is not suitable to treat through the vaginal route. Abdominal myomectomy can deal with both subserosal and submural fibroid.
Q.322. A 32-year-old presents with heavy blood loss. US (ultrasound): uterine thickness> 14 mm. What is the best possible management for her?
Correct Answer : B
UAE.
Either low-dose combination hormonal contraceptive treatment or progestin therapy is generally effective in women aged 19-39 years.
Q.323. A 30-year-old woman on OCP (oral contraceptive pill) presents with dilated tortuous veins crossing her abdomen to join the tributaries to SVC. What is the most likely cause?
Correct Answer : D
DVT.
IVCT (inferior vena cava thrombosis) is well known to occur secondary to DVT leading to dilated tortuous veins crossing the abdomen to join the tributaries to SVC.
Q.324. A 25-year-old primigravida of 8 weeks GA (gestational age) presents with severe lower abdominal pain, vaginal bleeding and passage of clots. The internal os is open. What is the most likely diagnosis?
Correct Answer : D
Abortion.
Up to 24 weeks termination of pregnancy is abortion.
Q.325. During antenatal visits, the following tests are routinely offered to all pregnant mothers apart from HIV and Hepatitis B?
Correct Answer : A
Rubella and syphillis
Q.326. A pregnant lady at her 39 weeks GA (gestational age) presents with eclampsia. Soon after her arrival in the labour suit, IV MgSO4 and IV hydralazine has been prescribed. The patient then develops another fit in the hospital and maintenance dose of MgSO4 has been started. What is your next step in management?
Correct Answer : A
Mg SO4
Q.327. A 19-year-old female diagnosed with trichomonas vaginalis. LMP (last menstrual period) was 10 days ago. What is the best antibiotic treatment?
Correct Answer : C
Metronidazole
Q.328. A 28-year-old woman comes with sudden onset vomiting and pain per abdomen. Examination: mobile swelling in the right iliac fossa. What is the most probable diagnosis?
Correct Answer : D
Ovarian torsion.
As there is no history of amenorrhea ectopic pregnancy is less likely. So dx is possible ovarian torsion.
Q.329. A 32-year-old woman with previous history of PID (pelvic inflammatory disease) now presents with severe abdominal pain. Her LMP (last menstrual period) was 8 weeks ago. What is the most probable diagnosis?
Correct Answer : A
Ectopic pregnancy.
PID is a risk factor for ectopic pregnancy.
Q.330. A 25-year-old who is 38 weeks pregnant presents to the labour ward with a history of fewer fetal movements than usual during the evening. She also says that abdominal contractions are coming every few minutes and she is having a blood stained show per vagina for the last few minutes. Examination: cervix is fully affaced, 9 cm dilated, cephalic presentation and station is +1. Choose the most likely diagnosis?
Correct Answer : C
Abdominal contractions coming every few minutes, having blood stained show per vagina, fully effaced cervix with dilatation of 9 cm, cephalic presentation and station +1 suggests that the patient is in labour.
Q.331. A young lady with cervical ectropion bleeds on touch. What is the most appropriate next investigation?
Correct Answer : D
Screening test cervical smear is only done at a scheduled time and not in on a demand basis. Also, a smear test is started at the age of 25 years. So if it is scheduled now then it can be the option otherwise Colposcopy should be done.
Q.332. A 35-year-old woman who usually has 4 days mid-cycle bleeding, had her period 10 days ago. She has now presented with spots of blood. Her smear was normal 6 months ago. Examination: cervical ectropion which doesn’t bleed on touch. What would you do?
Correct Answer : B
Infection is a recognized cause of intermenstrual bleeding and it should be ruled out doing endocervical swabs first.
Q.333. A young woman who is a marathon runner comes with secondary amenorrhea. Investigation: normal LH, FSH and estradiol, prolactin 600. What is the most likely diagnosis?
Correct Answer : D
Prolactinoma
Q.334. A 34-year-old pregnant woman with 38 weeks of GA (gestational age) is in labor. She had a long 1st stage and troublesome 2nd stage, has delivered a baby. After her placenta was delivered she had a convulsion. What is the most probable management?
Correct Answer : A
Eclampsia, treatment is with IV MgSO4.
Q.335. A 23-year-old woman presents with offensive vaginal discharge. Vaginal pH 4.5. What is the most likely organism?
Correct Answer : A
Gardenella
Q.336. A girl with sickle cell anemia has painful bleeding and vaso-occlusive crisis during her periods. What is the best possible management for this patient?
Correct Answer : D
Hormone and barrier methods are all acceptable choices but intrauterine devices are not recommended, as they may be associated with uterine bleeding and infection.
Depot contraceptive (Depo-Provera) is safe and has been found to improve the blood picture and reduce pain crises.
Q.337. An 18-year-old girl has menorrhagia and dysmenorrhea and requires contraception. What drug will you give her?
Correct Answer : A
COCP
Q.338. An obese woman with history of migraine presented with heavy bleeding during menstruation which is painful and needs contraception too. What is the best possible management for this patient?
Correct Answer : B
Mirena coil.
In migraine COCP should be avoided.
Q.339. A 43-year-old woman has suffered with heavy periods for many years and has tried many medical treatment without success. She is constantly flooding and at times can’t leave her house due to heavy bleeding. She has completed her family of 5 children and her last blood test showed Hgb=8.9g/dl. She feels that she can’t cope with the bleeding anymore and her husband is asking for a treatment that can guarantee success. What is the most appropriate management to improve menorrhagia in this patient?
Correct Answer : B
As family is complete hysterectomy is the best option to stop bleeding and it also helps not to get endometrial carcinoma.
Q.340. A 48-year-old nulliparous woman feels tired all the time. Her periods are regular but have always lasted for at least 10 days. Choose the most appropriate intial investigation?
Correct Answer : B
Serum Hb conc.
Feeling tired all the time and prolonged periods suggest anemia. So serum Hb should be done initially.
Q.341. A woman is admitted to the hospital for elective abdominal hysterectomy. 2 months ago she was diagnosed with DVT and pulmonary embolism and was started on warfarin. What is the most appropriate preoperative measure you will take on this occasion?
Correct Answer : C
Stop warfarin and start heparin.
Q.342. A 37-year-old woman had an elective LSCS (lower segment cesarean section) 1 day ago. You are called to see her as she becomes SOB (short of breath) with left sided chest pain and a cough. She has had 3 children, 2 born by LSCS. Examination: she has reduced air entry at left lung base. Her observations include saturation 92% on air, BP 105/84 mmHg, pulse 120 bpm, temperature 37.2C. Which C-section complications has she developed?
Correct Answer : D
Pulmonary embolism.
Absence of wheezing and near normal temperature makes aspiration as unlikely diagnosis and favours the diagnosis of pulmonary embolism.
Q.343. A 32-year-old woman of 38 weeks GA (gestational age) attends the antenatal day unit with pain in the suprapubic area that radiates to the upper thighs and perineum. It is worse on walking. Her urine dipstick showed a trace of protein but no white cells, nitrates or blood. What’s the most likely diagnosis?
Correct Answer : C
Symphysis pubis dysfunction.
Symptoms can include: pain over the pubic bone at the front in the center pain across one or both sides of the lower back pain in the area between the vagina and anus (perineum) Pain can also radiate to thighs.
Cause: stiffness of pelvic joints or the joints moving unevenly at either the back or front of the pelvis during pregnancy. Physiotherapy is helpful.
Q.344. A 30-year-old woman, G2P1 (gravida2, para1) at 37 weeks gestation mentions that her 3-year-old son has just developed chickenpox. She is not certain whether she has had the disease herself. Which is the next step in management?
Correct Answer : D
Measurement of varicella IgG level.
If previous infection is doubtful do varicella IgG level.
Q.345. A 24-year-old primigravida presents to the emergency department with a history of 8-weeks amenorrhoea followed by heavy vaginal bleeding and severe, crampy abdominal pain. Examination: HR 110/min and BP 120/80mmHg. The uterus is bulky. The cervix is dilated and there is active bleeding from the cervical os, but no tissue has been expelled. Which of the following is the most likely diagnosis?
Correct Answer : A
Inevitable abortion.
When os is closed threatened and when os is opened inevitable abortion (No tissue has been expelled).
Q.346. A 31-year-old woman, G5P4 (gravida5, para4), who has amenorrhoea for 12 weeks and a positive pregnancy test presents to the emergency department with vaginal bleeding. Symphysial-fundal height measurement corresponds to 22 weeks gestation. Ultrasound examination reveals bilateral cystic masses. No fetal parts are seen during the examination. The cervix is closed. What is the most likely diagnosis?
Correct Answer : C
Hydatidiform mole.
In molar pregnancy uterus is more enlarged than gestational age and in the US no fetal part but cystic masses are seen.
Q.347. A married 25-year-old woman presents with 6 hours history of abdominal pain located in the LIF. The pain is persistent, of increasing intensity and not radiating first experienced while she was lying down. She feels giddy when she tries to stand erect. The last menstrual period was 6 weeks ago. The radial pulse=130/min and BP=80/40 mmHg. Pelvic US shows free intra-peritoneal fluid. What is the most appropriate next step in management?
Correct Answer : B
Immediate laparotomy.
As the patient is in shock it is a ruptured ectopic pregnancy. So the next step is immediate laparotomy.
Q.348. A 32-year-old woman of 40 weeks gestation attends the antenatal day unit with sudden onset epigastric pain with nausea and vomiting. She is clinically jaundiced. Her biochemistry results show a raised bilirubin, abnormal liver enzymes, high uric acid and hypoglycemia. What’s the most likely diagnosis?
Correct Answer : A
Acute Fatty Liver of Pregnancy.
When jaundice is present in pregnancy, AFLP should be high on the differential. Pain, nausea, vomiting, jaundice, fever with elevated liver enzymes, and bilirubin are indicative of AFLP. Also can have elevated INR, TLC, and hypoglycemia.
Q.349. A 29-year-old woman presents to her GP with troublesome heavy periods. The medical treatment that she has tried have made little difference. She is known to have large uterine intramural fibroids. You confirm that she is currently trying for more children. Select the most appropriate management for menorrhagia in this patient?
Correct Answer : D
Myomectomy.
Chance of subsequent pregnancies are better after myomectomy.
Q.350. A 30-year-old woman had an IUCD inserted 8-9 months ago. Now on routine follow up the thread is missing. Uterine US showed no IUCD in the uterus. What is the best management?
Correct Answer : D
Pelvic XR.
Ultrasound should be arranged to locate the device. If ultrasound does not locate the device and there is no definite history of expulsion then an abdominal X-ray should be performed to look for an extrauterine device.
Q.351. A 28-year-old woman who has had a previous pulmonary embolism in pregnancy wishes to discuss contraception. She has menorrhagia but is otherwise well. What is the most suitable contraceptive method for this patient?
Correct Answer : C
Levonorgestrel Intra-Uterine System.
The woman has a history of thromboembolic disease, which essentially contraindicates COCP. LNG-IUS (Mirena) is the hormone-releasing device that is most suitable in this patient with thrombophilia and menorrhagia.
Q.352. A 27-year-old woman who takes the COCP has had painless vaginal spotting and discharge for 3 days. Her last menstrual period, which lasted four days, finished 10 days ago. Her last cervical smear two years ago was normal. Abdominal and vaginal examinations are normal apart from a mild ectropion with contact bleeding. What is the most appropriate initial investigation?
Correct Answer : C
Endocervical swab.
As her cervical smear and examination of abdomen and vagina are normal, next we have to exclude STD for which Endocervical swab should be taken.
Q.353. A 19-year-old woman has had progressive bilateral iliac fossa pain and dyspareunia for 3days. She has an offensive vaginal discharge and feels unwell and feverish. Her temp=39C. An initial antimicrobial regimen is commenced. What set of organisms are the most appropriate for the antimicrobial regimen to cover?
Correct Answer : C
Neisseria gonorrhoeae and Chlamydia trachomatis.
Q.354. A primigravida in the 17th week of her symptomless gestation is found, on US, to have evidence of placental tissue covering the cervical os. By the end of her pregnancy she is likely to develop?
Correct Answer : A
Placental migration.
In 90% of pregnancies, an initial low lying placenta will be pulled upwards by the growing uterus and assume a normal position in the upper segment. This phenomenon is referred to as Migration.
Q.355. An elderly lady with COPD has chronic SOB. She is listed for cataract extraction. What is the anaesthetic of choice?
Correct Answer : C
The key is C. Peribulbar lignocaine. The most used mode of anaesthesia in ophthalmic field is peribulbar lignocaine.
Q.356. A pregnant woman in an early stage of labour expresses the wish to have pain relief during labour. The anesthetist describes that if the patient wishes he can use medication as a local anesthetic to block the pain sensations of labour. Into which space should the local anaesthetic be normally injected?
Correct Answer : D
Epidural space
Q.357. A 31-year-old woman is anxious about slight per vaginal bleeding. She is 22 weeks pregnant and had similar complaints 2 years ago when she was on the pill. What is the most appropriate next investigation?
Correct Answer : D
Ultrasound localization of the placenta.
Low set placenta is drawn up with the age of pregnancy causing slight vaginal bleeding, which can be detected by ultrasound scan.
Q.358. A 20-year-old married woman presents to A&E with acute onset of lower abdominal pain. Her last menstrual period was 6 weeks earlier. She has pain radiating to the left shoulder. What is the most likely diagnosis?
Correct Answer : A
Ectopic pregnancy.
Often, the first warning signs of an ectopic pregnancy are light vaginal bleeding and pelvic pain.
If blood leaks from the fallopian tube, the patient may feel shoulder pain or an urge to have a bowel movement. Patients' specific symptoms depend on where the blood collects and which nerves are irritated.
Q.359. A 22-year-old woman who has had 2 terminations of pregnancy, reports that she is pregnant again. She has noted a small amount of watery brown discharge and is tender in right iliac fossa. What is the most likely diagnosis?
Correct Answer : D
Ectopic pregnancy.
Prior spontaneous abortions increase the risk of ectopic pregnancy. Also watery brown discharge and right iliac fossa tenderness suggests bleeding ectopic pregnancy.
Q.360. The time span over which a percentage of women with untreated CIN will develop cancer. What's the likely time-interval?
Correct Answer : D
30 years
Q.361. The age at which the peak incidence of cervical carcinoma develops. Choose the likely time-interval.
Correct Answer : D
65 years
Q.362. The interval for cervical smears to be taken in a woman treated I year previously for CIN. Choose the likely time-interval.
Correct Answer : B
12 months
Q.363. The timescale within which the 50% of the patients with recurrent disease will present, following treatment for stage IB cervical cancer. Choose the likely time-interval.
Correct Answer : D
30 years
Q.364. A 24-years-old gravida 4, para 3, presents with a painless unprovoked vaginal bleed of approximately 50 ml at 32 weeks gestation. She is generally well, but worried. What is the most appropriate next investigation?
Correct Answer : A
Ultrasound localization of placenta.
Oxygen saturation by pulse oximetry is one of the vital signs and is not considered a lab. investigation.
The given case is a case of APH and as the history of active bleeding or ongoing bleeding is not given and as the patient is stable and has no uterine activity and tenderness we shall then assess fetal heart sound.
If OK then ultrasound localization of the placenta is the next investigation.
If there is concern about fetal heart sound CTG should be done. Now if there was active bleeding or uterine activity or tenderness next investigation would be haemoglobin concentration, rhesus status, and if Rh negative Kleihauser test.
Q.365. A 25-years-old nullipara presents at 26 weeks gestation with slight postcoital bleeding. What is the most appropriate next investigation?
Correct Answer : D
Speculum examination.
To exclude any local source of bleeding. A sterile speculum examination can be performed safely before ultrasonographic evaluation of placental localization, but a digital examination should be avoided until placenta previa is excluded by ultrasonography.
Q.366. Following recurrent antepartum hemorrhage, investigation shows the fetus to be small for dates at 32 weeks. Conservative management is preferred. A 19-week fetal anomaly ultrasound scan confirmed normal placental localization. What is the most appropriate next investigation?
Correct Answer : D
Rhesus status
Q.367. A woman, whose previous pregnancy was complicated by iso-immunization, has vaginal spotting at 36 weeks in an otherwise normal pregnancy. What is the most appropriate next investigation?
Correct Answer : C
Ultrasound localization of placenta
Q.368. A married 52-years-old woman who has a family history of breast cancer has been experiencing mild discomfort for a few hours following intercourse for last month. She is worried about using hormones. What is the management plan?
Correct Answer : D
Vaginal lubricant
Q.369. A 45-years-old woman who has had a total abdominal hysterectomy and bilateral salpingo-oopherectomy for fibroids and menorrhagia complains of hot flushes, night sweats and mood swings. She has no other medical problems. What is the management plan?
Correct Answer : B
Oestrogen-only HRT.
In case of hysterectomy unopposed estrogen (estrogen without progesterone) that is oestrogen only HRT can be given.
Q.370. A 41-years-old woman complains of being unable to conceive for 2 years despite having regular unprotected sex. She complains of sweating all the time, frequent defecation and says this explains her loss in weight in recent weeks. She denied starving herself and says she has a very good appetite. HbAlc levels are 5%. What is the most likely diagnosis?
Correct Answer : B
Hyperthyroidism.
Thyroid disease can cause female infertility by resulting in anovulation (lack of ovulation) and menstrual irregularity, luteal phase defect, and hyperprolactinemia.
Q.371. A 28-years-old woman complains of infertility for 3 years. She has a low libido, and has put on a lot of weight. Her breasts are discharging. What is the most likely diagnosis?
Correct Answer : D
Hypothyroidism.
Hypothyroidism causes significant hyperprolactinemia which can lead to infertility, loss of libido and discharging breast. Hypothyroidism is a cause of weight gain.
Q.372. A 38-years-old complains of infertility and is otherwise healthy. She had been on Haloperidol treatment for a schizophreniform illness for last 6 years. She has a healthy 3 years old daughter. What is the most likely diagnosis?
Correct Answer : A
Hyperprolactinemia.
Antipsychotic induced hyperprolactinemia. In women, hyperprolactinemia inhibits gonadotrophin secretion (follicle-stimulating hormone (FSH) and luteinizing hormone (LH)), leading to menstrual dysfunction, and infertility due to anovulation. It also may cause galactorrhoea.
Q.373. A 31-years-old woman complains of abdominal pain, which seems to increase during her periods. Over the last year she has noticed difficulty in breathing and chest pain associated with occasional haemoptysis, following her periods. Her mother is asthmatic and she has eczema. She has been unable to conceive. On examination she is found to have an enlarged and tender uterus. Her BMI is just 20. What is the most likely diagnosis?
Correct Answer : B
Endometriosis.
Ectopic endometrial tissue is endometriosis. Commonly there is abdominal involvement which causes symptoms like abdominal pain dyspareunia, and infertility.
When in lung tissue may produce dyspnea, and hemoptysis, particularly during periods. One of the main complications of endometriosis is difficulty getting pregnant or not being able to get pregnant at all.
Q.374. A 21-years-old woman presents as an emergency with a 4 hours history of abdominal pain and bright red vaginal blood loss. She has not had a men- strual period for 9 weeks and had a positive home pregnancy test I week ago. On vaginal examination the uterus is tender and bulky. The cervical os is open. What is the most likely diagnosis?
Correct Answer : A
Inevitable miscarriage.
Inevitable miscarriage usually presents with heavy bleeding with clots and pain. The cervical os is open. The pregnancy will not continue and will proceed to incomplete or complete miscarriage.
Q.375. A 16-years-old woman presents with a sudden onset of severe right iliac fossa pain. On vaginal ultrasound examination a 6cm diameter echogenic cystic mass is seen inright fornix. What is the most likely diagnosis?
Correct Answer : D
Torsion of ovarian cyst.
When the egg is released during ovulation, the sac that held the egg should also disappear. If the egg does not leave the sac in the ovary or if the sac closes before dissolving, it can fill with fluid and form a cyst.
The cysts shrink or dissolve after ovulation. Sometimes a cyst can get large and burst or rupture. The larger the cyst, the more likely that ovarian torsion will occur. With ovarian torsion, the blood supply to the ovary can be blocked and permanently hurt the ovary.
Q.376. An 18-years-old student due to take her examinations, reports that she missed her period and that a pregnancy test is negative. She has worsening abdominal pain, which has been troublesome for 3 months. She is otherwise well. What is the most likely diagnosis?
Correct Answer : C
Normal pregnancy.
Missed abortion is painless. It is possible to get a false negative pregnancy test.
Q.377. A 27-year-old who conscientiously uses OC pill, has experienced intermittent breakthrough vaginal bleeding and malodorous discharge for several weeks. When examined she has pain over the lower abdomen, worse on the left. Her temperature is 39C and her white cell count is elevated. What is the most likely diagnosis?
Correct Answer : A
Pelvic inflammatory disease.
The current outpatient treatment recommendation is ceftriaxone 500 mg as a single intramuscular (IM) dose, followed by doxycycline 100 mg orally twice daily and metronidazole 400 mg twice daily for 14 days.
An alternative regime is oral ofloxacin 400 mg twice daily and oral metronidazole 400 mg twice daily for 14 days.
This is not recommended if the woman is at high risk of gonococcal PID because of increasing quinolone resistance of gonorrhoea. Levofloxacin may be used as a once -daily, convenient alternative to ofloxacin.
The current treatment recommendation for severely ill (pyrexia above 38°C, clinical signs of tubo-ovarian abscess, signs of pelvic peritonitis or pregnancy) patients is: Initial treatment is with doxycycline, single-dose IV ceftriaxone, and IV metronidazole, then change to oral doxycycline and metronidazole to complete 14 days of treatment.
There is no evidence-based recommendation for treatment in pregnancy, but an empirical regimen might include IM ceftriaxone plus oral or IV erythromycin, with the possible addition of oral or IV metronidazole 500 mg three times daily in clinically severe disease. Any risk of this regimen is justified based on the need to provide therapy and low risk to the fetus. IV therapy should be continued for 24 hours after signs of clinical improvement.
Q.378. A 34-year-old gravida 4, para 3 + I presents at 20 weeks with a grossly distended abdomen. She is dyspnoeic and complains of general abdominal discomfort. Abdominal USG shows the deepest pool of amniotic fluid to be I0 cm and a normal fetus. What is the management plan?
Correct Answer : C
Abdominal amniocentasis.
The given picture is of severe polyhydramnios supported by the deepest pool of amniotic fluid to be 10 cm. Deepest pool >8 cm is polyhydramnios and if <2 cm it is oligohydramnios.
Treatment at this stage is abdominal amniocentasis.
Q.379. A 24-year-old primi gravida presents at 36 weeks with abdominal discomfort and on examination her abdomen is found to be larger for dates. She is dyspnoeic and complains of indigestion and claims the abdomen has swollen to this size within a week. USG shows the fetus to be normal. What is the management plan?
Correct Answer : B
Do emergency cardiotocography.
Polyhydramnios. Usual recommendation is deliver at 37 weeks and if needed even a few weeks earlier.
Q.380. A 40-year-old lady 38 weeks pregnant is brought to A&E fitting. Prior to this she had complained of epigastric pain. Her BP is found to be 200/110 mmHg. What is the management plan?
Correct Answer : D
4-5 g IV MgSO4 + hypotensive.
Case of Eclampsia. Should be treated with MgSO4 and hypotensive.
Q.381. A 72-year-old woman has experienced of micturition intermittently for the last few months. Midstream urine cultures have been persistently negative. She is well otherwise, but would like her symptoms to be resolved. What is the management plan?
Correct Answer : B
Combined HRT.
Menopause can frequently produce UTI-like symptoms though there is no infection. For post-menopausal symptoms combined HRT is the treatment of choice for those who have uterus.
Q.382. A 34-year-old woman presents with malodorous discharge. A wet film smear shows ‘clue cells’. What is the most likely diagnosis?
Correct Answer : A
Bacterial vaginosis.
In a wet film smear, a sample of the vaginal discharge is placed on a glass slide and mixed with a salt solution. A wet prep is considered positive when more than 20% of the epithelial cells present in the microscopic field are clue cells. Clue cells are seen in bacterial vaginosis.
Q.383. A 28-year-old woman presents with a white curdly discharge from her vagina. Wet smear shows mycelium growth. What is the most likely diagnosis?
Correct Answer : C
Candidiasis.
Candidiasis is a fungal infection caused by a yeast (a type of fungus) called candida.
Candida causes the following symptoms in the case of vaginal candidiasis: pruritus vulvae, vulval soreness, white ‘cheessy’ discharge, dyspareunia and dysuria.
Treatment: Prescribe either an intravaginal antifungal, such as clotrimazole or miconazole pessaries, or an oral antifungal, such as fluconazole or itraconazole. If there are vulval symptoms, consider a topical imidazole as well (eg, clotrimazole or miconazole). Combination packs of pessary/vaginal cream and topical cream are available.
Q.384. A 28-year-old woman presents with lower abdominal pain, an offensive vaginal discharge and deep dysparenuia. She has no gonorrhea. What is the most likely diagnosis?
Correct Answer : C
Chlamydial pelvic infection
Q.385. A 31-year-old woman complains of a chronic non-foul smelling discharge. She bleeds after sexual intercourse. What is the most likely diagnosis?
Correct Answer : D
Cervical erosion can cause odorless vaginal discharge with post-coital bleeding.
Q.386. A 52-year-old woman had had a history of offensive vaginal discharge and intermittent vaginal bleeding over the past 3 months. Her last cervical smear was taken 4 years ago. What is the most relevant next examination?
Correct Answer : C
Endocervical swab.
The likely diagnosis is PID. Though cervical smear is overdue it is not the NEXT investigation as cervical screening doesn't include tests for chlamydia or other sexually transmitted infections (STIs), such as gonorrhea.
Q.387. A 23-year-old has a new sexual partner. She has been on the combined OC pill for last 6 years. She presents with a 2-month history of breakthrough bleeding. What is the most relevent next examination?
Correct Answer : A
Endocervical swab
Q.388. A 47-year-old woman who has breast cancer and is on tamoxifen has 2 episodes of bright red bleeding. Her last period was when she started tamoxifen 2 years ago. What is the most relevant next examination?
Correct Answer : C
Endometrial sampling.
Tamoxifen can cause endometrial carcinoma.
Q.389. A 26-year-old woman with a 5-week history of amenorrhoea presents to A&E with vaginal bleeding. An ultrasound scan report “empty uterus”. What is the most relevant next examination?
Correct Answer : B
Gonadotropin levels.
Probable ectopic pregnancy.
Q.390. A 49-year-old woman presents with a 9-month history of prolonged slightly irregular periods. Clinical examination shows a normal size uterus with no adnexal masses. What is the most relevant next examination?
Correct Answer : B
Endometrial sampling.
If it was an infection 9 months history would present with its complications which are not present here. Also, pattern of menstruation warns us to exclude endometrial cancer.
Q.391. A 56-year-old nulliparous woman with a BMI of 37 has a four month history of blood stained discharge. She is otherwise normal. What is the most likely diagnosis?
Correct Answer : C
Post menopausal blood-stained discharge is highly suggestive of endometrial carcinoma.
Q.392. A 23year old woman has been taking the combined oral contraceptive pill for 4 years. She has a troublesome clear, sticky discharge with no odour or itching. What is the most likely diagnosis?
Correct Answer : C
Oral contraceptive is a well-known cause of cervical ectropion. There may be an increase in vaginal discharge which is otherwise asymptomatic (no redness or plaque, no itching, no odor or other symptoms) in cervical ectropion.
Q.393. A 25-year-old woman is 8 weeks pregnant. She has experienced a degree of vaginal bleeding and severe left sided abdominal pain. Her pulse rate is 100 beats/minute and her BP is 110/75 mmHg. There is marked cervical excitation on vaginal examination. What is the most appropriate management?
Correct Answer : D
Culdocentasis.
In the given case diagnostic laparoscopy should be the answer but as it is not in the options we should go for the most appropriate investigation from the given options which is culdocentasis here.
As the patient is not in shock the diagnosis is not ruptured ectopic pregnancy yet but leaking ectopic pregnancy in which there occurs accumulation of blood in the pouch of Douglas which can be revealed by culdocentasis.
Q.394. A 30-year-old woman has IUCD inserted 8-9 months ago. Now on routine follow-up the thread is missing. Uterine ultrasound shows no IUCD in the uterus. What is the best management?
Correct Answer : D
Pelvic X-ray.
Management of Lost Thread: Ultrasound should be arranged to locate the device. If ultrasound does not locate the device and there is no definite history of expulsion then abdominal X-ray should be performed to look for an extrauterine device.
Expulsion should not otherwise be assumed. Hysteroscopy can be helpful if ultrasound is equivocal. Surgical retrieval of an extrauterine device is advised.
Q.395. A pregnant patient who’s Rh negative and has not has been previously sensitized delivers her first baby without complications. What would be the latest time to administer antisensitization?
Correct Answer : D
72 hours post partum
Q.396. A 60-year-old woman present with post coital bleeding for the past 1 week. What is the most appropriate investigation?
Correct Answer : C
Please note Red Flag Signs for Cancer (either cervical or endometrial) is AGE >35 yrs and persistence of post-coital bleeding for more than 4 WEEKS!!
So the important clincher here is duration and the presenting case still is not supposed to be diagnosed as cancer!! Hence infection is the most likely cause of atrophic vaginitis and from the given options Colposcopy is the likely correct option.
Choose a Question
×Choose a Question
×
Trial Access Limit Reached
You’ve reached the limit of free content. Subscribe to continue learning without restrictions.