

Hello,
Dr. Batman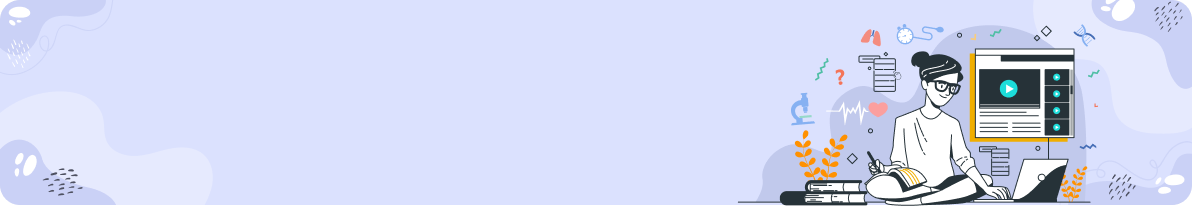
Hello Doctor, Welcome!
Profile

Name: Batman
Email: batman@gotham.com
ORTHOPEDICS
(Total Questions - 106)Q.1. A 26 year old primigravida pregnant woman at 34 weeks gestation presents with tingling and numbness with occasional pain of her right hand in addition to altered sensation over her right middle and index finger. Tinel test is negative. What is the most likely diagnosis?
Correct Answer : A
Because the stem states that the Tinel test is negative, you may be tricked into choosing a different answer. However, remember that the Tinel test has a very low sensitivity for carpal tunnel syndrome.
If the patient has a high suspicion of having carpal tunnel syndrome such as the classic tingling and numbness over the median distribution of the hand as well as being pregnant (which is a high risk factor for carpal tunnel syndrome) then you should always choose carpal tunnel syndrome as the answer.
Pregnancy is a known risk for carpal tunnel syndrome. In pregnancy, carpal tunnel is due to fluid retention. The best thing to do is to advise the pregnant women to wear wrist splints until delivery as after delivery, the carpal tunnel syndrome usually resolves.
Q.2. A 15 year old boy presents with fever and pain in the right lower thigh. The pain has been ongoing for the past one month. On examination, there is a 2 cm by 2 cm mass at the lower third of his thigh which is red, warm and tender. An X-ray shows bone destructionwith overlying onion-skin layers of periosteal bone formation and a soft tissue mass. What is the most likely diagnosis?
Correct Answer : C
Ewing’s sarcoma :
• A malignant round-cell tumour of long bones (typically grows in the diaphysis of long bones) and limb girdles, usually presents in adolescents (usually 5 to 15 years old)
Presentation :
• As a mass or swelling commonly in long bones of arms and legs, pelvis, or chest
• Pain in area of tumour
• Other signs and symptoms include: malaise, anorexia, weight loss, fever
Investigation :
• A typical "onion skinning" type pattern is often seen on X-rays.
This is due to bone destruction with overlying concentric layers of new bone formation.
Q.3. A 15 year old boy complains of pain in his leg which usually settles within an hour of taking aspirin. The pain is described as a dull pain which is persistent but is usually worse at night. What is the most likely diagnosis?
Correct Answer : B
The key fact here is the aspirin. The fact that the bone pain responds to aspirin in such a short period is classic for osteoid osteoma.
Osteoid osteoma :
• Benign bone tumor that develops in the long bones of the body such as the femur and tibia
• Pain is unrelated to activity and is relieved quickly by NSAIDS
• Pain is usually worse at night
• Frequently affects children and young adults
• Usually less than 1 cm in diameter
Important note to remember: Bone pain relieved well by NSAIDs is characteristic for osteoid osteoma.
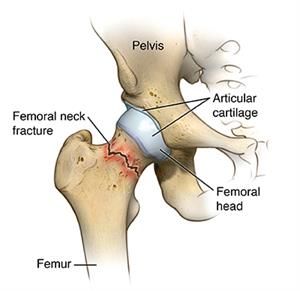
Q.4. A 33 year old woman fell from playing volleyball and hit her right knee. Valgus stress test is seen to be positive. What is the likely structure that is injured?
Correct Answer : C
The medial collateral ligament prevents the lateral movement of the tibia on the femur when valgus (away from the midline) stress is placed on the knee.
The valgus stress test is performed with the hip abducted and the knee at 30° of flexion, with one hand placed as a pivot on the knee. The other hand is placed on the foot with an abducting force. The idea is to attempt to force the leg at the knee into valgus.
The fingers of the hand at the knee are used to feel the amount of joint-line opening that occurs when valgus stress is applied.
If the joint line is seen to open up on the medial side, this is indicative of medial collateral ligament damage.
Test for knee ligament injuries -
Medial collateral ligament : Valgus stress test
Lateral collateral ligament : Varus stress test
Anterior cruciate ligament : Anterior drawer test, Lachman test
Posterior cruciate ligament : Posterior drawer test
Q.5. An 80 year old woman with mild dementia at a nursing home tripped and fell on her hand. She was brought to the Emergency Department with tenderness throughout her wrist. Distal pulses and sensation of her hand is intact. Her hand looks well perfused. X-ray revealed a fracture of the distal end of the radius with a 10 degree dorsal angulation. What is the best management for her?
Correct Answer : D
To choose the correct answer, we first need to know the diagnosis. This is a Colles' fracture.
Colles' fracture is a fracture of the distal radius with dorsal displacement of fragments. It typically occurs from a fall onto an outstretched hand that results in forced dorsiflexion of the wrist.
The characteristic dinner fork deformity makes it easy to recognize, along with the classical history.
We should always aim to tailor management for individual patients and their needs rather than apply generalized rules across the population.
This patient is elderly and she has mild dementia. In this situation, the best type of management for her should be a complete cast below the elbow to maximally immobilize her wrist and prevent further injury to her wrist, thus causing potential complications.
A back slab is the preferred method of management for younger patients. Surgical reduction is reserved for intra-articular fractures and if there is any intraarticular incongruity. Since there was no mention of this in the question, open reduction and internal fixation are the wrong choices.
Q.6. A 35 year old male typist suffered a wrist injury after falling on his right outstretched hand. He was treated with a scaphoid cast with the probable diagnosis of a scaphoid fracture. The cast was removed after 2 weeks from the injury for a repeat X-ray. After removing the cast, he noted that he had difficulty in moving his right thumb, index and middle finger. There was also a tingling sensation on those fingers. What is the most likely management that would improve his symptoms?
Correct Answer : C
Carpal tunnel syndrome is characterized by tingling, numbness, or pain in the distribution of the median nerve (the thumb, index, and middle fingers, and medial half of the ring finger on the palmar aspect) that is often worse at night and causes wakening.
It is due to compression of the median nerve as it passes under the flexor retinaculum. In this stem, the first hint is that he is a typist. Long hours of keyboard use may lead to or aggravate carpal tunnel syndrome.
Flexion or extension injury of the wrist can also be a secondary cause of carpal tunnel syndrome although it is rare that symptoms would arise in such a short time from the injury and immediately from removal of the cast.
Given the rest of the options, the release of the flexor retinaculum is the only option that would help improve symptoms should this be a diagnosis of carpal tunnel syndrome.
Q.7. A 64 year old diabetic woman presents to the GP with an acutely painful, swollen and hot right knee joint. There is limited range of movement and movements are painful in all directions. There is redness around the joint. An effusion surrounding the entire joint is obvious. There is no history of trauma. She has a pulse rate of 70 beats/minute, and a temperature of 37.8 C. What is the most likely diagnosis?
Correct Answer : A
She presents with the classic features of septic arthritis. Diabetes mellitus is a risk factor for septic arthritis. She should be referred to orthopaedics in the hospital for further management which would involve joint aspiration and empirical intravenous antibiotics.
In a patient presenting with acute monoarthritis, septic arthritis is the most common diagnosis to exclude as if not treated will result in permanent damage and even death in some patients.
The distractor here is reactive arthritis however unlike septic arthritis, fever is not a typical feature of reactive arthritis. Furthermore, reactive arthritis is more rare a disease compared to septic arthritis and it is typically seen in young adults.
The stem would need to include more information for one to pick reactive arthritis such as skin or eye manifestations or a recent genitourinary or gastrointestinal infection. Bursitis tends to result in tenderness and swelling localized to small areas with pain on passive movement only felt in certain directions.
Gout would be another differential however it is not in the options. Gout predominantly affects the first metatarsophalangeal joints but of course, the knee joint can be affected as well.
Q.8. A 60 year old female has pain and stiffness in her right hip joint. The pain has been worsening over the past 6 months. The pain increases in intensity as the day progresses and it is usually least pain in the morning. She has noticed nodules in the joints of the fingers of her hands. A recent blood test shows: Haemoglobin 92 g/L White cell count 9.8 x 109/L Platelets 250 x 109/L. What is the most likely diagnosis?
Correct Answer : A
The first step is recognizing that this is osteoarthritis. Pain in one joint that is worse towards the end of the day for 6 months are feature of osteoarthritis.
Hips are also a common joint affected by osteoarthritis. The nodules in her hand although not specified in the stem are likely to represent Bouchard’s nodes or Heberden's nodes which are seen in osteoarthritis.
Anaemia in this stem cannot be explained by choosing osteoarthritis except for the fact that it could be due to prolonged use of NSAIDS causing gastrointestinal bleeding.
This is one reason many doctors would have picked rheumatoid arthritis as the answer as rheumatoid arthritis is associated with anaemia of chronic disease.
However, we must remember how rheumatoid arthritis presents. Usually, more than one joint is involved in rheumatoid arthritis and the hands are almost always affected. With rheumatoid arthritis, the pain and stiffness are usually worst on waking but gradually improve during the day. This is quite the opposite of osteoarthritis which is represented in this stem.
Osteoarthritis :
- Monoarthritis
- Hip and knee are commonly affected
- Joint pain that is exacerbated by exercise and relieved by rest (sometimes gives a history of pain worsening at the end of the day)
- Bony deformity due to osteophytes.
In fingers, this presents as swelling at the distal interphalangeal joints (Heberden's nodes) or swelling at the proximal interphalangeal joints (Bouchard's nodes) Mnemonic for Heberden nodes and Bouchard's nodes.
Heberden - distal interphalangeal joint (H-D) (High Definition).
Bouchard - proximal interphalangeal joint (B-P) ( Blue Picture)
X-ray shows loss of joint space, marginal osteophytes, bone cyst, and subarticular sclerosis.
Mnemonic for X-ray features :
L - Loss of joint space.
O - Osteophytes.
S - Subchondral cysts.
S-Subchondral sclerosis
Management :
- Exercise and physiotherapy
- Weight reduction
- Regular paracetamol
- Topical NSAIDs
- Oral NSAIDs.
Note: Paracetamol and/or topical NSAIDs should be considered ahead of oral NSAIDs
- Joint surgery is the last option.
Q.9. A 33 year old woman with a previous history of pain at the left wrist following a fall on her outstretched hand 4 months ago presents with pain in the same wrist below the thumb. She has not sought any medical advice or treatment prior to this. She says that the pain is aggravated when she holds her baby. What is the most likely cause?
Correct Answer : C
The likely diagnosis here is a scaphoid fracture. A very typical scenario is a young person who falls on his or her outstretched hand with forced dorsiflexion. In this scenario, she fractured her scaphoid 4 months ago. As there was no management in place, likely a non-union would be in the differential. Non-union occurs in approximately 5-10% of nondisplaced scaphoid fractures.
The pain aggravated when she holds the baby gives us a small clue that she may be having pain during supination against resistance.
Signs: Tender in anatomical snuff box and over scaphoid tubercle, pain on axial compression of the thumb, and ulnar deviation of the pronated wrist, or supination against resistance. If initial X-rays are negative, cast and re-X-ray in 2 weeks.
Q.10. A 35 year old volleyball player has pain in his right arm and shoulder for the past 2 days. He finds it difficult to perform tasks which involve lifting his arm above his shoulder. His shoulder feels weak. The shoulder pain is worse at night when he is in bed. There is no history of trauma. What is the most likely cause of his pain?
Correct Answer : D
Supraspinatus tendinitis is often associated with shoulder impingement syndrome.
The stem would always have a history of either:
- A person with a job that requires repetitive overhead activity
- A person who has recently been involved in carrying heavy items e.g. moving to a new house.
- An athlete whose sport involves stressful repetitive overhead motions e.g. swimming, volleyball, tennis, badminton
Symptoms - Pain, weakness, and loss of motion. Pain worsens with overhead or above-the-shoulder activities.
Pain is often worse at night and can disturb sleep, particularly when lying on the affected shoulder.
Q.11. A 62 year old man has bone pain at his hips and back. On further investigatioin, alkaline phosphatase was found to be elevated in his blood. An X-ray shows multifocal sclerotic patches in the skull. What is the most likely diagnosis?
Correct Answer : D
Note that the patches of the skull are sclerotic and not lytic. Sclerotic patches represent Paget’s disease (osteitis deformans) whereas if it was lytic lesions on the skull it would represent multiple myeloma. Alkaline phosphatase is seen to be raised in both Paget’s disease and multiple myeloma however it is usually seen raised in multiple myeloma only when associated with fractures.
Q.12. A 33 year old man was painting his wall when he slipped from the ladder and fell from a height of 8 feet landing on his feet. On examination, his left foot is tender and swollen. Which bone is most likely to have been fractured?
Correct Answer : B
The Calcaneus is the bone that is most commonly fractured in a vertical fall. In cases of stress fractures, the metatarsals are commonly involved followed by the navicular and calcaneus.
A good mnemonic to remember is “CAL”. If the patient falls and lands vertically, look for CALcaneal fractures.
Important note: A common injury with calcaneal fractures is spinal fractures due to the type of force exerted. If a calcaneal fracture is seen on a foot X-ray, examine the patient for spinal fractures as well.
Q.13. A 24 year old man falls on an outstretched hand while playing football. He comes in complaining of pain at the base of the thumb. On physical examination, he is tender to palpate over the anatomical snuffbox. Wrist movement, particularly pronation followed by ulnar deviation is painful. X-rays are read as negative. What is the most appropriate next management?
Correct Answer : B
This is a typical presentation of a scaphoid fracture. It is a very debatable question. The answers C and B both may seem right, but the more appropriate answer of the two would be C.
First, we need to understand scaphoid fractures. A very typical scenario is a young man who falls on his outstretched hand with forced dorsiflexion. X-rays are usually negative but if repeated in 2 weeks become positive. They are also infamous because of a high rate of nonunion.
Signs: Tender in anatomical snuff box and over scaphoid tubercle, pain on axial compression of the thumb, and ulnar deviation of the pronated wrist, or supination against resistance. If initial X-rays are negative, cast and re-x-ray in 2 weeks. Unfortunately, for this question, re-x-ray was not an option.
Immobilization of the wrist and review in 2 weeks” would be a better answer because you should not cast for 6 weeks without knowing if there is a fracture. Thus immobilize for 2 weeks, and review (and obtain X-rays). If the fracture is seen after 2 weeks, then cast for another 4 more weeks.
Q.14. A 48 year old woman presented to her general practitioner with the complaint of new onset right shoulder pain and right thoracic spine pain. She says that the pain started a few weeks ago. Initially, it was just a minor discomfort but now it is a constant dull ache, which becomes worse when she lies down. She has had no relief with regular paracetamol or ibuprofen, which she purchased over the counter. She believes that the pain is probably due to her intense gym session last week and has presented today for further evaluation of her pain. Upon further questioning, she reveals that she was diagnosed with breast cancer one year ago. She finished her treatment successfully a few months ago and says that her oncologist reported to her that she was in remission. Upon examination of her shoulder, tenderness could be elicited over the shoulder joint and the surrounding areas. Her left shoulder appears to be normal and an upper limb neurological examination reveals no further abnormalities. An X-ray of her right shoulder was done which showed some degenerative changes. What is the most appropriate investigation that you will perform to add in the management of this patient?
Correct Answer : A
This question can be tricky if we see the age and the X-ray findings of the patient which shows degenerative changes at the age of 48.
In a 48-year-old, osteoarthritis may be present coincidentally. However, the pain seen in osteoarthritis is typically made worse by prolonged activity and relieved by rest, and not by lying down which is the first hint that there is possibly more to it than just osteoarthritis.
One should always be considering metastasis when there is a history of breast cancer.
Bone scintigraphy is a type of nuclear medicine imaging technique that would help look specifically at bone metastasis.
DEXA scan is not the right option. It is a bone density scan and is used to measure bone loss mainly in patients with suspected osteoporosis. Serum calcium levels are also performed in suspected bone metastasis because, in bone metastases, calcium can be released into the bloodstream leading to hypercalcemia.
However, there is a difference between "most appropriate investigation” and “most initial investigation”.
Serum calcium would be the most initial investigation but not the most appropriate unless, of course, this patient were to portray signs and symptoms of hypercalcemia.
A skeletal survey is useful for multiple myeloma where tumours are seen as “punched out” lesions. It is inappropriate for this case.
Q.15. A 33 year old woman has complaints of pain in her right arm and shoulder when she abducts it. The pain is worse at night and disturbs her sleep. She finds it difficult to perform task which involve lifting her arm such as combing her hair. She has recently moved to a new house and was involved in carrying heavy items. There is no history of trauma. What is the most likely cause of her pain?
Correct Answer : C
Please see Q-11
Q.16. A 44 year old man slipped while he was coming down the stairs and he fell on his outstretched arm. X-rays demonstrate an oblique fracture of the middle to distal thirds of the humerus. He is unable to dorsiflex his right wrist. What is the most likely associated nerve injury?
Correct Answer : D
The X-ray findings alone which show a humeral shaft fracture already give you the answer (radial nerve injury).
If you go on reading, this question gives you a second clue which is a wrist drop (he is unable to dorsiflex his wrist) which is classic for a radial nerve injury Fracture of the humeral shaft is often caused by a fall on an outstretched arm.
These fractures can injure the radial nerve, which courses in a spiral groove right around the posterior aspect of that bone.
The management of humeral shaft fracture is not commonly asked in exam but you may want to know it for your knowledge: Nonoperative management is adequate for >90% of these fractures.
A hanging arm cast or coaptation splint is used, and the nerve function returns eventually.
Surgical management may sometimes be needed but is uncommon.
These surgical options include intramedullary nailing and compression plating. It is important to remember the key phrases for nerve damage during exam. There are certain phrases you need to memorize to relate them to specific nerve damage.
Examples:
Wrist drop - Radial nerve.
Foot drop - Either common peroneal nerve or sciatic nerve.
Claw hand - Ulnar nerve, Paraesthesia of thumb, index, and middle finger.
Median nerve - Numbness on the superior aspect of the upper arm just below the shoulder joint.
Axillary nerve - Fibular neck fracture.
Common peroneal nerve - Femur neck fracture or Acetabular fractures.
Sciatic nerve - Fracture of the humeral shaft.
Radial nerve - Fracture of the humeral neck.
Axillary nerve - Monteggia fracture.
Q.17. A 20 year old fit man suddenly develops severe low back pain as he is getting up from bed. There is greater pain when he is lying supine with his leg raised. He gives a description of an electric shock pain moving down his left leg. What is the most likely diagnosis?
Correct Answer : C
Sudden onset of lower back pain and felt more during forward bending or similar movement like getting up from bed favour the diagnosis of lumbosacral disc herniation.
Q.18. A 61 year old female with a history of osteoporosis suddenly falls on her outstretched hand while shopping. She is tender over the wrist and there is visible deformity of the wrist. X-ray of the wrist shows a fracture at the distal radius with a dorsally displaced distal fragment. What is the most likely deformity?
Correct Answer : B
Colles’ fracture - Results from falls on an outstretched hand, often in old osteoporotic women. Dinner fork deformity.
Q.19. A 44 year old man complains of pain in the ring finger of his left hand, predominantly at the base of his finger. He finds that his finger is usually bent in the mornings when he wakes up and he has to straighten it with his other hand. It usually then straightens with a ‘click’. What is the most likely diagnosis?
Correct Answer : A
Trigger finger is also known as stenosing tenosynovitis. It usually affects the thumb, ring finger, or little finger. Usually, flexion is normal but beyond a certain range of motion, the patient would have difficulty extending the flexed finger. A snap is frequently felt as the finger straightens out.
Q.20. A 15 year old boy presents with a limp and pain in the left knee. The pain started acutely. He finds it very difficult to weight bear. Physical examination shows the leg is externally rotated and 2 cm shorter. There are limitations of flexion, abduction and medial rotation of the hips. As the hip is flexed, it externally rotates. What is the most likely diagnosis?
Correct Answer : B
Slipped Upper Femoral Epiphysis usually causes groin pain on the affected side, but sometimes causes knee or thigh pain. Usually in slipped upper femoral epiphysis, there is limited hip motion, and as the hip is flexed the thigh goes into external rotation and cannot be rotated internally.
SLIPPED UPPER FEMORAL EPIPHYSIS (SUFE) : A slipped upper femoral epiphysis is an orthopedic emergency.
The typical patient is a chubby boy, around age 13. They complain of groin (or knee) pain and are noted to be limping.
It is caused by the displacement of the femoral epiphysis (growth plate) about the femoral neck.
It is the most common cause of a limp in young boys.
In this age group, it must be actively excluded in a limping child.
The classic presentation is a limping, obese, 13-year-old boy with knee pain.
The pain can be poorly localized, so it may be seen as hip, groin, thigh, or knee pain.
Pain may present acutely or with a history of days or weeks.
Risk factors include: Obesity - Rapid growth - Male > 3:1.
Clinical features :
- The affected limb will be shorter and lie in external rotation
- Abduction is limited. When the hip is flexed, it will rotate externally Note: the left side is usually more commonly affected compared to the right side. The link below shows a short video on a patient’s experience with SUFE.
Mnemonic for slipped upper femoral epiphysis :
S – Shortening of the limb
U – Unable to abduct
F – Flexed hip will rotate externally
E – External rotation of the hip is seen.
Q.21. A 20 year old man was brought in by paramedics after jumping from an overpass in a suicide attempt. The paramedics reported obvious deformities of his bilateral lower extremities. He arrived at Accident & Emergency in pain but with normal vitals. Plain films demonstrate bilateral mid-shaft femur fractures and a left tibial shaft fracture. The patient was subsequently placed in bilateral distal femoral traction with a left long-leg splint and admitted to the orthopaedic department for an open reduction. The next day following surgery, he became acutely unwell with a decreased level of consciousness and his observations were recorded as follows: Heart rate 140 beats per minute Oxygen saturation of 80% on room air Temperature 38.2 C An arterial blood gas (ABG) was also done and the results are as follows: pH 7.47 (7.35-7.45) pCO2 3.8 kPa (4.7-6.0 kPa) pO2 7.3 kPa (10-14 kPa) Intubation caused an improvement of his hypoxaemia. An ECG done showed sinus tachycardia. What is the most likely cause of deterioration of his condition after surgery?
Correct Answer : A
The differential in the poly trauma patient with a sudden change in the level of consciousness is broad. In this particular patient, the history of long bone fractures, sudden hypoxaemic respiratory failure, and focal neurological findings suggest a specific aetiology: Fat embolism syndrome.
While it is true that pulmonary embolism in this patient is a distinct possibility since he has just had surgery, it is unlikely in this scenario.
By giving you a history of a femur fracture, the examiners are pointing you toward fat embolism as an answer.
If the examiners had wanted you to choose pulmonary embolism as an answer, they would not have included the history of the femur fracture.
Although atelectasis presents with low oxygen saturation, increased heart rate and breathlessness in the history point more towards a fat embolism.
Fat embolism syndrome is associated with long bone fractures of the lower extremities, usually the femur. Another group of patients with fat embolism syndrome is commonly seen in those with pelvic fractures.
They typically occur between 24 to 72 hours post-fracture. Fat embolism syndrome is a clinical diagnosis. Imaging is important to rule out other causes of the symptoms however the diagnosis of fat embolism syndrome can be made with the classic triad of hypoxaemia, neurologic deficits, and the petechial rash.
A petechial rash may not always be present like in this stem as only less than half of them have petechial rashes.
Treatment for fat embolism is largely supportive while it resolves spontaneously.
Q.22. A 26 year old man complains of severe pain while trying to grasp objects. It started when he fell during a skiing trip and hit his thumb on the ground while his thumb was abducted. On physical exam there is collateral laxity at the thumb-metacarpophalangeal joint with bruising over the joint. What is the most likely deformity?
Correct Answer : D
Gamekeeper's thumb :
• Also known as skier's thumb
• An injury to the ulnar collateral ligament (UCL) of the metacarpophalangeal (MCP) joint (on the medial side of the thumb) due to forced abduction of the MCP
• Historically suffered by gamekeepers when they killed rabbits by dislocating their necks with violent blows with the extended thumb.
However, in this era, it is seen as a skiing injury when the thumb is abducted and gets stuck in the snow or the ski strap during a fall.
Examination :
- Collateral laxity at the thumb-metacarpophalangeal joint
- Thumb is hyperextended and laterally deviated with swelling
- Grasp and pinching ability is reduced
Management :
- If incomplete ligamental injury and the joint is stable, immobilization in a thumb spica splint for 4-6 weeks.
Q.23. A 60 year old man is brought to the emergency department with a fractured hip. He has been having progressive hearing loss and was recently diagnosed with cardiac failure. Hypercalcaemia was noted on his blood test. What is the most likely diagnosis?
Correct Answer : B
History of deafness and heart failure favours the diagnosis of Paget’s disease.
Q.24. A 40 year old man presents to the Emergency Department with calf and heel pain. He was playing football when he suddenly felt a pop at the back of his left leg followed by pain at his calf. He says he felt as if someone kicked his leg from behind however no one was near him at that time. He describes himself as an infrequent football player. He has a history of a deep venous thrombosis on his left calf 5 years ago. On examination, Thompson test reveals absent plantar flexion. What is the most appropriate action?
Correct Answer : C
This is a classic case of Achilles tendon rupture. It usually occurs in a middle-aged man who decides to play a sport after several months or years of not being active. The Thompson test is when the examiner squeezes the calf muscle specifically at the gastrocnemius-soleus complex when the patient is lying prone with his feet over the examination table. If the Achilles tendon is ruptured, there will be absent plantar flexion.
Achilles tendon rupture requires a same-day review by either orthopaedics or a sports injury team thus the option for referring to a physiotherapist and GP as an outpatient is wrong.
The history of a DVT can throw you off and cause you to pick D-dimers as the answer. Requesting a D-dimer is a wrong answer as we do not suspect a DVT here.
There is an association between Achilles tendon rupture and thromboembolism and these patients are usually sent home with low molecular weight heparin for prophylaxis. The risk of thromboembolism occurs because he is immobile however in this case, he has not developed and we do not suspect a DVT.
Q.25. A 74 year old woman has a history of a Colles’ fracture three weeks ago after falling on a concrete floor with her right hand. She is otherwise fit and well. What is the most appropriate investigation to assess her risk for further fracture?
Correct Answer : A
Colles’ fracture results from a fall on an outstretched hand, often in old osteoporotic women as seen in this stem. The diagnosis of osteoporosis centres on the assessment of bone mineral density of which DEXA is regarded as the gold standard technique for the diagnosis.
A DEXA scan is the most commonly used investigation to assess fracture risk by measuring bone density and would be the best option here.
Q.26. A 55 year old woman has a history of a recent radial fracture. In the last decade, she had a Colles’ fracture in the right forearm and supracondylar humerus fracture of the left arm. She used to take corticosteroids for 2 years as part of managing her inflammatory bowel disease. What is the most appropriate investigation to perform?
Correct Answer : C
It is clear from the given history and the corticosteroid use that this is likely a case of osteoporosis. Other added risk factors in the stem include her sex (female) and her age (postmenopausal). Diagnosis of osteoporosis centers on the assessment of bone mineral density.
DEXA is required as the gold standard technique for the diagnosis of osteoporosis.
Q.27. A 50 year old man presents to the Emergency Department with acute back pain radiating down to his right leg. He is unable to weight bear. There is no history of trauma. The pain is relieved when lying down. What is the most appropriate investigation?
Correct Answer : A
Back pain radiating down to the legs which is relieved when lying down is characteristic of lumbosacral disc herniation. If there was an option to pick reassure and prescribe pain relief that would be the better option as an MRI here is not indicated.
There are no red flags in the stem. That being said, if an investigation was required, it would be an MRI.
MRI remains the most sensitive in showing disc herniations. Plain X-rays may be useful, as they can show misalignments, instabilities, and congenital anomalies well but the investigation of choice for a disc prolapse is an MRI.
Q.28. A 33 year old pregnant woman presents with right knee pain worse when moving the joint. The pain has been present for the last 4 months but it is worsening. The pain is noted to be worse at the end of the day. X-ray shows decreased joint space in the right knee. Blood results show a CRP of 12. What is the most appropriate management?
Correct Answer : B
The first step is recognizing that this is osteoarthritis. Pain in one joint that is worse towards the end of the day, decreased joint space, and inflammatory markers that are not significantly raised are recognizable features of osteoarthritis. Paracetamol is the first line for osteoarthritis.
It is also worth noting that she is pregnant and you should avoid prescribing NSAIDs as much as possible in a pregnant woman.
Q.29. A 63 year old man has knee pain and back pain for the last 3 months which is progressively worsening. Bowing of the tibia is noted on examination. He also has pronounced kyphosis. On further investigation, alkaline phosphatase was found to be elevated in his blood. Serum calcium levels were normal. What is the most likely diagnosis?
Correct Answer : D
Please see Q-12
Q.30. A 24 year old man presents to A&E after an injury to his hand while playing basketball. Examination of his hand reveals an avulsion of the extensor digitorum tendon from the distal phalanx. What is the most likely deformity?
Correct Answer : A
A mallet finger is an injury of the extensor digitorum tendon of the fingers at the distal interphalangeal joint. It results from hyperflexion of the extensor digitorum tendon.
It occurs when a ball (such as a softball, basketball, or volleyball), while being caught, hits an outstretched finger causing it to bend (flex) further than normal and rupture or stretch the extensor digitorum tendon.
Without the use of the extensor digitorum tendon, the finger stays bent (flexed) resembling a mallet. Splint DIP in extension for 6 to 8 weeks is usually adequate to manage this.
Q.31. A 58 year old woman fell with an outstretched hand. She presents with dinner fork deformity on the right wrist and tenderness over the right arm and wrist. Distal pulses of the limb is felt however she complains of numbness of the right hand. What is the most likely associated nerve injury?
Correct Answer : D
Please see Q-19
Q.32. A 7 year old boy fell in the playground with arm outstretched an hour ago. He is now seen to be holding his forearm complaining of pain. Examination of his forearm reveals tenderness but no sign of deformity or swelling. An X-ray was performed. What is the most likely diagnosis?
Correct Answer : D
In the exam, if a child falls and attains a fracture, it is almost always a greenstick injury. The classical fracture in a child is a greenstick injury.
This is when there is an incomplete fracture of the long bones. It occurs when the force applied to a bone results in the bending of the bone such that the structural integrity of the convex surface is overcome.
This usually occurs to a child who falls on an outstretched arm. Because the bones are soft in children, the bending force applied does not break the bone completely and the concave surface of the bent bone remains intact.
The fracture resembles the break that results when a supple green branch of a tree is bent and breaks incompletely.
Q.33. A 78 year old lady has been brought in after a fall in her home. She is now complaining of pain in her left hip and is unable to walk or weight bear. On examination, the left leg is noted to be shorter than the right and is externally rotated. What is the most likely diagnosis?
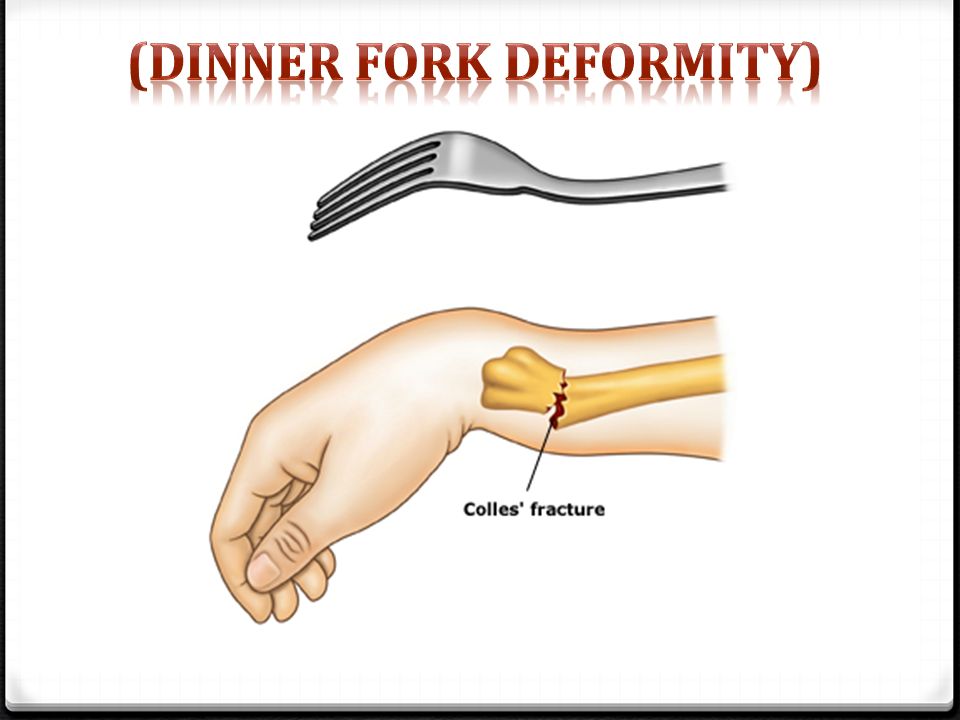
Correct Answer : B
This is a classical presentation of a fracture of the neck of the femur. It is usually seen in old patients secondary to osteoporosis and follows a fall or any other trivial injury involving the hip or bottom. The leg appears shortened and is externally rotated.
Typically, they would be unable to weight bear. This image shows the affected extremity which is the right leg. Shortened and externally rotated compared to the unaffected leg.
Q.34. A 15 year old male presents to his GP with the complaint of knee pain. He complains of being unable to sleep at night due to pain in his right knee. Further questioning reveals that he has been having intermittent unilateral pain in his right knee for the past seven months which has gradually worsened. He is concerned because he has had to give up football due to this pain. He has no other complaints and he has no significant past medical history. Examination of the knee reveals a 1 cm by 1 cm smooth, fixed, tender mass on the medial side of his right knee at the level of the tibial tuberosity. He is unable to bear weight on the knee however, his gait appears to be slightly antalgic. The rest of the knee examination revealed no other abnormalities but small lymph node was found in the ipsilateral inguinal canal. What is the most likely diagnosis in this patient?
Correct Answer : B
Malignant bone tumors are uncommon in children but the two that you need to know are osteosarcoma and Ewing’s sarcoma as these are the 2 most common malignant bone tumours affecting children. Osteosarcoma arises most often at the end of bones where growth occurs. It is the most common type of primary bone cancer and it accounts for just over half of childhood bone tumours.
Q.35. A 7 year old boy falls on his right hand with the arm extended. He has severe pain around the elbow. X-ray imaging showed a supracondylar fracture of the humerus. The distal fragment is displaced posteriorly. What is the most likely structure to be damaged?
Correct Answer : B
Supracondylar fracture of humerus is the most common fracture in childhood, with a peak incidence between the ages of 5 and 7 years.
It occurs occur with hyperextension of the elbow in a child who falls on the hand, with the arm extended. These fractures may compromise brachial artery, median, radial, or ulnar nerve function so check neurovascular status.
Keeping the elbow in extension after injury prevents exacerbating brachial artery damage from the time of injury.
Q.36. A 28 year old man was involved in a road traffic accident. He has severe pain in his shoulder and upper arm. There is loss of shoulder and arm function with bruising seen at the anterior shoulder on examination. X-ray shows a fracture of the neck of the humerus. What is the most associated neurovascular injury?
Correct Answer : C
Neurovascular injury in proximal humeral fractures :
- About a third of proximal humeral fractures produce neurovascular injury.
- Axillary nerve damage is most common.
- Suprascapular, radial, and musculocutaneous nerves can also be affected. Rarer neurovascular injury in proximal humeral fractures.
- Axillary artery injury is possible but rarely occurs
- Brachial artery injury also rarely occurs.
Q.37. A 33 year old man had fall on his outstretched arm. He is tender over the distal radius with no scaphoid tenderness. There is no obvious deformity on clinical examination. X-ray reveals a non-displaced distal radial fracture. Analgesia was given. What is the most appropriate next step in management?
Correct Answer : D
Since the fracture is nondisplaced wrist splints would be a better option as it allows patients to have mobility in their hands.
Q.38. A 33 year old woman who is 39 weeks pregnant is concerned about her child having developmental dysplasia of the hip as she suffered from developmental dysplasia of the hip when she was a child and had to undergo corrective surgery. Which one of the following is a risk factor for developmental dysplasia of the hip?
Correct Answer : B
The main risk factors for developmental dysplasia of the hip (DDH) are:
• Breech presentation
• Female sex
• Positive family history
• Birthweight more than 5 kg
• Congenital calcaneovalgus foot deformity
• Oligohydramnios
Q.39. A 67 year old woman presents to the emergency department with pain in her left groin. She falls from a chair in the waiting area and now is in severe pain and is not able to move her left leg. She takes alendronate regularly. What is the most likely diagnosis?
Correct Answer : C
The use of alendronate indicates that she is likely to be at high risk for an osteoporotic fracture as alendronate is primarily used to prevent fractures in osteoporotic patients.
Proximal femur fractures are one of the common areas of fractures seen in osteoporosis.
Thus, a fracture of the neck of the femur would be the most appropriate answer.
Osteoporosis is the reduction in the amount of bony tissue within the skeleton.
Osteoporotic bone is at high risk of fracture, even after trivial injury.
It usually is clinically silent until an acute fracture like in this stem. Common osteoporotic fractures are seen in hips, wrist (Colles’) and compression fractures of vertebral bodies.
Q.40. A 65 year old man with a three-year history of prostate cancer presents to the GP surgery with worsening thoracic backache over the past few weeks. He started having episodes of urinary incontinence today. He takes regular slow-release morphine for his pain however he still feels back pain at night which prevents a good night sleep. On examination, he has bilateral lower limb weakness. What is the most appropriate investigation to request?
Correct Answer : A
This is an oncological emergency. Patients with spinal metastases often experience pain for several weeks before signs of malignant spinal cord compression (MSCC).
In the exam, suspect malignant spinal cord compression with anyone with back pain, neurological symptoms, and a history of cancers of the breast, prostate, or myeloma.
Q.41. A 30 year old male presented to the Emergency Department with the complaint of swelling in his left hand. He states that he works in a textile factory and while operating one of the machines, his left hand got stuck in the machine. The incident occurred five hours ago. He has already taken some over the counter medication for pain relief, which proved to be not very helpful. When the patient noticed that the4 pain was not relieved and that his fingers began swelling, he then presented to hospital. The swelling appears to be distributed evenly all over the fingers of his left hand and he has noticed that it has been increasing since his accident. An X-ray was arranged but yielded no evidence of a fracture. On examination, the patient appears to be in obvious pain and clutches his left arm to his abdomen. Swelling is present over his fingers and there is a limited range of movement, namely of flexion and extension. What is the most appropriate step in the management of this patient?
Correct Answer : A
This is a typical case of a sprain injury. A sprain is an injury to a ligament which usually occurs by the ligament being overstretched. To choose the best treatment option for this patient, it is important to know the main aim of treating a sprain injury.
The usual initial treatment for a sprain is described as paying the PRICE. P: Protect R: Rest I: Ice C: Compression E: Elevation A high-arm sling is the right option for this patient.
Q.42. A 78 year old woman fell with an out stretched hand after slipping on ice on the pavement. She presents to the Emergency Department with a deformity of the right wrist. On examination, her wrist is tender to touch. There is no scaphoid tenderness. Her distal sensation and pulses are intact. An X-ray of her right wrist shows a posterior and radial displacement of the distal fragment of the radius. What is the most appropriate management?
Correct Answer : C
This is a typical Colles’ fracture presentation. Closed reduction followed by a Plaster of Paris cast below the elbow and a fracture clinic appointment is the most appropriate answer here.
Q.43. A 79 year old man had a fall 2 days ago and since then he is unable to bear weight on his right leg. He presents with deformity and tenderness over the right hip area. X-ray shows fracture of the acetabulum. What is the most likely associated nerve injury?
Correct Answer : A
Acetabular fractures and posterior dislocation of the hip Both acetabular fractures and posterior dislocation of the hip can result in sciatic nerve damage.
Sciatic nerve injury:
Pain in the distribution of the sciatic nerve, loss of sensation in the posterior leg and foot, and loss of dorsiflexion (peroneal branch) For these fractures always check for sciatic nerve damage. Examine foot dorsiflexion and below-knee sensation.
Q.44. A 7 year old boy fell on his outstretched arm and presents with pain around the elbow. On examination, radial pulse is absent on the affected hand. What is the most likely diagnosis?
Correct Answer : C
Supracondylar fracture of the humerus is the most common fracture in childhood.
It occurs occur with hyperextension of the elbow in a child who falls on the hand, with the arm extended.
These fractures may compromise brachial artery, median, radial, or ulnar nerve function so check neurovascular status.
Keeping the elbow in extension after injury prevents exacerbating brachial artery damage from the time of injury. In this question, damage or occlusion of the brachial artery is the cause of absent radial pulse.
Q.45. A 34 year old male presents with the complaint of back pain. It occurred two days ago when he and his family were moving home. He says that the pain radiates to his left foot and becomes much worse when he coughs. Examination reveals a loss of deep tendon reflexes on his left leg and a postive straight leg raising test. He has sensory loss over the anterior aspect of the knee. What is the most likely cause of this patient’s symptoms?
Correct Answer : B
This patient has a prolapsed intervertebral disc - a lumbosacral disc herniation. L5 nerve root compression occurs in a prolapsed lumbar intervertebral disc however if this was the case there would be sensory loss of the dorsum of the foot and intact reflexes.
Spinal fractures and cauda equina syndrome often present with bowel/bladder disturbance. In the exam, when the question writers want you to choose cauda equina syndrome, they will give a history of bowel incontinence, urinary retention, or saddle paresthesia.
The ilioinguinal ligament runs from the pubic tubercle to the anterior superior iliac spine. It has nothing to do with this patient’s back pain.
Q.46. A 59 year old woman is being investigated for chronic back pain. X-ray of her spine was reported to be normal. Bone scans revealed multiple lesions in the skeleton suggestive of metastatic disease. What is the most likely site of the primary?
Correct Answer : D
Bone scan is highly sensitive to osteoblastic or sclerotic metastases. In females, the most common tumour causing bone metastasis is the breast. Second to that is the lungs.
In males, the most common tumour causing bone metastases is the prostate. Second to that is the lungs.
The most common site for bone metastases to occur is in the spine. Then the pelvis, ribs, skull, and long bones.
Q.47. An 81 year old man presented to his GP with the complaint of pain in his right hip that radiates to his right knee. He says that he noticed the pain a few months ago but that it has recently become a lot worse and has now begun to disturb his sleep at night. He mentions as well that the pain is worse when he walks but that it becomes releived somewhat upon rest. He denies the possibility of having sustained trauma to his hip and denies having any joint stiffness in the morning. Physical examination reveals a limp on his right side. Hip examination reveals pain upon passive movement of the joint as well as a reduced range of motion upon active movement. A mild degree of crepitus can also be appreciated. What is the most likely diagnosis?
Correct Answer : B
This patient has osteoarthritis (OA) of the hip. In the exam, look for an elderly person who has joint pain that is exacerbated by exercise and relieved with rest.
The exam scenarios to look for are osteoarthritis of the knee, the hip and the wrist, and the hand. Questions dealing with the wrist and hand will often attempt to trick you with rheumatoid arthritis (RA) so learn the differences between OA and RA well.
Q.48. A 13 year old boy presents with pain in the groin. He is seen limping. There was no history of trauma. The pain started a few weeks ago but has been worsening. There are limited hip motions, and as the hip is flexed the thigh goes into external rotation and cannot be rotated internally. When the boy is lying down, the left leg is 2 cm shorter than the right leg and it is externally rotated. What is the most likely diagnosis?
Correct Answer : A
Slipped Upper Femoral Epiphysis usually causes groin pain on the affected side, but sometimes causes knee or thigh pain.
Usually in slipped upper femoral epiphysis, there is limited hip motion, and as the hip is flexed the thigh goes into external rotation and cannot be rotated internally. The pain may be acute but may also be chronic like in this case and symptoms may be present for weeks.
Q.49. A 16 year old boy was rushed to A&E following a road traffic accident. He was found to have swelling and deformity in his right thigh. A femur fracture is suspected. Primary survey has been done and his airway was found to be patent however, examination of his right leg reveals no proximal or distal pulses. There is no visible wound or loss of blood but the patient is severely hypotensive. What is the most likely structure to be involved in this patient’s fracture?
Correct Answer : C
The only answer that makes sense in the choices is the femoral artery.
The femoral artery is a large artery in the thigh and the main arterial supply to the leg. It enters the thigh from behind the inguinal ligament as the common femoral artery.
In a high-impact accident that has resulted in a femur fracture, we would be most concerned about injury to the femoral artery. As this patient is severely hypotensive, it indicates an injury to the femoral artery, most likely from a piece of bone. Injuries to the femoral artery may require reattachment surgery.
Q.50. A 22 year old football goalkeeper was brought to the Emergency Department with a locked right leg and the inability to extend the knee greater than 30 degrees. The injury occurred when he tried to catch the ball and, instead, landed with his leg twisted. What is the most likely diagnosis?
Correct Answer : C
This is a classic picture of a common sports injury. The player jumps up and lands on a slightly twisted knee hence giving rise to a medial meniscus tear.
He could very well also have an anterior cruciate ligament injury as meniscal tears are often associated with ACL injury. If this question had medial collateral ligament tear as a choice, then you would pick that.
If you remember the mechanism of injury for knee trauma, then you will never get a knee question wrong in the exam.
Q.51. A 33 year old man who suffers from chronic lower back pain has shooting pain coming down his left leg. He has reduced sensation of the dorsum of his left foot. On examination, he experiences pain while performing a straight leg raise test of his left leg at 45 degrees. There is weakness in left ankle dorsiflexion. Which nerve root is likely to be compressed?
Correct Answer : C
L5 nerve root compression can lead to ankle dorsiflexion weakness and reduced sensation on the dorsum of the foot.
Q.52. A 12 year old boy attends A&E with pain after falling off his bicycle. A lateral X-ray of his wrist shows a fracture at the distal radius with the distal fracture fragment displaced anteriorly. What is the most likely diagnosis?
Correct Answer : D
Smith's fracture :
• Also known as reverse Colles' fracture
• It is a fracture of the distal radius that has anterior displacement of the distal fragments (opposite to Colles’ fracture where there is dorsal displacement of fragments)
• It is usually caused by falling backward like a fall onto the palm of the outstretched hand with the arm above it pronating as the body falls. It can also occur if one falls onto a flexed wrist.
• The characteristic appearance is called a 'garden spade deformity'
• Lateral view of an X-ray of a Smith's fracture is very similar to a Colles' fracture except with the displacement anteriorly instead of posteriorly thus the term reverse Colles’ fracture.
Q.53. A 30 year old lady was playing volleyball when her hand got injured with the volleyball. The right hand is not swollen and there is tenderness under the root of the thumb. Wrist movement, particularly pronation followed by ulnar deviation is painful. X-ray of the wrist shows no presence of fractures. What is the most appropriate next step in management?
Correct Answer : A
The likely diagnosis is scaphoid fracture where the initial X-ray may not show the fracture right away. A very typical scenario is a young person who falls on his or her outstretched hand with forced dorsiflexion. In this scenario, she fractures her scaphoid from a volley.
X-rays are usually negative but if repeated in 2 weeks become positive.
They are also infamous because of a high rate of nonunion.
Signs: Tender in anatomical snuff box and over scaphoid tubercle, pain on axial compression of the thumb, and ulnar deviation of the pronated wrist, or supination against resistance. If initial X-rays are negative, cast and re-X-ray in 2 weeks.
Q.54. A 12 year old boy was playing in the park with his younger brother when he accidentally fell onto his out stretched hand. He was subsequently brought to A&E with the complaint of pain around his elbow. Upon examination, generalised swelling was found around the elbow region and he flinches away in pain when the doctor tries to touch his elbow. He was found to have a limited range of motion at his elbow, and passive rotation of his arm yields significant pain. Examination of the radial nerve reveals tenderness over the radial tunnel and the patient complains of pain when his fingers are extended against resistance. What is the most likely type of fracture in this patient?
Correct Answer : B
The stem gives you all the clues to point you in the direction of a radial fracture however, the examiners want you to know that radial head fractures occur more commonly in adults and radial neck fractures occur more commonly in children.
Radial head movement in children is rare. Radial neck fractures and radial head fractures present with the same signs and these are:
• Swelling over lateral elbow
• Limited range of motion of the elbow
• Pain is greatly increased with passive rotation of the elbow.
There may be vascular/nerve involvement so it is necessary to assess the radial nerve for damage.
Q.55. A 38 year old painter has developed burning pain around his right lateral elbow that radiates to his forearm. The pain started two months ago and has gradually worsened over time. The pain is worse when he lifts heavy objects and he finds that his grip strength when using his right hand is reduced. Upon examination, there is tenderness over the lateral epicondyle of his right arm and pain is elicited upon resisted extension of his right wrist. Which is the most likely muscle group affected here?
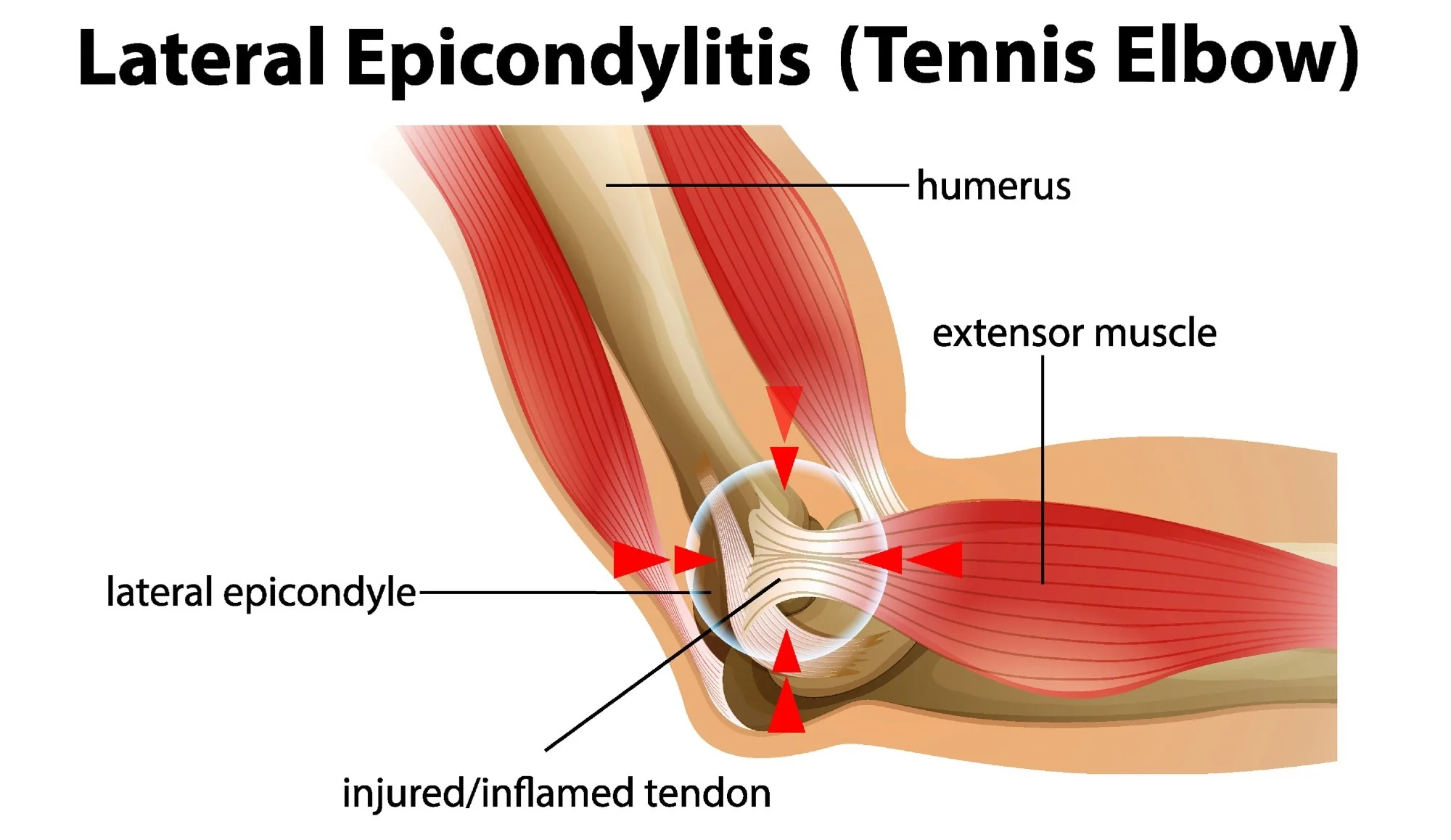
Correct Answer : D
This patient is suffering from a condition called tennis elbow or lateral epicondylitis. In this condition, there is pain where the common extensor tendon arises from the lateral epicondyle of the humerus. The muscle group that is affected is the wrist extensors. Why is the answer not forearm extensors?
The primary condition affects the extensors of the forearm and the specific muscle that is affected is the extensor carpi radialis brevis muscle.
Q.56. A 53-year-old female presents with an acute painful hot knee joint. She is a known case of RA (rheumatoid arthritis). On examination, the knee is red, tender and swollen. The hamstring muscles are in spasm. Her temperature is 38.5C and BP is 120/80 mmHg. What is the best next investigation?
Correct Answer : A
Joint aspiration for cytology and culture and sensitivity.
Case of septic arthritis. Any chronically arthritic joint is predisposed to infection. Moreover chronic use of steroids in Rh. arthritis is one of the important predisposing factors. In this age group likely organism is Staphylococcus. In the younger age group Neisseria gonorrhea is more common.
Q.57. A patient with an acute gout attack came to the emergency department. What drug should be given to relieve symptoms?
Correct Answer : A
Oral NSAIDs commenced immediately and continue for 1 – 2 weeks; Colchicine can be an effective alternative but is slower to work than NSAIDs. Intra-articular corticosteroids are highly effective in acute gouty monoarthritis.
Q.58. A young boy fell on his outstretched hand and has presented with pain around the elbow. He has absent radial pulse on the affected hand. What is the most likely diagnosis?
Correct Answer : B
Damage or occlusion of the brachial artery is the cause of absent radial pulse. Often closed reduction results in the restoration of normal anatomy and correction of occlusion of the bracheal artery and establishes circulation again but in few instances, open reduction is required to fix the occluded artery.
Q.59. A 23-year-old woman has been having pain at the base of her thumb, the pain is reproduced when lifting her 3 month old baby or changing diapers and also with forceful abduction of the thumb against resistance. What is the likely cause?
Correct Answer : C
Can be diagnosed by Finkelstein’s test: The physician grasps the thumb and the hand is ulnar deviated sharply. If sharp pain occurs along the distal radius (top of the forearm, about an inch below the wrist), de Quervain's syndrome is likely.
Q.60. A 78-year-old male with diabetes mellitus and hypertension, had a fall and since then is unable to walk. He presents withdeformity and tenderness over the right hip area. X-Ray shows fracture of femur neck. What is the most associated nerve injury?
Correct Answer : A
Sciatic nerve injury though may occur but may not be very common!.
Q.61. A 37-year-old female had a fall with outstretched hand, presented with dinner fork deformity and tenderness over the right arm. What is the most associated nerve injury?
Correct Answer : D
Median nerve is the nerve-injured in Colle’s fracture.
Q.62. A pregnant woman with longterm history of osteoarthritis came to the antenatal clinic with complaints of restricted joint movement and severe pain in her affected joints. What is the choice of drug?
Correct Answer : A
Paracetamol
Q.63. A 6-year-old fell on outstretched hand while playing. He feels tender at the elbow but otherwise well. What is the most likely diagnosis?
Correct Answer : B
Greenstick fracture
Q.64. A 15-year-old boy presents with a limp and pain in the knee. Examination: leg is externally rotated and 2 cm shorter. There is limitation of flexion, abduction and medial rotation. As the hip is flexed external rotation is increased. Choose the most likely diagnosis?
Correct Answer : D
The given presentation is classic for slipped femoral epiphysis.
Q.65. A 60-year-old woman presents with acute onset of bone and back pain following a rough journey in a car. Examination: tenderness at mid-thoracic vertebra with spasm, she feels better once she bends forward. What is the most probable diagnosis?
Correct Answer : B
Myofascial pain syndrome is a chronic pain disorder. In myofascial pain syndrome, pressure on sensitive points in your muscles (trigger points) causes pain in seemingly unrelated parts of your body. This is called referred pain.
Myofascial pain syndrome typically occurs after a muscle has been contracted repetitively.
Q.66. A 12-year-old boy with a history of fall on an outstretched hand was brought to the emergency department with swelling and pain around the elbow. His radial nerve was affected. What is the type of fracture?
Correct Answer : A
Around 50% of interosseous nerve lesions occur in supracondylar fracture whereas 25% show radial nerve damage.
If the fracture is a spiral fracture of the lower third of the humerus it causes nerve damage in 18% almost all of which are radial nerve lesions.
However, as the fracture is around the elbow (not above) it is a supracondylar fracture.
Q.67. A 16-year-old boy following a RTA was brought to the emergency department with a swelling and deformity in his right thigh. Examination: airway is patent and is found to have a pulseless leg. Which structure is involved in this fracture?
Correct Answer : A
Femoral artery
Q.68. A 60-year-old man has had spontaneous painful swelling of his right knee for 3 days. 5 days prviously he had an inguinal hernia repaired as a day case. He takes bendroflumethiazide 2.5mg daily. He is apyrexial. What is the most appropriate diagnostic investigation?
Correct Answer : D
Thiazide diuretics cause hyperuricemia which can precipitate an acute attack of gout.
Q.69. A 30-year-old lady was playing volleyball when her hand got injured with the ball. The right hand is not swollen and there is tenderness under the root of the thumb. X-ray is normal. What is the most appropriate next management?
Correct Answer : C
A likely diagnosis is a scaphoid fracture where an X-ray may not show the fracture right away.
In such case put her hand in a below elbow cast and repeat the X-ray in a week or two to see if the fracture becomes visible. Usually, it becomes visible as a healing fracture line.
Q.70. A 10-year-old child who presented with fracture of the radius which was treated with a plaster cast, complains of pain. Examination: limb is swollen but warm and well perfused, pulses are present. What should you do next?
Correct Answer : D
This is not compartment syndrome. So the next step is analgesia.
Q.71. A 22-year-old man came to the hosp after an injury in his hand while playing basketball. Examination: avulsion of extensor tendon from the distal phalanx. What is the most probable deformity?
Correct Answer : C
A finger that bends down at the end joint and cannot be straightened is called a mallet finger.
It is caused by an injury to the extensor tendon that straightens (extends) the finger. A splint worn day and night for 6-8 weeks will cure the problem in most cases.
Q.72. A 35-year-old male typist who suffered a scaphoid fracture was treated with a scaphoid cast. After 2 weeks when the cast was removed for a review X-ray, it was found that he had problems in moving the thumb, index and middle fingers. What would you suggest as the management for the recent problem?
Correct Answer : A
Now he developed carpal tunnel syndrome (median nerve compression).
Q.73. A 35-year-old male who recently had an appendicectomy has got severe pain in his right big toe. Joint is red and swollen. He consumes 30 units of alcohol/week. What is the most probable diagnosis?
Correct Answer : C
Alcoholic drinks can raise the level of uric acid in the blood.
Q.74. A 25-year-old male who recently noticed change in his shoe size, he is also constipated, has a preference to hot weather, his skin is dry, has severe pain in wrist joint. Joint is red and swollen. What is the most probable diagnosis?
Correct Answer : D
Hypothyroidism (change of shoe size due to myxedema (or pedal oedema can be seen in hypothyroidism), other features of constipation, cold intolerance, and dry skin are well-known features of hypothyroidism) has well-recognized association with pseudogout.
Q.75. A 20-year-old fit man suddenly developed severe lower back pain as getting up from bed. What is the most probable diagnosis?
Correct Answer : C
Sudden onset of lower back pain and felt more during forward bending or similar movement like getting up from bed favours the diagnosis of PID.
Q.76. A 60-year-old man brought to the emergency department with fracture hip, he is deaf and has bilateral pedal edema. What is the most probable diagnosis?
Correct Answer : A
H/O deafness and evidence of heart failure like pedal edema favours the diagnosis of Paget’s disease.
Q.77. An 80-year-old lady presents with pain on left 6th rib for a week. It is non-tender on examination. What is your most likely diagnosis?
Correct Answer : C
Bone degeneration
Q.78. A 63-year-old female with a history of osteoporosis suddenly falls on her outstretched hand while shopping. X-ray shows fracture at distal radius with backward shift of the distal fragment. What is the most probable deformity?
Correct Answer : A
Dinner fork deformity
Q.79. A woman with a previous history of pain at the left wrist following a fall 4 months ago for which she didn’t seek any treatment now presented with pain in the same wrist below the thumb and the pain is aggravated whenever she holds her baby. What is the cause?
Correct Answer : B
Scaphoid fracture
Q.80. A 67-year-old man presents to the emergency department with pain in his left groin. He suddenly collapses and he is not able to move or lift his leg. He is on alendronate. What is the diagnosis?
Correct Answer : A
Use of alendronate indicates osteoporosis where fracture neck of femur is more common.
Q.81. A woman came with the complaint of pain in her right arm when she abducts it. She has recently moved to a new house. There is no history of trauma. What is the likely cause of her pain?
Correct Answer : D
Tendinitis and partial tears in the supraspinatus tendon causes a ‘painful arc’ since as the person elevates his arm sideways, the tendon begins to impinge under the acromion through the middle part of the arc, and this is usually relieved as the arm reaches 180 degrees (vertical).
Q.82. A 19-year-old boy comes to the emergency department with pain, swelling and tenderness 2cm distal to Lister’s tubercle of radius. Examination: proximal pressure on the extended thumb and index finger is painful. X-ray: no fracture. What is the next appropriate management for the patient?
Correct Answer : C
Request a dedicated ‘scaphoid’ series. If –ve, and fracture is suspected MRI has been shown to be sensitive and cost-effective. CT is an alternative. If neither is available, cast and re-x-ray in 2 weeks.
Q.83. A young man’s arm was caught in a machine. X-ray showed no fracture but arm is very swollen. What is the best treatment?
Correct Answer : B
If the limb is kept hanging it will aggravate the swelling as fluid shifts to dependant part. Here wide splint with upward position will help the accumulated blood or fluid to move down and will improve the swelling.
Q.84. A 6-year-old boy fell in the playground and has been holding his forearm complaining of pain. Examination: no sign of deformity or swelling. However, there is minimal tenderness on examination. What is the diagnosis?
Correct Answer : D
Green stick fracture of distal radius
Q.85. A young woman fell and hit her knee. Examination: valgus test +ve. What ligament was most probably injured?
Correct Answer : B
The valgus stress test involves placing the leg into extension, with one hand placed as a pivot on the knee.
With the other hand placed upon the foot applying an abducting force, an attempt is then made to force the leg at the knee into valgus.
If the knee is seen to open up on the medial side, this is indicative of medial collateral ligament damage.
Q.86. A pregnant woman presents with knee pain on movements. The pain becomes worse at the end of the day. Radiology shows decreased joint space. Laboratory investigation: CRP=12. What is the 1st line medicine?
Correct Answer : A
Pain on movement, pain worse at the end of the day, and decreased joint space are characteristic of osteoarthritis supported by NO significant rise in inflammatory marker (CRP=12). 1st line of medicine is paracetamol.
Q.87. A 60-year-old woman presented with radial fracture and had a colle’s fracture and supracondylar fracture in the past. What investigation is required to detect her possibility of having the same problem later?
Correct Answer : A
The likely cause of this multiple fracture is osteoporosis (post-menopausal women) for which we should do a Dexa scan to establish the diagnosis.
Q.88. A 48-year-old man presents with bone pain. Laboratory: ALP high, phosphate normal. What is the most likely diagnosis?
Correct Answer : C
Bone pain, high ALP, and normal phosphate are suggestive of Paget's disease.
In osteoporosis Ca+, PO4³-, and ALP are normal. In osteomalacia Ca+ is low, PO4³- low and ALP is high. In Paget's disease Ca+ and PO4³- normal and ALP markedly raised.
Q.89. A 60-year-old female has pain and stiffness in her right hip joint. Pain is not severe in the morning but increases as the day progresses. She has noticed some nodules in her hands. Investigations: Hb low. What is the most probable diagnosis?
Correct Answer : B
Stiffness and pain of right hip increasing as the day progresses, nodules in hands (Hebarden or Bouchard’s nodes), anemia (probably secondary to prolonged NSAIDs use) indicates osteoarthritis.
Q.90. A 30-years-old female has chronic diarrhea, mouth ulcers and skin tags. She complains of visual problems, low back pain and morning stiffness. Investigations: ESR & CRP raised, Hgb 10mg/dl. What is the most probable diagnosis?
Correct Answer : D
There is a well-known association between IBD and seronegative arthritis (particularly AS). Here low back pain, visual problems, morning stiffness, raised ESR and CRP, and low hemoglobin indicate the diagnosis of Seronegative arthritis.
Q.91. An elderly man with recently diagnosed HF (heart failure) has been treated with diuretics. He now develops severe joint pain in his left ankle with swelling and redness. What is most likely investigation?
Correct Answer : C
Thiazide diuretics may increase uric acid levels in blood causing or precipitating gout and joint fluid may show uric acid crystals.
Q.92. A 60-year-old lady with a history of HTN and suffering from RA since the last 10 years now presents with hot, swollen and tender knee joint. What investigation would you do for her?
Correct Answer : B
RA itself is a risk factor for joint infection and there are possibilities to increase the chance of septic arthritis with the use of probable steroid which lowers immunity and further facilitates infection of joints for which C&S of joint aspirate should be done.
Q.93. An 80-year-old woman fell over at her nursing home. X-ray shows fracture of radius with <10 degree of dorsal angulation. What is the most appropriate treatment?
Correct Answer : C
Closed reduction of fracture
Q.94. A 32-year-old woman presents with complaints of having low back pain. She is taking analgesics for it. All investigations are normal. What will you advice her?
Correct Answer : C
Advice to be more active
Q.95. A 34-year-old labourer developed severe pain in his lower back after lifting a sack of sand. He also complains of shooting pain down his leg. The GP has prescribed him complete bed rest, with painkillers and also scheduled an MRI for him. What is the most likely diagnosis?
Correct Answer : B
Intervertebral disc prolapsed can cause severe back pain following heavy lifting and radiculopathy (pressure on spinal nerve root) can cause this shooting pain which can be demonstrated by MRI spine.
Q.96. A 34-year-old man sustains a fracture to shaft of femur after falling from the roof of his house. Examination: distal pulses are not palpable. Which vessel is damaged?
Correct Answer : A
Femoral artery
Q.97. A 66-year-old man has renal colic. He has also presented with acute onset pain in his knee in the past. What is the most likely cause for renal failure?
Correct Answer : D
Knee pain is due to gout and renal colic may occur from uric acid stone (urate stone).
Q.98. An 11-year-old boy came to the hospital with pain after falling off his bicycle. X-ray shows fracture at distal radius with forward angulations. What is the most probable diagnosis?
Correct Answer : D
Garden spade deformity is seen in Smith fracture. A Smith fracture is a break to the end of the radius. The end part of the bone, which forms part of the wrist joint, is displaced or angled in the direction of the palm of the hand.
Often, this injury occurs by a fall to the back of a flexed wrist but can occur in any fall to an outstretched hand.
Q.99. A 28-year-old male complains of severe pain while trying to grasp any object. It started since he participated in skiing and had a fall and caught his thumb in the matting. Examination: rupture of the ulnar collateral ligament of MCP joint of the thumb. What is the most probable deformity?
Correct Answer : B
Gamekeeper's thumb is an insufficiency of the ulnar collateral ligament (UCL) of the metacarpophalangeal (MCP) joint of the thumb.
Q.100. A 25-year-old male had an injury to the knee while playing football. X-ray shows condylar fracture of tibia. What is the most probable deformity?
Correct Answer : D
Genu valgus
Q.101. A 2-year-old fell on outstretched hand on playground. He presents with pain on base of the thumb. X-ray shows no fracture. What is the most likely diagnosis?
Correct Answer : D
Scaphoid fracture is often missed in initial x-ray.
Q.102. A 65-year-old woman with DM, hypertension and normal kidney function underwent a total right hip replacement. She had massive haemorrhage during the operation and was given 8 units of packed RBC. The blood pressure dropped to 60/40 mm Hg for about two hours before it was corrected with blood transfusion. Two days after the surgery the serum creatinine level rose to 4.2 mg/dl (normal <1.5 mg/dl), BUN was 50 mg/dl (normal 10-20 mg/dl) and potassium 5.0 mmol/L (normal 3.5-5.0 mmol/l). There were brown granular casts in the urine sediment. Which is the most likely cause of this complication?
Correct Answer : C
Hypotension even for some minutes or few hours can readily lead to acute tubular necrosis which is evident here by uremia and further supported by brown granular cast in the urine sediment.
Q.103. A 3-year-old boy is playing with his brother when he falls. He cries immediately and refuses to walk. His mother carries him to hospital. He had a full term NVD (normal vaginal delivery) with no neonatal complications. His immunisations are up to date. Examination: looks well and well-nourished, no dysmorphic features. He has slight swelling, warmth and discomfort on the lower 1/3 of the left tibia, and refuses to weight bear. AP and lateral x rays of the tibia are normal. What is the most likely diagnosis?
Correct Answer : D
Toddler's fracture :
• Undisplaced spiral fractures of the tibial shaft in children under 7 years old often follow minimal trauma and may not be visible on initial X-ray.
• Can be difficult to diagnose but should be suspected whenever a child presents with a limp or fails to bear weight on the leg.
• Treatment consists of immobilization for a few weeks to protect the limb and relieve pain.
• Subperiosteal bone formation is usually apparent on X-rays by two weeks.
Q.104. A 24-year-old woman fell and injured her right knee. The knee is swollen and tender to valgus stressing. Which of the following ligament is the most likely to have been damaged?
Correct Answer : C
Positive valgus stress test indicate medial collateral rupture.
Q.105. A 70-year-old man who is on bendroflumethiazide develops an acute swelling of his right knee. What is the most appropriate diagnostic investigation?
Correct Answer : A
Bendroflumethiazide can cause hyperurecemia leading to gout.
Q.106. A 30 year old male presented to the Emergency Department with the complaint of swelling in his left hand. He states that he works in a textile factory and while operating one of the machines, his left hand got stuck in the machine. The incident occurred five hours ago. He has already taken some over the counter medication for pain relief, which proved to be not very helpful. When the patient noticed that the pain was not relieved and that his fingers began swelling, he then presented to hospital. The swelling appears to be distributed evenly all over the fingers of his left hand and he has noticed that it has been increasing since his accident. An X-ray was arranged but yielded no evidence of a fracture. On examination, the patient appears to be in obvious pain and clutches his left arm to his abdomen. Swelling is present over his fingers and there is a limited range of movement, namely of flexion and extension. What is the most appropriate step in the management of this patient?
Correct Answer : C
This is a typical case of a sprain injury. A sprain is an injury to a ligament which usually occurs by the ligament being overstretched.
To choose the best treatment option for this patient, it is important to know the main aim of treating a sprain injury.
The usual initial treatment for a sprain is described as paying the PRICE.
P: Protect
R: Rest
I: Ice
C: Compression
E: Elevation
A high-arm sling is the right option for this patient.
Choose a Question
×Choose a Question
×
Trial Access Limit Reached
You’ve reached the limit of free content. Subscribe to continue learning without restrictions.