

Hello,
Dr. Batman
Hello Doctor, Welcome!
Profile

Name: Batman
Email: batman@gotham.com
PAEDIATRICS
(Total Questions - 285)Q.1. A 3 month old infant presents with recurrent infections and feeding difficulties. His face looks dysmorphic and has a cleft palate. A chest X-ray shows absent thymic shadow. What is the most likely diagnosis?
Correct Answer : C
DiGeorge syndrome is a deletion of chromosome 22q11.2. It causes absent thymus, fits, small parathyroids (thus decreased Ca2+), anaemia, lymphopenia, low levels of growth hormone, and low T-cell immunity. It is related to the velocardiofacial syndrome: characteristic face, multiple anomalies, eg cleft palate, heart defects, cognitive defects Developmental delay, facial dysmorphism, palatal dysfunction, and feeding difficulties are seen in most infants with this syndrome.
The facial dysmorphism is typically mild but fairly typical. These include hypertelorism, hooded eyelids, tubular nose, broad nose tip, small mount, and mild ear abnormalities.
The most important factor to memorize here is the absent thymic shadow which is pathognomic for DiGeorge syndrome.
Mnemonic: CATCH-22
• Cardiac abnormality (commonly interrupted aortic arch, truncus arteriosus, and tetralogy of Fallot)
• Abnormal facies
• Thymic aplasia
• Cleft palate
• Hypocalcaemia / Hypoparathyroidism
• With the 22 to remind one the chromosomal abnormality is found on the 22 chromosome.
Q.2. A 4 year old boy is referred by the GP to the paediatrician with a cervical lymphadenopathy that is 2 cm in size. His mother says that she thinks the lymph node is growing. It was first noticed 6 weeks ago. The child is generally well with no complaints of tenderness. He has no history of fever. On examination, the spleen is not palpable and there are no other palpable lymph nodes around the body. The cervical lymph node is firm, non-tender and immobile. His throat is clear with no signs of infection. What is the most appropriate initial investigation to perform?
Correct Answer : A
All the above tests are appropriate but the number one test to do if you had to choose would be to perform a full blood count and blood film to look for evidence of haematological malignancies such as leukaemia or lymphoma. A lymph node that is increasing in size and larger than 2 cm should be a worry.
There are many causes of lymphadenopathy in children which include CMV, EBV, Kawasaki disease, and tuberculosis but the one diagnosis that you do not want to miss is haematological malignancies.
An ultrasound of the lymph node is appropriate since it persists beyond 16 weeks, isolated, larger than 2 cm, and increasing in size. However, it would not be the initial test to perform.
Q.3. An 8 year old boy is brought by his mother to the emergency department with bruises on his lower back and a left shoulder dislocation. The child currently lives with his stepfather. The young boy is quiet and makes no eye contact while in conversation. What is the most likely diagnosis?
Correct Answer : C
This is a frequent paediatric topic on exam. This is a case of non-accidental injury. Having a non-biological father in the picture is always a hint of non accidental injury in exam.
Non accidental injury Presentation:
Delayed admission into hospital or clinic by carer
Child usually brought in by step-father or boyfriend
Bruising of varying degrees, color variations (means long-term abuse)
Fractures
Diagnosis: Mostly clinical history
Treatment:
- Admit to ward and manage pain
- Refer to social services
- Treat any other underlying medical conditions.
Q.4. A 5 year old boy is brought to clinic by his mother. The young boy has a distinct nasal speech and snores heavily at night. He is hyperactive during the day but has poor concentration. He is noted to be constantly breathing through his mouth. What is the most appropriate action?
Correct Answer : B
The likely diagnosis here is obstructive sleep apnoea syndrome. Referrals are usually to paediatric physicians, although sometimes paediatric neurologists, respiratory doctors, or ENT consultants may have a specialist interest.
Obstructive Sleep Apnoea Syndrome in Children is mainly due to enlarged tonsils and adenoids.
Presentation :
- Snoring ; usually parents seek attention; many will just get better as they grow older
- Mouth breathing - Witnessed apnoeic episodes
- Daytime sleepiness and somnolence are common in childhood OSAS, in contrast with adults who often fall asleep during the day
- Sleep deprived children tend to become hyperactive, with reduced attention spans, and be labeled as difficult or disruptive, or even ADHD.
They may not be doing well at school due to poor concentration
Investigations:
- Overnight in-laboratory polysomnography (PSG) continues to be the gold standard instrument
* During sleep studies the following are usually monitored:
Oxygen saturation and heart rate.
Airflow at nose or mouth.
Chest and abdominal movements.
ECG, electroencephalogram, electromyogram, and sometimes electrooculogram (eye movements).
Q.5. A 4 week old female infant presents to the Emergency Department with vomiting after every feed. The mother describes the vomiting as projectile and non-bilious. The child is also constipated. On examination, there is a right sided olive-sized abdominal mass on palpation. What is the most appopriate next step of action?
Correct Answer : C
This is a classic presentation of pyloric stenosis. As the child is vomiting profusely, there will be an electrolyte imbalance. Hypokalaemia may be present and therefore needs to be corrected immediately. In reality, one would take blood for serum potassium levels and arrange an abdominal ultrasound while waiting for the serum potassium results. However, the exam writers want you to think about which is the most important given the stem.
Pay attention to the final line of the question.
If the question is asking for the NEXT STEP of action, serum potassium levels would be appropriate.
If the question is asking for the NEXT STEP TO DIAGNOSE the condition, then an abdominal ultrasound would be the answer. Intravenous fluid should follow after taking blood.
Presentation:
- Projectile non-bilious vomiting
- Age group: 3-8 weeks
- Olive-sized abdominal mass
- The child will feel hungry and want to feed despite constant vomiting
Diagnosis:
- Abdominal ultrasound
Treatment:
- Metabolic alkalosis : correct electrolyte imbalance + hydration
- Then referral to paediatric surgery (pyloromyotomy) + nasogastric tube.
Q.6. A 4 year old girl presents to the emergency center with difficulty breathing and stridor. She has a temperature of 39.1 C. The parents state that the child had been in her usual state of health but awoke with a hoarse voice, and difficulty swallowing. They tell you that she has not been immunised because they are afraid of the side effects of the vaccination. What is the most likely diagnosis?
Correct Answer : D
The most worrisome and likely diagnosis here is acute epiglottitis. The fact that she is not immunized and has a high temperature along with difficulty swallowing gives the likelihood of this being acute epiglottitis. If the question was asking for management, summon the most experienced anaesthetist to intubate before obstruction occurs.
Acute epiglottitis :
- Now rare due to the introduction of the Hib vaccine. However, it is still a serious infection. Prompt recognition and urgent treatment are essential.
- Caused by Haemophilus influenzae type B
Features :
- Rapid onset - High temperature
- Stridor
- Drooling of saliva
- Difficulty speaking
- Muffling or changes in the voice.
Q.7. A 2 week old male, term infant presents to the Emergency Department with a sudden onset of green, bilious vomiting for two hours and blood in diapers. Abdominal x-ray reveals dilatation of the stomach and in the proximal loops of the bowel. Barium enema indicates partial obstruction of the duodenum and malposition of the caecum. Which of the following is the most likely diagnosis?
Correct Answer : C
When you see a sudden onset of green, bilious vomiting and blood per rectum in neonates for the exam, think of malrotation with volvulus. EXAM may have an abdominal x-ray result as a “double bubble sign”. Pyloric stenosis in exam would have projectile vomiting as a key feature and the age would be older than 3 weeks.
Intussusception is uncommon in neonates and would most likely occur in infants 6 months or older.
Note that it may be possible in EXAM for them to show an x-ray for case stems so instead of having a description of the result you may need to interpret the radiology yourself.
Malrotation and volvulus presentation:
- Green, bilious vomiting
- Blood per rectum - Sudden onset
- Age: neonates
Diagnosis:
- Abdominal x-ray
- Barium enema
Treatment: ABCDE protocol
- Decompression with nasogastric tube & Referral to paediatric surgery for laparotomy and resection.
Q.8. A 5 month old child is unable to speak but makes sounds. She can hold things with her palm, but not with her fingers. She smiles and laughs and is not shy. She cannot sit independently but can hold her hand and sit when propped up against pillows. What is the best development stage to describe this child?
Correct Answer : A
Only around 12 months does the child say his/her first words. E.g. “mama” Smiling, laughing, and being not shy is normal for her age group.
Only around 7 to 8 months do babies sit unsupported. Refer if by 12 months if unable to sit unsupported. Holding using her palms at her age group is normal.
Developmental milestones are a commonly asked question in. Try to memorize some basic ones.
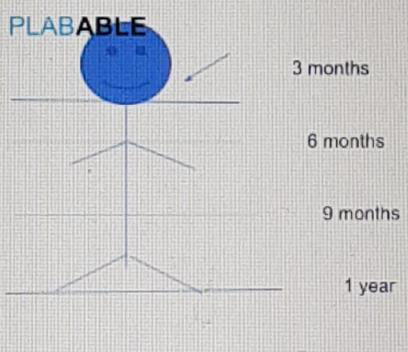
PAEDIATRIC DEVELOPMENTAL MILESTONES :
6 weeks - Good head control, Fixes and follows face, Still in response to sound, Smiles
3 months - Neck holding, Hands open half the time, Startle at loud noise, cooing, Recognizes mother.
6 months - Rolls over, Transfers hand-to-hand, Monosyllabic (mostly babbles), Knows familiar directions (supine to prone)
9 months - Gross motor- Crawling, sit with support, pulls to stand. Fine motor - Pincer grasp, Language - Bi-syllabic (“Mama”, “bye bye”), Social - Stranger fear, holds/bites food.
1 Year - Gross motor -Walks independently, Fine motor - Stacks two blocks, Throws objects Language - Two words with meaning, Social - Wave, clapping.
2 years - Gross motor - Running, up and down steps holding on, kicks ball, Fine motor - Stacks four blocks, makes or copies straight lines, Language - Simple sentences (with 2 to 4 words), Social - Copies others.
3 years - Gross motor - Tricycle, walks up and down stairs, one foot on each step, Fine motor - Stacks eight blocks, makes or copies circles, Language - Can tell name, age, gender, Social - Dresses and undresses self.
4 years - Gross motor - Hops, jumps, walks, Fine motor - Stacks twelve blocks, Language - Tell Stories, poems, Social - Cooperates with other children.
5 years - Gross motor - Skips (both legs above ground), Fine motor - Can draw a person with at least 6 body parts, copies a triangle and other geometric shapes Language - Understands complex instructions, Social - Wants to please friends.
Here are some ways to memorise this table. This figure is intersected at 4 different levels of the body which represent different time frames.
• 3 months – Neck – Holds neck • 6 months – Body – Rolls both directions
• 9 months – Knees – Crawling
• 12 months – Feet – Walks
For fine motor skills :
• At 2 years – Draws a line
• At 3 years – Draws a circle
• At 4 years – Draws a cross and square
• At 5 years – Draws a triangle
Below are certain negative indicators (things a child cannot do) by a certain age that you should recognise and refer to a specialist community paediatric assessment:
• Unable to sit unsupported at 12 months of age
• Unable to walk by 18 months of age
• No speech at 18 months of age
• Unable to run by 2.5 years of age
• Unable to hold objects placed in hand by 5 months of age
• Unable to reach for objects by 6 months of age
Q.9. An 8 year old child is brought into A&E with a fractured leg. The parents are unable to explain how the leg fractured. X-rays reveal several other fractures in various stages of healing. The parents cannot explain what might have caused them. On examination, the child has a blue sclerae and difficulty hearing. What is the most likely diagnosis?
Correct Answer : C
There is frequently a history of multiple bony fractures with no history of trauma. Scenes like this may occur which may lead you to think of non-accidental injuries (e.g. child abuse). But in this case, the cause of the fractures is not child abuse. It is osteogenesis imperfecta (OI). Osteogenesis imperfecta is an inherited disorder of type I collagen that results in fragile, low-density bones.
The bones break easily often from little or no apparent cause.
A person with osteogenesis imperfecta may sustain just a few or as many as several hundred fractures in a lifetime.
Stem may give a scenario like the above but they will have to give some other sign that it is not a non-accidental injury. In this case, they gave the sign of blue sclerae and hearing loss which is found in osteogenesis imperfecta.
Q.10. A 13 year old girl with several years of elevated liver enzymes of unknown etiology presents to clinic with a slow deterioration in her school performance. On examination, there is hepatosplenomegaly, intention tremor, dysarthria and dystonia. Her urinalysis has elevated levels of glucose, protein, and uric acid. What is the most likely diagnosis?
Correct Answer : D
Stem clues for Wilson’s disease: there will be behavioral changes, liver dysfunction, and Kayser-Fleischer rings.
Option C, while similar to Wilson’s, does not exhibit neurological or behavioral changes. Hereditary haemochromatosis is iron overload and also does not exhibit the neurological or behavioral changes typically found in Wilson’s.
Wilson’s Disease presentation:
- Kayser-Fleischer rings
- Liver dysfunction - deranged liver function tests, cirrhosis
- Neurological - ataxia, dysarthria, dystonia
- Behavioural personality changes, decreased school performance
Diagnosis:
- Wilson’s disease scoring system : score > 4
- Serum ceruloplasmin - initial
- Measurement of hepatic parenchymal copper concentration
- Definitive Treatment: Choice of D-penicillamine; trientine; ammonium tetrathiomolybdate
- Neurological involvement - zinc
- First line - Acute liver failure/cirrhosis
- Liver transplant - definitive treatment.
Q.11. An 18 month old boy has been brought to the emergency department by his mother because he has been refusing to move his left arm and crying more than usual for the past 24 hours. He has recently been looked after by his mother’s new partner while she attended college. Assessment shows multiple bruises on his body and the medial aspect of his left upper arm. What is the most appropriate next step?
Correct Answer : B
The likely diagnosis here is a non-accidental injury.
Bruising in unusual sites (eg medial aspect of upper arms or thighs) should prompt consideration of non accidental injury.
The child needs to be admitted for further investigation and also to prevent further injury from the mother’s partner.
Non accidental injury
Presentation:
- Delayed admission into hospital or clinic by carer
- Child usually brought in by step-father or boyfriend
- Bruising of varying degrees, color variations (means long-term abuse)
- Fractures
Diagnosis:
- Mostly clinical history
Treatment:
- Admit to ward and manage pain
- Refer to social services
- Treat any other underlying medical conditions.
Q.12. A 12 month old male infant presents to clinic because his mother is concerned that the child cannot sit on his own, crawling but not standing with support, unable to pick up small items, and is not socially interactive with his older sibling. What is the best management?
Correct Answer : B
For the exam, it is important to memorize the development milestones. The questions that come up for development are similar to the ones above. A scenario is presented where the mom is concerned and you would be told to give the best advice / management. You must answer accordingly depending on the scenario.
This child is clearly showing indications of developmental delay and therefore requires assessment. Infants are usually able to sit without support at 7-8 months.
At 12 months, if they are unable to do this, we should assess and refer.
At 12 months, he should be able to walk with support. A concern would be if he is unable to stand holding on by 12 months.
Q.13. A 3 year old girl ingested 10 capsules from her grandmother’s medication bottle thinking it was candy. By the time the child is in the Emergency Department, she is drowsy and lethargic. Paramedics noted myoclonic twitching. ECG reveals tachycardia and widened QRS. Potassium is elevated. What most likely medication did the child ingest?
Correct Answer : A
This is a diagnosis of tricyclic antidepressant (TCA) overdose. This topic overlaps with toxicity and emergency medicine.
This is a typical exam stem: there is a child who accidentally ingests an unknown bottle of medications.
For TCA overdose, look for widened QRS, peaked T waves, and hyperkalemia as main clues.
Note that in young children (< 5 years) the symptoms would usually be drowsiness, lethargy, and in this stem indications of seizure. In adolescents and adults, you would see more predominant signs of hypertension turning into hypotension and ventricular dysrhythmias along with the widened QRS clue.
Tricyclic antidepressant overdose -
Presentation:
- Child ingesting an unknown bottle of medication
- Lethargy, drowsy - +/- Coma or seizure
- ECG
- Widened QRS, peaked T waves (indications of hyperkalemia)
Diagnosis:
- Urea, electrolytes, toxicology screen - ECG
- Arterial blood gas
Treatment: ABCDE protocol
- If within 1 hr of ingestion and > 4mg/kg
- Activated charcoal - Sodium bicarbonate
- Correct electrolytes if necessary.
TRICYCLIC ANTIDEPRESSANT (TCA) OVERDOSE :
Tricyclic antidepressant (TCA) overdose should always be considered potentially life-threatening. They can deteriorate very rapidly sometimes within 1 hour of ingestion.
Clinical features :
• Dilated pupils
• Dry mouth
• Dry flushed skin
• Urinary retention
• Drowsiness and altered mental state leading to coma
• Hypotension ECG monitoring for TCA overdose is essential.
The important ECG finding suggestive of TCA poisoning is QRS widening (> 100 ms). Broad complex tachycardias may occur which are life-threatening.
Two popular stems in the exam where the answer is likely to be TCA overdose is the young child that takes his/her grandparents’ medication and later becomes drowsy and lethargic.
Another is an elderly person who has a terminal illness and wants to take his/her own life and who comes into the ED having dry and flushed pupils dilated. TCA’s are a prescription-only medication so you should think about how the person in the stem obtained the medication before you choose an answer.
Q.14. A 6 year old boy presents to clinic with obesity. He has a history of failure to thrive as an infant. He is now behind in school, has difficulty interacting with friends, and feeds constantly. His mother says he cannot stop eating. What is the most likely diagnosis?
Correct Answer : C
Prader Willi syndrome is a result of chromosomal abnormality in chromosome 15 on the paternal side. The key clue is behavioral problems and uncontrolled feeding habits.
There may sometimes be clues in the stem stating the child has “blue eyes and blonde hair”.
Presentation:
- Male with blonde hair, and blue eyes
- Behavioral problems
- If uncontrolled feeding + obesity, the boy usually < 6 years old
- Developmental delay
Diagnosis :
- Chromosomal analysis: abnormality of paternal chromosome 15
- Mostly clinical diagnosis
Treatment:
Referral to paediatric psychiatry for behavioral problems and developmental delay.
Q.15. A 13 month old female baby presents to the emergency department with dificulty in breathing. On examination, she has intercostal recessions and a bilateral widespread wheeze. Her temperature is 37.9 C and respiratory rate is 35 breaths/minute. What is the most likely diagnosis?
Correct Answer : D
Bronchiolitis is very common in infants and young children. Their early symptoms are those of a viral upper respiratory tract infection including mild rhinorrhoea, cough, and fever. The fever is usually high (above 39°C) however in this stem a temperature of 37.9°C is given. Do not let that fool you into thinking that it is not an infective cause.
Other symptoms of bronchiolitis include wheeze. Occasionally, one may find symptoms of cyanosis and poor feeding in the stem.
Bronchiolitis - An acute infectious disease of the lower respiratory tract that occurs primarily in the very young, most commonly infants between 2 and 6 months old
- Respiratory syncytial virus (RSV) is the pathogen in 75-80% of cases It is a clinical diagnosis based upon:
- Breathing difficulties - Cough - Coryzal symptoms (including mild fever)
- Decreased feeding
- Apnoeas in the very young
- Wheeze or fine inspiratory crackles on auscultation
Management :
- Largely supportive involving humidified oxygen.
Q.16. A 6 week old child is brought to A&E with persistent non-bilious vomiting. The child feels hungry and wants to feed despite constant vomiting. Biochemistry shows K+ of 3.1 mmol/L. What is the most likely diagnosis?
Correct Answer : B
Hypokalaemia and non-bilious vomiting should direct you toward pyloric stenosis as a diagnosis.
It is unlikely to be duodenal atresia as the newborn presents with bilious vomiting with every feed. In this question, the scenario was one of non-bilious vomiting.
Malrotation is manifested by bilious vomiting, crampy abdominal pain, abdominal distention, and the passage of blood and mucus in their stools. Again in this scenario, non-bilious vomiting was given.
Pyloric stenosis :
- Projectile non-bilious vomiting
- Age group: 3-8 weeks
- Olive-sized abdominal mass
- The child will feel hungry and want to feed despite constant vomiting
Diagnosis:
- Abdominal ultrasound
Treatment: - Metabolic alkalosis
Correct electrolyte imbalance + hydration, then referral to paediatric surgery (pyloromyotomy) + nasogastric tube.
Q.17. A 3 year old boy is brought to A&E after having a generalized tonic-clonic seizure that lasted approximately 5 minutes. The parents say that he was previously well but started developing symptom s of a cold earlier in the morning. He is noted to have a fever of 39 C. What is the most likely diagnosis?
Correct Answer : C
Febrile seizures are common in children and usually occur in ages 6 months to 6 years. They occur in 3% of all children in this age group. Management for this patient would involve antipyretics.
FEBRILE SEIZURES :
Febrile seizures are epileptic seizures accompanied by fever in the absence of an intracranial infection.
Key points -
• Usually between 6 months to 6 years of age with a peak at 14-18 months
• Usually with a positive family history
• Temperature usually increases rapidly to > 39 C
• Typically a generalized tonic-clonic seizure is seen
• Must determine the cause of fever and rule out meningitis
Types :
• Simple febrile seizures are the most common type and are characterized by a single generalized seizure lasting less than 15 minutes.
• Complex febrile seizures include those that are focal, prolonged, or recurrent It is important to know the figures for febrile seizures as parents often ask questions like “Would this seizure happen again” and “Would this lead to epilepsy in the future.
• About 1 in 3 would have further episodes of febrile seizures.
• About 1 in 3 who have further episodes would develop epilepsy (this means roughly about 10% of complex febrile seizures would develop epilepsy)
Treatment :
• Antipyretics to control the fever
• Seizures lasting more than 5 minutes should be managed with benzodiazepines (i.e. buccal midazolam).
Q.18. A 4 year old girl attends clinic with a history of diarrhoea, bloating and abdominal pain. She is failing to thrive. Blood tests reveal a hypochromic microcytic anaemia. Alpha gliadin antibodies are positive. What is the most likely diagnosis?
Correct Answer : D
The key word here is the alpha gliadin antibodies which are positive. This is a test for coeliac disease.
Coeliac disease: an example of malabsorption associated with exposure to gluten, rye, wheat, barley.
Malabsorption typically presents with diarrhoea, failure to thrive, and anaemia. As subclinical/latent forms exist, investigate any unexplained anaemia, fatigue, ‘irritable bowel’ symptoms, and diarrhoea. Patients mostly present between 6 months to 2 years of age but can occur at any age.
There may be a deceleration on the growth chart after introduction to gluten at weaning (4–6 months).
Diagnosis Immunology:
- Raised IgA anti-tissue transglutaminase (IgAtTG), anti-gliadin (IgA-AGA), and endomysial antibodies (EMA)
Biopsy: Confirm by finding villous atrophy on small bowel biopsy (gold standard).
Q.19. A mother calls the postnatal ward with concerns of her newborn. Her baby was born at term by an uncomplicated vaginal delivery in the birthing centre yesterday evening. The baby is feeding well and not irritable. This is parents’ first child and the parents are especially concerned as the baby has a yellowish colour to his skin and eyes. What is the most appropriate management?
Correct Answer : B
Neonatal jaundice within the first 24 hours of life should ring alarm bells in your head. They would require urgent assessment within two hours according to NICE guidelines. Investigations such as transcutaneous bilirubin measurement, liver function test, full blood count, blood film, blood group, Coomb’s test, G6PD levels, and review for sepsis would be performed in the hospital.
Q.20. A 13 month old child is assessed for developmental milestones. He holds furniture to help him stand and walk. He can say ‘mama’ and ‘papa’ but is unable to join two or three words in sentences. He makes eye contact and smiles to his mom but he is very shy around strangers. He can transfer objects from one hand to another. He responds to his name. What is the best development stage to describe this child?
Correct Answer : D
Developmental milestones are frequently asked. In this stem, his developmental milestones are correct for his age. At a 12 month mark, they should be able to do the following:
Language and hearing :
• Says “dada”, and “mama” to parents
• Vocalises two or three other words with meaning
Gross motor skills :
• Sits well and for an identified period
• Can rise independently from the lying position to the sitting position
• Can cruise around furniture
• May be able to stand alone
Fine motor skills :
• Can pick up small objects
• Can bang two bricks together
Personal and social milestones :
• Stranger anxiety
• Can drink from a cup
Investigation is prompted in the following red-flag situations :
• No smile by 8 weeks
• Poor eye contact by 3 months
• No reaching by 5 months
• Not walking by 18 months
• No single words with meaning by 18 months
• No 2-3 word sentences by 30 months.
Q.21. A 2 year old boy fell off his tricycle and hurt his arm. He got up and was about to start crying but before there was any sound, he went pale, and unconscious. He recovered after 2 minutes but remained pale. His colour came back after a few minutes. His mother was concerned at that time that he was going to die. She is very worried and mentions that he had a similar episode 2 months ago after falling down some steps. What is the most appropriate next step?
Correct Answer : A
The diagnosis here is breath-holding spells. This usually occurs in young children when they are upset and can be precipitated by trauma or when separated from their parents. Anything which may upset a child including injury from falling down. These children stop breathing for some time, they may turn blue or have little jerks of the limbs.
After some time, they spontaneously start breathing. They become completely fine after an hour. Treatment is not necessary. Usually just reassure parents.
Q.22. A 3 month old term female infant presents to clinic with frequent episodes of non-projectile vomiting after feeds. She is exclusively breastfed. The mother complains it is difficult to breastfeed her child as she often gags, and chokes during feeds. Shortly after feeding, she occasionally would display signs of distress, cries and refuses feeds. On examination, the infant is irritable and she is below centiles on the growth chart in terms of weight. What is the most likely diagnosis?
Correct Answer : B
This is a diagnosis of gastro-oesophageal reflux disease (GORD). This is one of the most common causes of vomiting in infants. This is due to slower gastric emptying time, a weaker oesophageal sphincter, an inability to sit up, and an entirely liquid diet.
Episodes of gagging and regurgitation can occur throughout the day. While GORD can occur at any age, in paediatrics the case stem would usually have an infant < 1 year old. This is because, in the vast majority of cases (90%), reflux would be resolved by 1 year of age. If it still has not been resolved by 1 year, then there might be another pathology such as a hiatus hernia.
It is common for growth to plateau off if the infant has persistent GORD and it is one of the more worrying features which warrants treatments.
GASTRO-OESOPHAGEAL REFLUX DISEASE :
Presentation:
- Age group for < 1 year
- Excessive and frequent episodes of regurgitation / vomiting after feeds
- Difficult to feed - Failure to thrive
- Irritable and crying
Diagnosis:
- Upper GI study with contrast as per protocol only (do not offer routinely)
- First line is upper GI endoscopy with biopsy as per protocol only (do not offer routinely)
Treatment:
- If breast-feeding: Breast-feeding assessment
- If formula-fed: take feeding history increase feeding frequency and reduce the amount per feed thickened formula
- Only prescribed proton pump inhibitors (PPIs) or H2 receptor antagonists (H2RAs) and consider enteral feeding only if there is no improvement to the above.
Q.23. A 6 year old boy is brought to clinic by his mother. She says that he is still unable to keep dry at night and will be attending a sleepover party at a friend’s house. She says that it would be embarassing if he wets himself during the sleepover and she wants to know if anything can be done. The child does not wet himself during the day. What is the most appropriate management?
Correct Answer : C
For children older than 5 years of age, if rapid or short-term control of bedwetting is required (for example for sleepovers or school trips), offer treatment with desmopressin.
PRIMARY ENURESIS MANAGEMENT :
The management of bedwetting can be a little confusing as different sources and books would have slightly different answers.
The points on NICE CKS can be summarized below:
Primary bedwetting (without daytime symptoms) - Younger than 5 - reassurance.
Older than 5 years of age - If the bedwetting is infrequent (less than 2x a week) - reassurance.
- If long-term treatment is required- enuresis alarm (1st line) + reward system
- If short-term control of bedwetting is required (e.g. sleepovers) - Desmopressin
If treatment has not responded to at least two complete courses of treatment with either an alarm or desmopressin - Refer to secondary care
Primary bedwetting (with daytime symptoms) - Refer all children above 24 months with primary bedwetting and daytime symptoms to secondary care or an enuresis clinic for further investigations and assessment.
Q.24. An 8 year old child has recurrent throat infections. He feels tired and lethargic all the time. Petechiae is noticed on his lower limbs. On examination, splenomegaly and gum hypertrophy was noted. Blood results show: Hb 6.8 g/dL WCC 7 x 109/L Platelets 75 x 109/L. What is the most likely diagnosis?
Correct Answer : D
These symptoms that he is presenting are due to pancytopenia. The likely cause given the options and his age is acute lymphoblastic leukaemia (ALL) The commonest leukaemia in children is acute lymphoblastic leukaemia (ALL). One needs to be careful with picking AML or ALL as there are often questions with a very similar stem.
In reality, it is difficult to diagnose them clinically as well.
For the exam, if one sees a clinical picture of acute leukaemia in a very acute setting with bleeding from the gums, AML is likely to be the answer. On the other hand, if one sees a clinical picture of acute leukaemia but less acute and only with gum hypertrophy, ALL is likely to be the answer. - Can these differences be used in real life? Probably not!
Q.25. A 10 month old male infant presents with a 6 hour history of crying and passage of loose, bloody stool. On examination, the infant is irritable, with intermittent drawing up of his knees to his chest, and a temperature of 38.8 C. A currant jelly-coloured blood is seen in his stools. What is the most likely diagnosis?
Correct Answer : D
This is a diagnosis of intussusception.
Note the clues: the infant is between 5-12 months, the child has been crying persistently (indication of abdominal pain), drawing the legs up to the chest, currant jelly blood in stool, and a sausage-shaped mass.
This along with pyloric stenosis and malrotation with volvulus is a common paediatric surgical question. Know the differences between each.
Intussusception :
TRIAD of: Abdominal pain, Currant jelly blood in stool , Sausage shaped mass on palpation (often in the right upper quadrant)
- Child is crying persistently
- Drawing up of legs
- May be vomiting if severe
Diagnosis:
- Abdominal ultrasound may show doughnut or target sign
- Bowel enema
Treatment:
- Air enema reduction or laparotomy
Remember:
“Red currant jelly” stools are pathognomonic for intussusception.
Q.26. A 2 year old has atrophy of the buttocks. He has often had bloating of his abdomen with frequent offensive, smelly stools that are difficult to flush. He looks pale on examination. What is the most appropriate initial investigation?
Correct Answer : B
The diagnosis here is coeliac disease. Bulky, frothy, and floating (difficult to flush) stools are a hint that he is having a malabsorption syndrome. He looks pale because he is anaemic.
If you have answered A (Sweat chloride test) for cystic fibrosis. You are not completely wrong as cystic fibrosis can occur at that age as well and has symptoms of malabsorption too (foul-smelling bulky stool that "floats).
But the question writers are likely to give other hints like “repetitive cough over the last few months” if cystic fibrosis is the likely diagnosis. Also, given the two diseases, coeliac is much more common compared to cystic fibrosis, and thus the most likely investigation that would lead to a diagnosis is anti-endomysial antibodies.
Q.27. A 9 year old girl with cystic fibrosis is discussing her problems with you and wishes to know the reason for her repeated pulmonary problems. What is the most likely cause of her pulmonary symptoms?
Correct Answer : B
Due to the CTFR gene, there are abnormal chloride channels in the epithelial cells. This causes abnormal fluid production which results in increased thickening of mucus hence increasing the changes of pulmonary infections. Ciliary dysfunction is seen in Kartagener’s syndrome.
CYSTIC FIBROSIS is an autosomal recessive disorder that induces low salt and chloride excretion into airways leading to increased viscosity of secretions
Clinical presentation :
- Recurrent chest infections (Cough and chronic sputum production)
- Recurrent chest infections may lead to bronchiectasis
- Malabsorption leading to frequent, bulky, greasy stools (Steatorrhoea), failure to thrive
- Pancreas increased incidence of diabetes mellitus
- Delayed sexual development
- Male infertility, female subfertility
- Salty taste of skin
- Short stature
- Meconium ileus (in neonatal period)
Diagnosis :
• Primarily made during newborn screening (Guthrie test) All newborn infants are screened for cystic fibrosis using the heel-prick test.
The majority of them would be identified using this method If this is positive, then molecular genetic testing for the CTFR gene and sweat test would follow.
• If not picked up by newborn screening and later on develops clinical manifestations of cystic fibrosis, then perform sweat test or genetic testing for the CFTR gene.
Q.28. A 5 year old boy presents with drooling of saliva and severe stridor. He has a temperature of 39.0 C and is sick looking. He has difficulty speaking and has muffled voice. A lateral radiograph demonstrates a “thumb sign”. What is the most likely diagnosis?
Correct Answer : C
The given case is classic picture of acute epiglottitis. The thumb sign is a manifestation of an oedematous and enlarged epiglottitis which is seen on lateral soft-tissue radiograph of the neck, and it suggests a diagnosis of acute infectious epiglottitis. The second clincher here is drooling of saliva. If you find any questions with a child with drooling of saliva.
It is likely that this is acute epiglottitis, Summon the most experienced anaesthetist to intubate before obstruction occurs.
Acute epiglottitis - Now rare due to the introduction of Hib vaccine. However, it is still a serious infection.
Prompt recognition and urgent treatment is essential.
Caused by Haemophilus influenzae type B.
Q.29. A 12 year old girl presents to clinic with sudden onset of pallor, palpitations, and difficulty breathing while running on the school track. After 30 minutes, her symptoms resolved. This is a first time event and she has never been cyanotic. Cardiac examination was normal. Chest x-ray and echocardiogram were normal. ECG reveals evidence of pre-excitation, delta waves, and prolonged QRS. What is the most likely diagnosis?
Correct Answer : B
This is a diagnosis of Wolff-Parkinson-White (WPW) syndrome. The age group for the case stem may present itself in older age (i.e. 20-30).
However, the features are similar to the stem above. Note the ECG features, especially delta waves and pre-excitation pathway.
Wolff-Parkinson-White syndrome :
- Child may be exercising with sudden onset of pallor, difficulty breathing, and palpitations followed by spontaneous recovery
- Otherwise, an asymptomatic child
- ECG: delta waves, pre-excitation pattern, prolonged QRS, shortened PR.
Diagnosis:
- ECG - 24 hour Holter monitor
Treatment:
- Catheter ablation - first line
- Medications : flecainide and propafenone.
Q.30. After several episodes of urinary tract infections, a 2 year old girl undergoes a micturating cystourethrogram which reveals mild dilation of the renal pelvis and reflux into the ureters and kidney. She is currently not on any medication. Which of the following is the most appropriate next step in treatment?
Correct Answer : C
This is a diagnosis of vesicoureteral reflux (VUR). For urology questions in paediatrics in this exam, pay particular attention to VUR and urinary tract infections.
Do not go into details for these questions, just know the basic presentation, diagnosis, and management according to current guidelines.
According to guidelines, she would start with low-dose antibiotic prophylaxis before consideration for surgery.
Vesicoureteral reflux : A condition where urine flows retrograde from the bladder into ureters/kidneys.
Presentation :
• Most children are asymptomatic
• Increases risk of urinary tract infection
Thus, symptoms of UTI: Fever, Dysuria, Frequent urination, Lower abdominal pain.
Diagnosis :
• Urinalysis, urine culture, and sensitivity initial investigation.
• Renal ultrasound initial investigation might suggest the presence of VUR if ureteral dilatation is present.
• Micturating cystourethrogram gold standard
• Technetium scan (DMSA) for parenchymal damage (seen as cortical scars)
Treatment :
• VUR grade I-IV
- Start with low-dose antibiotics prophylaxis daily (i.e. trimethoprim)
• If the above fails and/or parenchymal damage consider surgery - reimplantation of the ureters. Note that during early childhood, the kidneys are at higher risk of developing new scars.
. So it is particularly important to start parenteral antibiotic treatment for patients with vesicoureteral reflux before febrile breakthrough infections. For patients with frequent breakthrough infections, definitive surgical or endoscopic correction is preferred.
Surgical correction should also be considered in patients with persistent high-grade reflux (grades IV/V) or abnormal renal parenchyma.
Q.31. A 7 year old child is brought in by her mother with complaints of having a fever, sore throat and feeling unwell. She has a maculopapular rash on her trunk and back which appeared a few hours ago. On examination of the throat, there is a white coating on the tongue and tonsils have pale exudates. She has a temperature of 39 C. What is the most likely diagnosis?

Correct Answer : D
Scarlet fever is the diagnosis here. It is common around ages 2 to 8 years. The white coating of the tongue is an appearance of a white strawberry tongue.
Usually, there are also prominent red papillae seen. The rash described is characteristic of the rash of scarlet fever.
The other options remain less likely Roseola infantum (herpes 6 virus) may present with small (< 0.5 cm) blanching, rose-pink rashes with a high fever.
The rash also commonly affects the trunk which is seen in this stem and it can present with a sore throat. However, they do not present with a strawberry tongue. Also, the most common age group that this disease occurs in is around 6 months to 1 year. Note that roseola infantum, similar spots occur on the soft palate and uvula called Nagayama spots. Rubella usually has a rash that starts behind the ears and spreads from there to the rest of the face or body.
Measles is usually present in a more unwell child with a fever of more than 40 C. The red spots begin on the face and behind the ears and spread over 24 to 36 hours covering the majority of the body except the soles and palms. The spots can initially be as big as 1 cm in diameter and often appear together.
SCARLET FEVER : Key points Commonest in ages 2 to 8 years old
• Caused by group A streptococcus pyogenes
• Rash and fever are caused by toxins released by bacteria
• Diagnosis is clinical
• Presents with a sore throat, fever (usually more than 38.3 C), and a rash.
• Rash: Starts on torso 12 to 48 hours after fever and spreads to extremities, has a coarse texture like sandpaper
.• Other features : Strawberry tongue, Cervical lymphadenopathy, Tonsils covered with pale exudates with red macules on the palate (Forchhemier spots)
• Treatment is with penicillin V for 10 days.
Picture of strawberry tongue below.
Q.32. Following an emergency caesarean section for fetal distress, a baby is in poor condition. His heart rate is 90 beats/minute. He is blue at extremities but his body is pink. He has some limb flexion and muscle tone. He is gasping for air irregularly and grimaces on aggressive stimulation. What Apgar score does this newborn infant have?
Correct Answer : B
Apgar score is a scoring system used to evaluate a newborn baby. It is done at 1 minute and 5 minutes after birth. It may be repeated at 10 minutes if scores remain low.
The Apgar score is calculated by adding the total score of 5 components.
Score 0:
Skin color - Blue or pale all over
Pulse rate - absent , Reflex irritability
Grimace - No response to stimulation
Activity - Flaccid
Respiratory effort - Absent
Score 1: Skin colour - Blue at extremities body pink (acrocyanosis) Pulse rate - < 100 beats/minute Reflex irritability grimace - Grimace on suction or aggressive stimulation Activity - Some limb flexion Respiratory effort - Weak, irregular, gasping
Score 2: Skin colour - No cyanosis body and extremities pink Pulse rate - > 100 beats/minute Reflex irritability grimace - Cry on stimulation, sneezes, coughs Activity - Flexed arms and legs that resist extension Respiratory effort - Strong, robust cry Component of backronym: Appearance Pulse Grimace Activity Respiration
Q.33. A 2 year old male presents to the Emergency Department with a left-sided reducible firm swelling near the groin. The swelling descends when the child cries. On examination, both testicles are palpable in the scrotum. What is the most appropriate management?
Correct Answer : B
The diagnosis is an inguinal hernia.
There are no clues in the stem of strangulation; therefore, the herniotomy can be done electively. Most inguinal hernias can be reduced by gentle compression in the line of the inguinal canal.
A paediatric surgeon will do an elective herniotomy on an outpatient basis for this child as long as it can be reduced. Herniotomy is usually performed for children under 10 years. Herniorrhaphy is done in adults.
Herniotomy is where there is ligation of the processus vaginalis which has become the hernia sac. Herniorrhaphy, which is done in adults, involves reinforcing the abdominal wall with a mesh.
There is no need to do an orchidopexy since this patient’s testicles are both palpable in his scrotum and they are not incarcerated. In children, if reduction is impossible, an emergency surgery would need to be performed due to the risk of compromise of the bowels or the testes.
Features of a strangulated hernia include:
• Pain
• Inflammation
• Nausea and vomiting
• Fever
• Features of bowel obstruction such as severe abdominal pain, constipation and abdominal distention.
Q.34. An 8 year old boy presents with severe crushing chest pain. He is stall for his age and has a refractive error for which he wears thick glasses for. What is the most likely syndrome?
Correct Answer : A
A tall, myopic child can only be Marfan’s syndrome in the exam. The cardiovascular symptoms support this diagnosis.
Marfan's syndrome Features;
• Tall and thin
• Long arms, legs, fingers, and toes
• Arachnodactyly (long spidery fingers)
• Flexible joints
• Scoliosis
• Cardiovascular Aortic dilatation or dissection, aortic regurgitation, mitral valve prolapse, mitral regurgitation, abdominal aortic aneurysm
• Lungs pleural rupture causing spontaneous pneumothorax
• Eyes lens dislocation, high myopia.
Q.35. A 14 year old child is brought to the GP surgery by his mother with the complaint of mild dyspnoea. He also complains of coughing up about two tablespoons of mucopurulent sputum per day for about two years now. His past medical history is significant for cystic fibrosis. He has a history of repeated chest infections over the past few yeaers which he was treated with antibiotics. He has an oxygen saturation of 96% and his observations are within normal limits. What is the most appopriate management for this patient?
Correct Answer : D
Cystic fibrosis is often very difficult to manage and usually requires a multidisciplinary team approach. The physiotherapist helps the patient clear the bronchial secretions by physiotherapy, the paediatrics often have to prescribe antibiotics to treat the chest infection and prescribe pancreatic enzyme supplements to correct nutritional deficits. All the answers given have a place in the management of cystic fibrosis and the real challenge here is picking which one is the best.
Chest physiotherapy involves techniques to clear the mucous such as postural drainage where gravity-assisted positions are used to aid drainage. Other techniques include chest percussion and a positive expiratory-pressure device to aid dislodgement and expectoration of sputum. This would improve this patient’s symptoms of dyspnoea and mucopurulent sputum. Although oxygen usually forms part of the initial treatment for anyone presenting with dyspnoea, it is not the most appropriate management for this patient since his oxygen saturation is normal. Antibiotics are indicated in patients with cystic fibrosis only in an acute exacerbation of the disease or as prophylaxis in childhood. The prophylactic antibiotic to offer is flucloxacillin as it works well against respiratory Staphylococcus aureus infection for children with cystic fibrosis. It is offered from the point of diagnosis up to age 3, and consider continuing up to 6 years of age. If a mild exacerbation is present, antibiotics can be prescribed for 2 weeks.
Bronchodilators, specifically beta-2 agonists, are indicated in the management of patients with cystic fibrosis but they only benefit some patients who have a reversible component of their airway obstruction.
The question becomes more difficult to answer because dyspnoea and increased sputum production are considered early signs of an exacerbation in which case bronchodilators, antibiotics, and even corticosteroids have a role.
However, since his observations are well and there is no history of fever or signs of infection, chest physiotherapy still remains the best choice among the answers.
Q.36. A 3 year old child presents with cough, a rash on his face and a high temperature which began 2 days ago. A rash is also seen on his buccal mucosa. His parents state that he was not given routine immunization as the parents were concerned of the adverse effects. The rash is erythematous and maculopapular. What is the most appropriate diagnosis?

Correct Answer : B
This is a classic case of measles. The rash seen on his buccal mucosa is called Koplik spots. He was not given routine immunizations which include measles, mumps, and rubella (MMR) vaccine which if he had the first jab, could have decreased his chance of developing measles.
The distractor here is rubella which can present almost exactly like measles. The key features commonly seen in questions, if rubella (instead of measles) were to be the answer, are swollen lymph nodes.
• Spots on the soft palate (Forschhemier spots). In measles, the spots are on the buccal mucosa and are called Koplik spots.
Measles mnemonic to remember - Hard K sounds Koplik spots, Cough, Conjunctivitis, Coryza.
Prodromal features : irritable, conjunctivitis, fever & pathognomic Koplik spots (before rash): white spots ('grain of salt) on the buccal mucosa- maculopapular rash: starts behind ears and then to the whole body.
Q.37. A 4 year old girl is taken by her mother to the emergency department and complains of pain during urination and feeling generally unwell. She has a temperature of 38.5 C. What is the most appropriate initial action?
Correct Answer : C
The clinical features described are consistent with urinary tract infections for which a clean catch of urine is the next best action. Special arrangements may be needed for collecting a sample from a child. Clean catch, catheter, or suprapubic aspiration are methods used that reduce the risk of contamination.
Routine investigations that are done in urinary tract infections are:
• Dipstick analysis of urine - may treat as bacterial if there are positive results for nitrite and/or leukocytes
• Urine microscopy - leukocytes indicate the presence of infection • Urine culture.
Q.38. A 15 year old boy attended the emergency department with shortness of breath. A diagnosis of spontaneous unilateral pneumothorax was made. He is noted to be tall for his age with long arms and fingers. He also has severe scoliosis. What is the most likely syndrome?
Correct Answer : D
Spontaneous pneumothorax is common in Marfan’s syndrome. The other signs and symptoms point toward Marfan’s syndrome as well.
Q.39. A 4 year old child presents to A&E with fever and stridor. He is unable to swallow his saliva. He has a respiratory rate of 45 breaths/minute. What is the most appropriate next step in management?
Correct Answer : C
The clincher is unable to swallow his saliva. If you find any questions with a child with drooling saliva, this is likely acute epiglottitis. Summon the most experienced anaesthetist to intubate before obstruction occurs. In the above options, securing the airways is the most appropriate.
Q.40. A 3 year old child is admitted to hospital for a very high fever. He is discovered to be below the 25th percentile for weight. After a week in hospital, his weight improves from 10 kg to 11 kg upon discharge. A week later, he is readmitted with pneumonia. His weight upon admission is back to 10 kg and improved to 11.5 kg at the end of 10 days upon discharge. What is the most likely cause of his fluctuating weight?
Correct Answer : B
This is a seemingly tough question which in actuality, is quite simple. The normal weight for a 3-year-old male child is around 14 kg.
We can see from admission that his weight is way below the average for his age group. The fact that his weight improved in the hospital and declined upon discharge is highly suspicious of negligence.
Another clincher to this fact is the frequent hospital admissions. We cannot say this child has leukaemia or cystic fibrosis (although it is possible) because there is no evidence in the stem to suggest this. Thus, the best answer is nonaccidental injury. In certain questions like this one, there is insufficient information to properly know for certain which is the correct answer. These types of questions may reflect those that appear in the exam.
Options C and A are still the top choices.
Make one of these your choices and move on to the next question. Do not overthink this as it could waste valuable time in the exam.
Non-accidental injury / neglect :
• Frequent attendance or unusual patterns of attendance to health care services, including frequent injury.
• Failure to access medical care appropriately (including non-attendance for routine immunizations, and delay in presentation).
• Explanations that are inconsistent over time or between people, or which are not consistent with the presenting features.
• There is evidence of failure to thrive.
• Parents or carers do not administer prescribed medication.
• Inexplicably poor response to treatment.
• Reporting of new symptoms as soon as previous ones resolve.
Q.41. A 4 year old boy, who recently immigrated from Kenya with his parents, presents to clinic with intermittent watery diarrhoea, foul smelling flatulence, nausea, and abdominal pain. His weight is less than the 5th percentile for his age. On examination, he has a fever of 38 C and is dehydrated. Which of the following is the most appropriate investigation to confirm his diagnosis?
Correct Answer : C
Giardiasis Presentation:
- Watery diarrhea, foul-smelling flatulence
- Nausea, belching - Abdominal pain - +/- Fever
Diagnosis: - Stool microscopy - first line
- Stool PCR / ELISA
Treatment: - Hygiene - Metronidazole.
Q.42. An eight day old male neonate presents with vomiting, weight loss and lethargy. Urea and electrolyte blood tests have been done and show his serum potassium level to be 5.2 mmol/L. An ultrasound scan of his abdomen reveals bilaterlaly enlarged adrenal glands. What is the most likely feature to be seen in this patient?
Correct Answer : B
To answer what type of electrolyte imbalance this baby has, we first have to know a little about the condition he has presented with. The child has congenital adrenal hyperplasia.
The bilaterally enlarged adrenal glands in the stem directly point you to this diagnosis. Congenital adrenal hyperplasia has many different forms and varying severity however, it usually presents with the ‘salt-wasting’ form early on in males. The exam is likely to only test the ‘salt-wasting’ form in male children.
Q.43. A 5 week old male infant presents to clinic with jaundice during routine check-up. His mother reports a normal vaginal delivery at term with a birth weight of 3.5 kg. On examination, the baby is irritable, below average centiles for weight, and the liver is enlarged. Pale stools and dark urine on diaper were observed. The mother is currently not breastfeeding and had picked him on formula. What is the most likely diagnosis?
Correct Answer : C
Jaundice in newborns is an important topic within the paediatric section for exam. Understand the mechanisms and management for neonatal jaundice as well the causes of jaundice post 4 weeks of age. Examination results are consistent with obstructive jaundice therefore option C.
Jaundice in option B would occur within 24 hours of birth. Galactosemia would present with vomiting, diarrhea, failure to thrive with jaundice. The liver would not be hard or enlarged.
BILIARY ATRESIA : Biliary atresia is notoriously asked during exams so one should know this topic inside and out.
Presentation:
- Jaundice with pale stools and dark urine
- Usually would present in 3-4 weeks of life
- Splenomegaly is not usually a feature unless the presentation is late
- Failure to thrive is a result of poor absorption
Diagnosis :
- Abdominal ultrasound (initial investigation)
- Cholangiogram (definitive diagnosis)
Treatment :
Kasai procedure = hepatoportoenterostomy.
It is extremely important to diagnose biliary atresia early as without intervention, chronic liver failure will develop which usually leads to death before age 2.
NEONATAL JAUNDICE :
Physiological jaundice -
- This results from increased erythrocyte breakdown and immature liver function.
- It presents at 2 or 3 days old, begins to disappear towards the end of the first week, and has resolved by day 10.
- The bilirubin level does not usually rise above 200 mol/L and the baby remains well.
Early neonatal jaundice (onset less than 24 hours)
Note: The most common pathological causes of neonatal jaundice within 24 hours are:
Rhesus incompatibility, ABO incompatibility, G6PD, and sepsis.
Haemolytic disease: eg, haemolytic disease of the newborn (rhesus), ABO incompatibility, glucose-6-phosphate dehydrogenase deficiency, spherocytosis.
Infection: congenital (eg, toxoplasmosis, rubella, cytomegalovirus (CMV), herpes simplex, syphilis) or postnatal infection.
Crigler-Najjar syndrome or Dubin-Johnson syndrome.
Gilbert's syndrome - Prolonged jaundice (jaundice lasting for longer than 14 days in term infants and 21 days in preterm infants)
Note: The most important diagnosis not to be missed in this group is biliary atresia.
• Hypothyroidism - Congenital hypothyroidism is usually identified on routine neonatal biochemical screening (Guthrie test)
• Hypopituitarism
• Galactosaemia
• Breast milk jaundice: The baby is well and the jaundice usually resolves by six weeks but occasionally continues for up to four months.
• Gastrointestinal (GI): biliary atresia, neonatal hepatitis.
** Biliary atresia (commonly asked question)
Neonatal hepatitis : It is worth knowing a little about the system for newborn jaundice follow-up care following birth for mothers and newborns are delivered by the community midwives.
They would come to visit the mother and newborn at their own homes. If the newborn remains jaundiced after 14 days (or 21 days for premature babies), they are referred back to the hospital to see a paediatrician who would investigate further to rule out other rarer causes of jaundice.
The most important reason that investigations need to be carried out for infants with jaundice lasting longer than 14 days is to diagnose biliary atresia promptly, as delay in surgical treatment in this group could lead to severe complications. A split bilirubin blood test is usually performed to see the levels of conjugated and unconjugated bilirubin.
If hyperbilirubinaemia is unconjugated, the paediatric team is usually reassured since biliary atresia would have high levels of conjugated bilirubin.
Q.44. A 6 week old baby is admitted with persistent vomiting and failure to gain weight. Her mother describes the vomiting as projectile and non-bilious. On examination, there is a right sided olive-sized abdominal mass on palpation. Bloods show the following: Na+ 138 mmol/L K+ 3.3 mmol/L Cl- 83 mmol/L HCO3- 28 mmol/L What is the most appropriate diagnostic test?
Correct Answer : A
Bloods show a hypochloraemic, hypokalaemic alkalosis which points towards the diagnosis of pyloric stenosis. This is diagnosed using an abdominal ultrasound.
Q.45. A 7 month old baby is admitted with a 3 day history of coughing. He has a temperature of 38.5 C. On examination, there is marked subcostal recession and widespread wheeze is noted bilaterally. His respiratory rate is 60 breaths/minute and oxygen saturation is 91%. What is the most appropriate initial management?
Correct Answer : B
The diagnosis here is bronchiolitis. Supportive care is the mainstay of treatment involving oxygen. Oxygen supplementation should be given to children with bronchiolitis if their oxygen saturation is persistently less than 92%. The evidence for using nebulised salbutamol for children with bronchiolitis has always been very shaky.
Currently NICE does not recommend using salbutamol as part of the management for children with bronchiolitis.
Bronchiolitis - An acute infectious disease of the lower respiratory tract that occurs primarily in the very young, most commonly infants between 2 and 6 months old - Respiratory syncytial virus (RSV) is the pathogen in 75-80% of cases.
It is a clinical diagnosis based upon:
- Breathing difficulties
- Cough
- Coryzal symptoms (including mild fever)
- Decreased feeding
- Apnoeas in the very young
- Wheeze or fine inspiratory crackles on auscultation
Management :
- Largely supportive involving humidified oxygen.
Q.46. A 13 year old girl presents to the Emergency Department with weight loss, bloody diarrhoea, and fever intermittently over the last 6 months. The intermittent episodes have caused occasional restriction of activity. Currently she is having moderate abdominal pain. Labs reveal elevated ESR and positive p-ANCA. What is the most likely management for this patient?
Correct Answer : A
This is a diagnosis of ulcerative colitis (UC).
Question would usually have an adolescent (12-17 years) who either presents to the clinic or emergency with the above symptoms. There may or may not be other UC clues: growth failure, toxic megacolon, and affecting only the submucosa of the colon.
In this case, the patient is classified as having mild to moderate UC according to NICE.
Ulcerative colitis in Paediatrics :
- Bloody diarrhea, abdominal pain, tenesmus, vomiting, weight loss, fatigue
- p-ANCA positive
Diagnosis:
- Clinical diagnosis combined with rectal biopsies
- Upper endoscopy - to rule out Crohn’s
- Stool culture - to rule out infection
Treatment:
- Topical and oral aminosalicylate (mesalazine/sulfasalazine)
- First line - Add prednisolone orally
- Only if aminosalicylate is ineffective with no improvement after 4 weeks treatment
- Infliximab - only in severe UC for paediatrics
- Cyclosporin - if severe UC
- Surgery - only consider if severe.
Q.47. A 4 year old is brought to the emergency department by ambulance. His mother reports that he has been unwell with a sore throat. He is sitting on his mother’s knee and is tolerating an oxygen mask but looks unwell. He has constant noisy breathing and he is drooling saliva. He has a temperature of 39.0 C. What is the most likely diagnosis?
Correct Answer : C
The given case is a classic picture of acute epiglottitis.
The clincher here is drooling of saliva. If you find any questions with a child with drooling saliva, this is likely acute epiglottitis.
Summon the most experienced anaesthetist to intubate before obstruction occurs.
Q.48. A 2 year old boy presents to the Emergency Department with bruising and generalised petechiae that is more prominent over his legs bilaterally. The mother states that the child recovered from the flu 2 weeks ago. On examination, there was no hepatosplenomegaly, no lymph node enlargement. Platelet count is 15000/microlitre. What is the most likely diagnosis?
Correct Answer : A
This is a diagnosis of idiopathic thrombocytopenic purpura (ITP). This is a common exam topic under the haematology component.
The main clues in the case stem from ITP: previous viral infection, or in younger children previous immunization along with low platelets.
Also, the petechiae would be mainly in the legs and on occasion on the arms. Otherwise, the child feels well and is active.
Idiopathic thrombocytopenic purpura presentation:
- Follows viral infection or immunization
- The most common presentation is petechiae or bruising.
Petechiae mainly in arms and legs
- Sudden onset
- Up to a quarter present with nosebleeds
- Haematuria and gastrointestinal bleeds are less common.
- Older girls may have menorrhagia
- Otherwise, the patient is well and physical examination is normal
Laboratory diagnosis -
Isolated thrombocytopenia; blood count otherwise normal
Management:
• Prednisolone
• IV immunoglobulin
• Emergency platelet transfusion only in life-threatening haemorrhage (usually platelet less than 20 x 109/L).
Q.49. A 3 year old child is brought to the emergency department by his mother with bruises and swelling over the medial aspect of the left arm. The mother gives a history of her son falling down the stairs a few hours ago. Bruises on the child’s back and left chest are seen on examination. X-ray of the chest shows multiple callus formation in the ribs. Analgesia has been given. What is the most appropriate next step?
Correct Answer : D
A skeletal survey is a series of x-ray that are usually used in non-accidental injuries (NAI). It is performed systematically to cover the entire skeleton. Typically, this includes a bilateral anteroposterior and posteroanterior views of arms, forearms, humerus, feet, legs, femur, pelvis, spine, and skull. Once the skeletal survey has been done, then think of the child’s protection register and involve social services.
As a junior doctor, you should involve your seniors prior to checking the child’s protection register or involving social services.
The chief consideration is the treatment and protection of the child, so do not delay treatment of painful or apparently life-threatening problems, whilst awaiting an ‘expert’.
In every hospital system, there will be a designated doctor for child protection who should be available for advice. He or she will examine the child and arrange hospital admission for further investigations (e.g. skeletal survey) as necessary.
Social Services and the police may need to be involved. Children naturally sustain bruises during minor incidents as part of ‘growing up’
Bruising over the knees and shins is a normal finding in children, particularly toddlers, who are also prone to sustaining injuries to their foreheads and chin as a result of falls. As well as considering the possibility of NAI, remember that bruising may occur as part of an unusual pathological disease process (eg Henoch–Schönlein purpura, haemophilia, ITP, leukaemia, and other causes of thrombocytopenia).
The following bruises should prompt consideration of NAI:
- Bruising in unusual sites (the eg medial aspect of upper arms or thighs)
- Finger ‘imprinting’ (eg grip complexes around upper limbs or slap marks)
- Imprints or marks from other objects (eg belt, stick)
Consider NAI in the following fractures :
- Multiple fractures of different ages
- Rib and spinal fractures
- Fractures in infants who are not independently mobile
- Long bone fractures in children. There are a few rare bone diseases that may mimic NAI.
One commonly asked in exam is Osteogenesis imperfecta. They would usually give other clues such as a blue sclera, dental abnormalities, and brittle bones.
Q.50. A 3 year old boy was brougth to the GP surgery with his mother with a 4 day history of fever and a widespread rash. He was given a diagnosis of a viral exanthema, reassured and advised to take paracetamol. The following day his mother notices he has become more lethargic and unwell and was brought into the Paediatric Emergency Department. His rash continues to spread. On examination, he has cracked red lips, red sore eyes, and cervical lymphadenopathy. His temperature was 39.1 C. He was admitted for further a full septic screen, investigations and management. 2 weeks later, his skin on his fingers and toes began to peel. What is the most likely diagnosis?
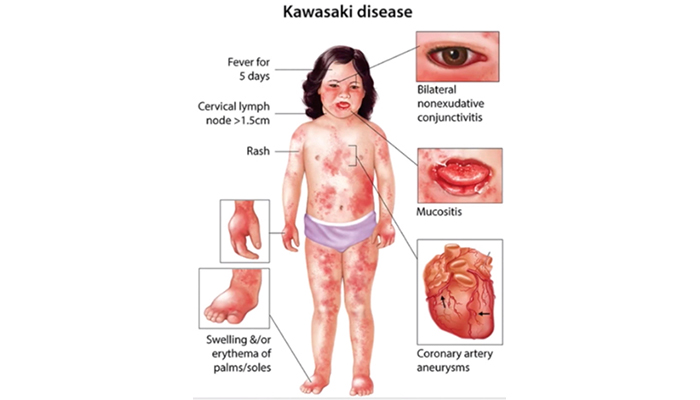
Correct Answer : C
This young boy has 5 out of 5 of the diagnostic features of Kawasaki disease with a fever above 39 C for more than 5 days. It is important to realize that in its early stages, Kawasaki disease can mimic a viral exanthem so it is often diagnosed as a viral rash and children are sent home.
Kawasaki disease and scarlet fever have many similarities such as rash, fever, strawberry tongue (which was not mentioned in the stem), and cervical lymphadenopathy however the primary complaint of scarlet fever is usually a sore throat.
KAWASAKI DISEASE is a febrile systemic vasculitis that predominantly affects children under 5 years of age. The disease is more common in Japanese children hence the Japanese name “Kawasaki” . The diagnosis is made by clinical findings alone.
Fever above 39 C for more than 5 days and at least 4 of the following features are diagnostic.
• Conjunctivitis
• Polymorphous rash
• Extremity changes: Erythema of palms and soles that later leads to desquamation
• Mucous membrane changes: Red, fissured lips, strawberry tongue
• Cervical lymphadenopathy : Prompt recognition is important as aneurysms of the coronary arteries are potentially devastating complications and treatment with immunoglobulins reduces their incidence. These coronary arteries are affected in around 30 percent of children within the first 6 weeks of illness. Hence, an echocardiogram would be an important investigation during the child’s stay in the hospital.
Bilateral, non-exudative conjunctival injection. Strawberry tongue and bright red, swollen lips with vertical cracking and bleeding. Desquamation of the fingers.
Management :
• High dose aspirin – Reduces risk of thrombosis. Once fever subsides and inflammatory markers fall, low-dose aspirin is given until an echocardiogram is performed at 6 weeks to exclude the aneurysm
• Intravenous immunoglobulin – If given within the first 10 days, reduces the risk of coronary artery aneurysms.
Q.51. A 3 year old boy has had symptoms of a viral upper respiratory tract infection for the past 3 days. His temperature recorded by his mother at home ranges from 38 C to 39 C. He has been brought to the Paediatric Accidents & Emergency with a history of a fit lasting for 3 minutes. Further clinical examinations and investigations for infection were performed in the hospital and meningitis was excluded. There is no history of febrile seizures or epilepsy in the family. At discharge, he was given the diagnosis of febrile seizures. His mother has concerns regarding the prognosis of febrile seizures and if her other children would be affected. What is the most appropriate advice to give to the mother?
Correct Answer : C
Around 30 to 40% of children with one episode of febrile seizure will continue to have another febrile seizure in the future.
Febrile seizures do have a genetic predisposition while there is a 10% risk of developing a febrile seizure if there is a first-degree relative who has suffered from febrile seizures. Around 10% of children with complex febrile seizures go on to develop epilepsy.
Q.52. Parents of a 2 month old baby are worried about cot death as their close friend recently lost their infant to sudden infant death syndrome (SIDS). She comes to you asking for advice on the best method to reduce her infant’s risk of SIDS. What is the most appropriate advice to give in regards to sleeping position and bedding?
Correct Answer : B
Cot death is more properly known as sudden infant death syndrome (SIDS). It is the term used to describe the sudden death of a child under the age of 1 year in its sleep where no cause or reason can be found. All other possible causes of death must be excluded for this diagnosis to be made. Sleeping position is particularly important.
Prone sleeping is a major, modifiable risk factor. Placing babies on their backs to sleep is advice that should be reinforced by professionals. Reassure parents that the risk of aspiration is not increased by sleeping in this position and several studies have confirmed this.
Other take home notes are:
• Soft bedding increases the risk of SIDS
• Pillows should not be used.
SUDDEN INFANT DEATH SYNDROME (SIDS) : These are some advice to give parents to decrease the risk of sudden infant death syndrome (SIDS)
• Avoid smoking near infants
• Put infants to sleep on their backs (not their front or sides)
• Avoid overheating by heavily wrapping infants
• Blankets should not be higher than their shoulders
• Infants should be placed with their feet at the foot of the cot
• Avoid bringing a baby into the bed after parents have consumed alcohol or sedative medications
• Avoid sleeping with an infant on a sofa
• Avoid using a pillow
• Use sheets and blankets rather than a duvet.
Q.53. A first time mother presents to the paediatric outpatient department with the complaint that her baby is not gaining weight. The male child is three months old and the mother claims that he has not been gaining weight for the past one month despite regular feedings. The mother says that her baby is exclusively formula fed since she cannot breastfeed due to her work during the day. The infant is taken care of during the day by his grandparents who both say that they have been feeding the baby at regular intervals with baby formula. The mother is especially concerned that her baby might have a cow’s milk allergy as the child has constant reflux. Upon examination, the baby appears irritable and cries continuously. The mother describes an uneventful pregnancy with her son being delivered via elective Cesarean section at 39 weeks of gestation. What is the most appropriate next step in management?
Correct Answer : D
There are two types of allergic reactions to cow’s milk protein: IgE-mediated reactions and non-IgE-mediated reactions.
IgE-mediated reactions -
• Occur within two hours of milk being consumed
• Symptoms include: Nausea, Vomiting, Colicky abdominal pain
• Skin manifestations include: Pruritus, Erythema, Urticaria or angioedema
Non-IgE-mediated reactions -
• Occur hours or days after ingesting milk
• Symptoms include: Reflux, Loose stools or constipation, Perianal redness, Abdominal pain, Food aversion.
• Skin manifestations include: Pruritus, Erythema, Atopic eczema, Upper and lower respiratory tract symptoms such as cough or a wheeze may be present for both IgE-mediated and non-IgE-mediated.
The best way to test for IgE-mediated reactions is to diagnose it with a skin prick test or a blood test.
The best way to diagnose non-IgE-mediated reactions is to exclude cow’s milk from the diet or to use a hypoallergenic formula such as an extensively hydrolyzed formula and see if there is an improvement in symptoms. We would normally expect improvements in symptoms in 2 weeks. If symptoms persist whilst using extensively hydrolysed formula, then swap to an amino acid formula.
Not gaining weight and reflux is seen more in non-IgE mediated reactions and thus this stem represents a classic scenario of a non-IgE mediated reaction and trying hypoallergenic formulas would be appropriate.
Key points to remember for exam purposes: If cow’s milk allergy is suspected and the reaction is acute
– Think IgE-mediated If cow’s milk allergy is suspected and the reaction is delayed (reflux, loose stools, tapering of growth)
– Think non-IgE-mediated.
Q.54. A 4 month old child is brought to Accident & Emergency by her parents. She is found to weigh 4.1 kg. She presents with multiple bruises on her left and right lower leg. Her left ankle is swollen and she refuses to move it. She appears irritable and she also has a runny nose. What is the most likely diagnosis?
Correct Answer : C
This is a probable non-accidental injury. This infant weighs 4.1kg. For a 4-month-old infant, this is beneath the normal weight gain line. A female infant of 4 months should weigh about 6.1kg and a male infant of 4 months should weigh about 6.8kg.
Another clue to the diagnosis of NAI is the multiple bruises on her lower limbs. This is the most common site of NAI in the infant population. It arises from parents or caregivers gripping and pulling the infant by the legs.
Haemophilia is incorrect because even though haemophilia is a possible diagnosis, it is improbable. Haemophilia is an X-linked recessive condition and this is a female infant.
Haemophilia CAN affect females but it is extremely rare and if they had wanted you to pick haemophilia they would have given additional clues such as neonatal bleeding following venipuncture, gastrointestinal hemorrhage, or intracranial bleeding.
Thrombocytopenia is incorrect because it usually presents following a viral infection in children. Although it presents with bruising and petechiae,
it is an improbable answer to this question because the diagnosis of thrombocytopenia lies solely in blood testing and blood smear. You cannot make a diagnosis of thrombocytopenia based on clinical signs.
Q.55. A 3 year old boy attends clinic with a history of diarrhoea on and off. The mother describes the stool as bulky, frothy and difficult to flush. He looks pale and wasted on examination. What is the most likely investigation that would lead to a diagnosis?
Correct Answer : B
The diagnosis here is coeliac disease. Bulky, frothy, and floating (difficult to flush) stools are a hint that he is having a malabsorption syndrome.
He looks pale because he is anaemic.
If you have answered A (Sweat chloride test) for cystic fibrosis. You are not completely wrong as cystic fibrosis can occur at that age as well and has symptoms of malabsorption too (foul-smelling bulky stool that "floats).
But the question writers are likely to give other hints like “repetitive cough over the last few months” if cystic fibrosis is the likely diagnosis. Also, given the two diseases, coeliac is much more common compared to cystic fibrosis, and thus the most likely investigation that would lead to a diagnosis is anti-endomysial antibodies.
Q.56. A 9 year old girl, known case of asthma, presents to the Emergency Department with a 1 day history of shortness of breath that is increasing in severity. She had a previous upper respiratory tract infection 1 week prior which had resolved. Chest x-ray reveals bilateral hyperinflation. On arrival, she was given oxygen, nebulized beta-2 agonist, and oral prednisolone. She is now drowsy, respiratory rate is 30 and her SpO2 is 90%. Which of the following is the most appropriate investigation?
Correct Answer : C
Know the step-wise management for acute asthma exacerbation in paediatric and adult medicine. Questions in exam would have a similar case stem but ask questions about investigations and treatment. Here the patient is breathless and we would need to see if she is in respiratory acidosis to determine the need for intubation/assisted ventilation.
Acute severe asthma : SpO2 <92% PEF 33–50%
- Can’t complete sentences in one breath or too breathless to talk or feed
- Heart rate >125 (>5 years) or >140 (2-5 years)
- Respiratory rate >30 breaths/min (>5 years) or >40 (2–5 years)
Life-threatening asthma : SpO2 <92% PEF <33%
- Silent chest - Cyanosis
- Poor respiratory effort
- Hypotension
- Exhaustion
- Confusion
MANAGEMENT OF ACUTE EXACERBATION IN CHILDREN :
Immediate treatment -
• Start O2 if saturations < 94%, aim sats 94-98%
• Salbutamol nebulized with O2 (pMDI + spacer if mild exacerbation)
• Add ipratropium bromide (mixed with the nebulised salbutamol solution) if refractory to initial salbutamol nebulizers
• Oral prednisolone unless vomiting, then give intravenous hydrocortisone. Remember, salbutamol and ipratropium bromide nebulizers can be repeated.
Other treatments to consider:
• Intravenous salbutamol in severe attack where the child is not responding to salbutamol nebulizers
• Intravenous aminophylline with severe attack not responding to other treatments
• Intravenous magnesium sulphate.
Q.57. A 6 year old male presents to the clinic with obesity and short stature. On examination, his BMI is > 95th percentile. His past medical history is significant for a renal transplant. What is the most likely diagnosis?
Correct Answer : B
Cushing’s syndrome is a frequent topic that overlaps in pediatrics and endocrinology for EXAM. Here it is important to make a few assumptions. The child had a renal transplant and is most likely taking corticosteroids as part of his medication regime.
Long-term steroid use would induce Cushing’s syndrome. Short stature would also result because the steroids would cause premature fusion of the growth plates.
Presentation:
The patient is taking oral steroids
- Obesity, moon face, buffalo neck hump, purple abdominal striae
- Behavioral/mood changes
- Short stature
Diagnosis: - Overnight dexamethasone suppression test or 24-hour urinary free cortisol (first line)
Treatment: - Taper the child’s steroid medication if possible or find another alternative for immunosuppression.
Q.58. A 9 year old boy is brought into the Paediatric Accidents and Emergency by his parents with severe shortness of breath. He has a history of asthma and has become unwell over the past few days with a productive cough. His symptoms are worsening and he feels the salbutamol inhalers are no longer effective in helping breathe. On examination, he has a widespread wheeze on auscultation. There are intercostal recessions and use of accessory muscles. His oxygen saturations were 88% and respiratory rate was 45 breaths/minute. Oxygen was immediately commenced. He was given back to back nebulizers with salbutamol and ipratroprium bromide. Intravenous hydrocortisone was administered. Due to poor response, he was given intravenous salbutamol and intravenous aminophylline. His symptoms continue to deteriorate with signs of exhaustions and poor respiratory effort. What is the next most appropriate medications to be considered?
Correct Answer : A
Intravenous magnesium sulphate would be the next medication to use in the severe exacerbation of asthma. At this stage, it would also be appropriate to inform the anaesthetist and paediatric intensive care unit as intubation may be required.
There is insufficient evidence to support the use of inhaled corticosteroids in acute asthma in children.
Q.59. A 6 year old boy is brought into the Paediatric Accidents and Emergency by his parents with shortness of breath. He was given the diagnosis of asthma a year ago. His symptoms have been worsening despite use of salbutamol inhalers. On examination, he has a widespread wheeze on auscultation. There are intercostal recessions seen. His oxygen saturations were 95% and respiratory rate was 40 breaths/minute. He was given back to back nebulizers with salbutamol and ipratropium bromide. What would be the next most appropriate medication to be administered?
Correct Answer : B
Oral steroids would be the next medication to administer.
This involves liquid prednisolone or crushed prednisolone tablets dissolved in water to be consumed by the child. Intravenous corticosteroids could also be given if the child was having difficulty swallowing due to his breathing or if he was vomiting however that option was not given here.
Q.60. A 4 week old female child presents with non-specific symptoms such as irritability, poor feeding, vomiting, fever of 39 C and smelly nappies. An Eschericia coli infection was confirmed on a urine culture and she responded well to antibiotics. What is the most appropriate next investigation?
Correct Answer : A
UTI presents atypically in neonates and may be associated with life-threatening sepsis. If the child is less than 6 months old like in this case and responds well to treatment within 48 hours, an ultrasound can be arranged to be done within 6 weeks. Micturating cystourethrogram (MCUG) is considered only if the ultrasound is abnormal or if the child fails to respond to antibiotics within 48 hours.
MCUG can also be performed if there is a history of recurrent UTI. A dimercaptosuccinic acid (DMSA) scan is usually performed 4 to 6 months after the acute infection. It is not needed if the child responds well to antibiotics.
REMEMBERING PAEDIATRIC UROLOGY SCANS : The key to remembering paediatric urology scans is to remember the number 6!
If younger than 6 months:
• Ultrasound during acute infection – If does NOT respond well to antibiotics within 48 hours
• Ultrasound within 6 weeks – If respond well to antibiotics
• MCUG – If did NOT respond well to antibiotics during acute infection
• DMSA scan 4-6 months – If did NOT respond well to antibiotics during acute infection.
IMAGING CHILDREN WITH URINARY TRACT INFECTIONS :
Ultrasound is the : First line test , Non-invasive, No radiation exposure, Good at determining anatomy, renal size, and presence of most congenital anomalies, Not effective at detecting mild to moderate vesicoureteric reflux.
Micturating cystourethrography (MCUG) : Gold standard test for detecting vesicoureteric reflux which affects between 25% and 40% of children with confirmed urinary tract infection.
• Requires catheterization
• Radiation exposure DMSA (dimercaptosuccinic acid) scan
• Gold standard test for detecting renal scarring or damage to renal parenchyma occurring in about 5% of children after proven urinary tract infection.
• Uses intravenous radioactive isotope which concentrates in renal tissue
• Should not be done at the time of infection as may get false positive results
• Usually done 4 to 6 months after infection
Straightforward UTI :
• Responds well to treatment within 48 hours
Atypical UTI :
• Failure to respond to treatment within 48 hours
• Septicaemia
• Raised creatinine
• Infection with non-E. coli species
• DMSA during acute infection is always the WRONG answer
• MCUG after 3 years old is always the WRONG answer.
Q.61. A 4 year old male child is brought to the GP by his mother with the complaint that he has started wetting the bed again. He had previously been dry for a period of seven months but had recently started wetting the bed again at night. This has been occurring regularly, at least once a night, for the past week now. He has no daytime symptoms. The mother describes her son’s birth as uncomplicated. The patient has an older sister who is currently seven years old. She has never wet the bed. The patient is within the 50th centile for height and weight for his age. He has no past medical history of note. A urinalysis was performed in clinic with normal results. What is the appropriate action?
Correct Answer : C
This patient has secondary enuresis. Secondary enuresis is defined as the involuntary passage of urine during sleep by a child who has previously been dry for at least six months. Enuresis can be divided into different types. Remember that enuresis is normal up to the age of 5 years.
The types of enuresis are as follows:
• Primary enuresis – Child aged 5 years or older who constantly wets the bed at night
• Primary enuresis with day time symptoms – Child aged 5 years or older who constantly wets the bed at night and who also has daytime symptoms such as urgency, frequency, or daytime wetting.
• Secondary enuresis – Child of any age who has previously been dry for at least six months and who is now wetting the bed consistently at night with or without daytime symptoms.
The most common cause of secondary enuresis is emotional upset. Other causes include urinary tract infection, constipation, or polyuria due to diabetes mellitus. It is therefore important to test the urine sample for infection and glucose. If there is no treatable UTI, then it would be reasonable to refer to a paediatrician for further investigation.
The paediatriacian would obtain a full history to look for any family problems, or developmental or learning difficulties that could account for the secondary enuresis. Remember, that one of the causes of emotional upset could be child abuse. Keep that in mind with any child who presents with secondary enuresis.
Q.62. The newborn screening results of an 8 day old female infant are as follows: TSH 40 mIU/L Total T4 32 nmol/L The mother notes that the child is difficult to feed and does not cry much. On examination, the child has cold mottled skin and weak, floppy muscles. What is the most appropriate management?
Correct Answer : B
This is a diagnosis of congenital hypothyroidism. Usually, it is found upon newborn screening. In exam, thyroid disease is a frequent topic under the endocrine component. Know how thyroid diseases present in paediatrics, especially in infants. The symptoms and signs are not always as clear-cut as adults.
The infant would usually present with difficulty in feeding, constipation, little crying, and may not be very responsive. On examination, there may be enlarged posterior fontanelles and hypotonia along with other usual hypothyroidism features i.e. decreased temperature, bradycardia, puffy appearance.
Congenital hypothyroidism :
- Difficulty feeding, constipation, little crying
- Not very responsive
- Hypotonia, dry mottled cold skin
- Prolonged neonatal jaundice.
Diagnosis:
Neonatal screening for TSH and T4 serum/plasma
The results must be interpreted according to age because TSH and T4 levels in the first weeks of life are significantly different from those in later life.
Treatment: Levothyroxine oral until 2 years of age.
Q.63. A 6 month old boy is admitted with persistent irritability. He is lethargic and is not feeding well. He has a temperature of 38.2 C, a capillary refill time of 2 seconds and a respiratory rate of 34 breaths/minute. A urinalysis reveals leukocyte esterase positive and nitrite negative. What is the investigation most likely to lead to diagnosis?
Correct Answer : C
The urine dipstick test shows leukocytes. A urine culture will be used to help confirm a urinary tract infection. Action plan for infants and children between 3 months and 3 years old with a suspected urinary tract infection:
• If both leukocyte esterase and nitrite are negative: o Antibiotic treatment is not required A urine sample for microscopy and culture is not required unless suspected to have acute pyelonephritis or serious illness
• If either leukocyte esterase or nitrite is positive: Start antibiotic treatment, Send a urine sample for a culture.
Q.64. A 1 day old male infant has developed abdominal distension, bilious vomiting and meconium ileus was present. Prenatal ultrasound had previously revealed echogenic bowel. Which of the following is the most likely diagnosis?
Correct Answer : A
This is a diagnosis of cystic fibrosis (CF).
For exam, this topic overlaps in both paediatric and adult medicine. Note that if the infant was older, then the stem would have features of “poor weight gain with foul-smelling stools” and some variation of respiratory deficit. However, this infant is a newborn, and therefore “meconium ileus” would be the most obvious clue to the diagnosis.
Features of cystic fibrosis in neonates/infants include -
• Poor weight gain
• Failure to thrive
• Meconium ileus
• Bilious vomiting
• Echogenic bowel on prenatal ultrasound.
Q.65. A 2 year old child was brought by his mother with swelling on the right side of his neck extending from the angle of the mouth to the middle one third of the sternocleidomastoid muscle. The swelling is on the anterolateral side of the sternocleidomastoid muscle. On examination, the mass is partially compressible, when subjected to light test is brilliantly translucent. What is the most likely diagnosis?
Correct Answer : B
Both lymphangioma and branchial cyst are lateral neck masses. Branchial cysts are not translucent whereas lymphangioma when subjected to light test is brilliantly translucent.
Lymphangiomas are uncommon, hamartomatous, congenital malformations of the lymphatic system that involve the skin and subcutaneous tissues. It occurs as a result of sequestration or obstruction of developing lymph vessels.
Lymphangiomas can occur anywhere in the skin and the mucous membranes. The most common sites are the head and the neck, especially in the posterior triangle of the neck. The cysts are lined by endothelium and filled with lymph. Occasionally unilocular cysts occur, but more often multiple cysts are infiltrating the surrounding structures and distorting the local anatomy.
The mass may be apparent at birth or may appear and enlarge rapidly in the early weeks or months of life as lymph accumulates; most present by age 2 years.(90% of lymphangioma occur in children less than 2 years). Lymphangiomas are soft and nontender and when subjected to light test brilliantly translucent.
Q.66. An infant soon after birth developed difficulty in breathing with intercostal recession and nasal flaring. He is afebrile. On examination, there is diminished breath sounds. On examining the mother’s notes, there was a history of spontaneous rupture of membranes 48 hours before delivery of baby. The mother was 36 weeks gestation when the baby was delivered. What is the most appropriate initial investigation?
Correct Answer : C
Infant respiratory distress syndrome secondary to surfactant deficiency which is the cause of respiratory distress. There could be potential sepsis due to prolonged rupture of membranes which worsens the respiratory distress however this is unclear.
One must remember that prolonged rupture of the membrane is not a risk factor for IRDS. The incidence of IRDS decreases with prolonged rupture of membranes.
Note, however, that PROM occurring before 37 weeks (PPROM) is one of the leading causes of preterm birth. 30-35% of all preterm births are caused by PPROM. This puts the fetus at risk for the many complications associated with prematurity such as respiratory distress.
At this stage, a chest x-ray should be done to rule out other causes of respiratory distress.
• Infant respiratory distress syndrome (IRDS) is caused by the inadequate production of surfactant in the lungs.
It is usually seen in premature infants where they have immature lungs.
• It affects approximately one-half of infants born at 28-32 weeks of gestation. It rarely occurs at term.
Risk factors:
• Premature delivery
• Infants delivered via caesarean section without maternal labour
• Maternal diabetes
Presentation :
• Respiratory distress very soon after birth: Tachypnoea, Expiratory grunting, Subcostal and intercostal retractions, Diminished breath sounds, Cyanosis, Nasal flaring.
Q.67. A 4 year old boy presents to the Emergency Department with fever, bloody diarrhoea, decreased urine output after a school field trip at a farm. On examination, the boy is pale, tired, and his face is swollen. Lab results: hematocrit 28%, platelets 72,000/microL. There is blood and protein in urine. What is the most likely diagnosis?
Correct Answer : D
For EXAM, know some of the major causes of bloody diarrhea/stool. This is a diagnosis of haemolytic uraemic syndrome. Clues: a young preschool child on an outing with family or friends and returns with bloody diarrhea. If the stem does not state specifically, assume that the child ate or was in an environment at high risk for Shiga toxin-producing E. coli.
HAEMOLYTIC URAEMIC SYNDROME :
Preschool children (< 5 years)
- TRIAD: microangiopathic haemolytic anaemia, thrombocytopenia, and acute renal failure - Bloody diarrhea, fever, abdominal pain
- Low hemoglobin and hematocrit, low platelets, hypoalbuminemia
Diagnosis: - Initial - E.coli serology, stool culture, urinalysis, full blood count
- Renal ultrasound to rule out damage
Treatment: - Hydration and electrolyte balance - +/- Nasogastric tube for nutrition intake - +/- Dialysis - Paracetamol for pain.
Q.68. A 7 day old baby whose birth weight was initially 3.5 kg, has a weight of 3.3 kg currently. What is the most appropriate next action?
Correct Answer : C
It is usual for babies to lose between five percent and 10 percent of their birth weight a few days after the birth. Note that this does not mean the child is not getting enough milk. One should not jump to the conclusion of child abuse with such minor weight loss.
Remember that in labour, very often mothers receive intravenous fluid to prevent dehydration.
This can contribute to a slightly higher birth weight for the neonate as he would have taken some fluid onboard. The fluids are lost over the next couple of hours to days which results in a reduction of weight. Following these few days of weight loss, there would be gradual weight gain. By day 14, most babies would be above their birth weight.
Q.69. A 2 year old boy presents to the Emergency Department with painless rectal bleeding for the past 2 days. On examination, the child is afebrile, tachycardic, alert, playful, and feeding well. Abdominal examination was normal. Which of the following is the most likely diagnosis?
Correct Answer : C
Meckel’s diverticulum clue (rule of 2): occurs between 2-3 years old, mostly male, approximately 2 inches long, around 2 feet away from the ileocaecal valve.
The child will usually start with painless rectal bleeding but is otherwise well. Know how to differentiate between painful and painless rectal bleeding in children for exam.
Options A to D would present with painful rectal bleeding with stool at onset.
Meckel’s diverticulum :
- Mostly asymptomatic
- Painless rectal bleeding
- If obstruction: vomiting, abdominal pain
- Age group: 2-3 years old; mostly male
Diagnosis:
Radioisotope scan - initial - Laparotomy
Treatment: - Surgical resection.
Q.70. A 14 year old boy presents to the emergency department after he fell and hit his head in the playground at school. He did not lose consciousness but has swelling and tenderness of the right cheek with a subconjunctival haemorrhage on his right eye. His observations are stable and he is alert and conscious. You are the foundation year 2 doctor who first sees him. What initial investigation would be helpful in this case?
Correct Answer : A
There is no feature of intracranial haemorrhage but the swelling and tenderness of the right cheek are likely to indicate a facial injury. While facial X-rays used to be used more frequently in the past for investigations of facial fractures, the modality of choice is now computed tomography to evaluate facial features.
However, as a foundation year doctor, it would be easy, quick, and appropriate to request a facial X-ray in this situation. It may show possible signs of a facial fracture (such as fluid level in the sinuses), however, a CT of the face would be needed to confirm the diagnosis.
Q.71. An 18 month old child is assessed for developmental milestones. He is unable to walk but is able to stand on support. He can crawl and pulls himself up to stand. He is able to transfer objects from hand to hand and is able to scribble but is unable to draw circles. He shows understanding of nouns such as “where’s mommy?” and has a vocabulary of around 4 to 6 different words but unable to form a sentence. He can wave, clap nd imitate others. What is the best development stage to describe this child?
Correct Answer : A
A child who is unable to walk by 18 months of age should be referred to a specialist community paediatric assessment. This shows a delay in gross motor development.
Q.72. A 4 month old, healthy female infant presents to clinic for her routine immunizations of DTP, Hib, polio, MenB, and pneumococcal vaccines. At her 3 month immunization, she cried and was irritable for 3 hours followed by a fever that lasted for 2 days. Which of the following is the most appropriate action now?
Correct Answer : D
For exam, usually the paediatric immunization case stem would be similar to the one above. Know the immunization schedule and the protocol for giving it.
Proceed with immunization and reassure parents that a slight fever post-vaccine is normal, and can be relieved with paracetamol. If it persists for more than 1 week then seek expert help.
Q.73. A young anxious mother of a 1 year old boy comes to you requesting a test for cystic fibrosis as her brother died from cystic fibrosis. What is the most appropriate investigation?
Correct Answer : B
Sweat testing confirms the diagnosis and is 98% sensitive. Chloride concentration > 60 mmol/L with sodium concentration lower than that of chloride on two separate occasions.
Q.74. An 8 week old baby boy is noted to be jaundiced. He has feeding difficulty, with vomiting and failure to gain weight. His stools are yellow and his urine is pale straw coloured. On palpation, the paediatrician notices an enlarged liver. What is the most likely diagnosis?
Correct Answer : C
This is a question of exclusion. Biliary atresia causes obstructive picture where stools are pale and the urine becomes dark which is NOT the case here.
Glucose-6-phosphate dehydrogenase (G6PD) deficiency like other haemolytic diseases has an onset of jaundice usually less than 24 hours Breast milk jaundice is a possibility but usually the baby is well and the jaundice usually resolves by six weeks. Occasionally it can continue for up to four months.
Congenital viral infection usually causes jaundice in the first 24 hours as well. The only possible answer is galactosaemia.
Galactosaemia : Although it is a rare inherited disease it is among the most common carbohydrate metabolism disorders.
It can be a life-threatening illness during the newborn period. Cardinal features are hepatomegaly, cataracts, and mental handicap.
Presentation :
- There is often feeding difficulty, with vomiting and failure to gain weight, with poor growth in the first few weeks of life
- Lethargy and hypotonia occur
- Jaundice and hepatomegaly develop
- Cataracts may be apparent even in the early days of life.
For the exam, pick galactosaemia when you see these symptoms in a prolonged jaundice infant:
• Poor feeding
• Vomiting
• Hepatomegaly
Management: As soon as the diagnosis is made, milk should be discontinued to remove the lactose load. This will have some immediate benefits. A galactose-free diet helps prevent the progression of liver disease.
Q.75. An 8 year old boy presents to clinic with behavioural problems. He is inattentive in class. During the interview, he is unable to sit still; he is constantly blinking his eyes, making grunting nosies with his throat and rubbing his fingers. What is the most likely diagnosis?
Correct Answer : C
This is a classic scenario for Tourette’s syndrome in exam. Other clues that may appear on exam may be the child yelling in class intermittently or shouting expletives. Most Tourette's syndromes are diagnosed at 6-8 years, maximum to the age of 13.
The other syndrome are less likely to be the answer:
Asperger syndrome: Characterized by severe persistent impairment in reciprocal social interactions, repetitive behavior patterns, and restricted interests. IQ and language are normal or, in some cases, superior.
Although tics (like the above case) can also be found in Asperger's syndrome, it is more specific for Tourette’s syndrome.
Not to mention, the question would include an impairment of social skills if the examiners wanted you to have picked Asperger syndrome.
Cotard’s syndrome is a rare mental illness in which an afflicted person holds the delusion that they are dead Rett’s syndrome There is normal development for 2–3 years, followed by a loss of acquired motor, language, and social skills between ages 3 and 4 years. Stereotypies and compulsions are common.
Ekbom’s syndrome. Also called restless leg syndrome. Unpleasant, often painful sensations in the legs, particularly on sleep onset.
Tourette’s syndrome presentation:
• Young (6-8 years old) mostly male
• Repetitive movements or gestures that are disruptive in the classroom or to people around the child (can be motor or vocal)
• Jerks, blinks, sniffs, nods, spitting, stuttering, irrepressible explosive obscene verbal ejaculations, grunts, and squeaks.
Treatment:
• Risperidone or haloperidol
• Behavioral therapy - Habit-reversal training.
Q.76. A 1 week old male infant, born at 32 weeks gestation, is currently in neonatal ICU and was doing well on increasing nasogastric feedings. The nurse now notes that the infant has been vomiting during the last 2 feedings, is less active, and has blood in his stool. On examination, the abdomen was tense, distended with decreased bowel sounds. Abdominal x-ray reveals distended loops of bowel with air in the bowel wall. What is the most appropriate next step in management?
Correct Answer : C
This is a diagnosis of necrotizing enterocolitis (NEC). This is a classic presentation and following is are the clues: abdominal distension, bloody stool, and air in the bowel wall. Note that the infant is premature although they can also be a term infant in these case stems.
According to guidelines, this infant is between Stage Ib and IIa of NEC, therefore option C is the most appropriate.
Necrotising enterocolitis presentation:
- Premature > term infant
- Vomiting (feeding intolerance), decreased activity, varying temperature
- Abdominal distension, bloody stools
- Abdominal plain film - air in the bowel wall
Diagnosis:
- Bell’s criteria/staging system
- Abdominal x-ray (supine antero-posterior; lateral decubitus)
Blood work - includes blood film, culture, coagulation, blood gas
Treatment: - Initial - stop feeds. NG tube free drainage with aspiration, antibiotics, fluids and electrolyte balance.
- Antibiotics - penicillin + gentamicin + metronidazole
- If pneumoperitoneum - surgery.
Q.77. A 12 year old boy presents with severe watery diarrhoea for the past 7 days. His urine output is low, mucous membranes are dry, and skin turgor is decreased. What is the most appropriate initial management?
Correct Answer : D
This child is dehydrated. The low urine output, dry mucous membranes, and decreased skin turgor are signs of dehydration. Fluid replacement is needed. The most common cause of gastroenteritis in children is rotavirus When assessing hydration status NICE advocates using normal, dehydrated, or shocked categories rather than the traditional normal, mild, moderate, or severe categories.
Estimating dehydration -
Clinical dehydration : Decreased urine output, Sunken eyes, Dry mucous membranes, Tachycardia, Tachypnoea, Reduced skin turgor, Clinical shock, Decreased level of consciousness, Cold extremities, Pale or mottled skin, Tachycardia, Tachypnoea, Weak peripheral pulses, Prolonged capillary refill time, Hypotension.
Management : If clinical shock admits for intravenous rehydration If just dehydrated.
Oral rehydration solution would do is unlikely to ask you to differentiate between clinical dehydration and clinical shock. However, you must be able to recognize the signs and symptoms of dehydration.
Q.78. A 3 year old boy who has had frequent urinary tract infections has recently been diagnosed with vesicouteral reflux. Which of the statements are correct?
Correct Answer : A
Antibiotic prophylaxis should be given before considering surgery. When medical management fails to prevent recurrent urinary tract infections, or if the kidneys show progressive renal scarring then surgical interventions may be necessary. Surgical corrections are generally reserved for the higher-grade refluxes (not low-grade).
The main idea of antibiotic prophylaxis is to reduce the risk of urinary tract infection and thus reduce renal scarring.
Vesicoureteral reflux - Condition where urine flows retrograde from the bladder into ureters/kidneys.
Presentation - Most children are asymptomatic - Increases risk of urinary tract infection
Thus, symptoms of a UTI: Fever, Dysuria, Frequent urination, Lower abdominal pain.
Diagnosis - Urinalysis, urine culture, and sensitivity
Initial investigation - Renal ultrasound; initial investigation might suggest the presence of VUR if ureteral dilatation is present.
Micturating cystourethrogram is gold standard - Technetium scan (DMSA) for parenchymal damage (seen as cortical scars)
Treatment - VUR grade I-IV - start with low-dose antibiotics prophylaxis daily (i.e. trimethoprim) - If the above fails and/or parenchymal damage consider surgery - reimplantation of the ureters.
Remember, the goal of treatment is to minimize infections, as it is infections that cause renal scarring and not vesicoureteral reflux. Thus, the importance of continuous antibiotic prophylaxis outweighs surgery in most cases.
Note that during early childhood, the kidneys are at higher risk of developing new scars. So it is particularly important to start parenteral antibiotic treatment for patients with vesicoureteral reflux before febrile breakthrough infections.
For patients with frequent breakthrough infections, definitive surgical or endoscopic correction is preferred.
Surgical correction should also be considered in patients with persistent high-grade reflux (grades IV/V) or abnormal renal parenchyma.
Q.79. A 3 year old male child is rushed to A&E. His mother says that he has been vomiting and having diarrhoea for the past two days. Upon examination, his dehydration status was assessed at 5% and he is unable to tolerate oral feeds. He has soiled just one diaper during the past two days. What is the best maintenance fluid regime for this child?
Correct Answer : B
This child has features of dehydration. Although normal saline can be used for initial boluses in children, it is important to remember that 0.9% sodium chloride + 5% glucose is usually used as maintenance in children (excluding neonates). This question specifically asks for a maintenance fluid regime, which should be 0.9% Normal saline + 5% Dextrose.
Q.80. You are working as a senior doctor in Accident & Emergency when you attend to a mother and a four year old boy. She complains that her child has a runny nose and sore throat which had rapidly become worse over the last three days. She also noted that he has a fever and states that the child has been refusing to eat. The mother has noticed a type of red rash which first started on her son’s face and then spread all over his body. She admits that he has missed some of his vaccinations as she had read an article online that vaccinations cause autism in children but is unsure which vaccinations were omitted and when they were originally scheduled for. There is no history of any known drug allergies in the child. The mother says that her son has recently started going to nursery school and was happy and enjoying the new environment. There is no significant history based on the patient’s past medical records. On examination, the child is alert but irritable. His temperature is 38 C and his chest is clinically clear. Examination of his throat reveals small, red spots, each with bluish-white specks in the centre. There is no cervical lymph node enlargement. On further examination of the body, there is a widespread maculopapular rash all over his body, causing discomfort and itchiness to the patient. What is the most likely treatment option for this patient?
Correct Answer : D
It is very important to remember a few critical points whenever there is a fever and a rash in a child to accurately reach a diagnosis. First, determine what type of rash is present, i.e. macular, maculopapular, vesiculaer, purpuric etc. Assess how severely ill the child is and if there are other systemic symptoms.
Q.81. A 4 year old boy is brought by his mother to the clinic as he has recently developed vesicles on his palms and soles of his feet. On examination, there are ulcers seen on the buccal mucosa. He has a temperature of 38.1 C. What is the most likely organism causing this condition?
Correct Answer : D
Hand, foot, and mouth disease is a viral illness that affects children. The lesions involve the hand, foot, and mouth. It is self-limiting. It is commonly caused by Coxsackievirus A16 (CA16) and enterovirus 71 (EV71). It is very contagious among children.
Clinical features :
• Low-grade fever
• Malaise
• Loss of appetite
• Sore throat
• Oral ulcers – may be on the buccal mucosa, tongue, or hard palate
• Followed later by vesicles on the palms and soles of the feet
• Small erythematous macules on palms and soles of the feet which progress to grey vesicles and may last for up to 6 days.
Q.82. A 2 year old child is brought to the hospital by his mother with a barking cough. A few days ago he had a runny nose, cough and a sore throat. His chest sounds are normal and there are no signs of intercostal recession. He has a temperature of 38.7 C, respiratory rate of 34 breaths/minute, pulse rate of 150 beats/minute and his oxygen saturation on air is 98%. What is the most appropriate management?
Correct Answer : A
A barking cough is a clincher that tells you this is croup. Croup is a form of upper respiratory tract infection seen in infants and toddlers with peak incidence at 6 months to 3 years. Parainfluenza viruses account for the majority of cases (more than 80% of cases). The illness usually lasts around 3 to 5 days involving features of stridor, barking cough, fever (mild temperature), and coryzal symptoms.
Giving a single dose of oral dexamethasone (0.15mg/kg) to all children regardless of severity is recommended. In this stem, it is clear that he has mild croup. Mild croup is largely self-limiting but treatment with a single dose of oral dexamethasone would be of benefit.
Emergency treatment of croup involves giving high-flow oxygen and nebulized adrenaline. In this stem, his oxygen saturation is not low and thus he will not benefit from oxygen. Nebulized adrenaline (epinephrine) is usually reserved for patients in moderate-to-severe distress which in this stem the child is not.
Q.83. A 6 year old child is brought in by her mother with complaints of having a fever and a sore throat. She developed a rash which started on her torso and had spread to her extremities. Her tongue has an appearance of a strawberry. She has a temperature of 39 C. A diagnosis of scarlet fever is suspected. What is the most likely organism causing her symptoms?
Correct Answer : C
Scarlet fever is caused by group A Streptococcus pyogenes.
Q.84. A 2 year old boy was separated from his mother in a shopping mall. He got very upset and then fell down and became unconscious. He looked blue. He became conscious after 2 minutes and was back to his active self after an hour. His mother is extremely concerned. What is the most appropriate next step?
Correct Answer : C
The diagnosis here is breath-holding spells. This usually occurs in young children when they are upset and can be precipitated by trauma or when separated from their parents.
Anything that may upset a child including injury from falling down These children stop breathing for some time, they may turn blue or have little jerks of the limbs. After some time they spontaneously start breathing. They become completely fine after an hour. Treatment is not necessary. Usually just reassure parents.
Q.85. A 7 year old child presented with chronic cough and is also found to be jaundiced on examination. What is the most likely diagnosis?
Correct Answer : B
Jaundiced is a hint towards liver dysfunction. Together with respiratory symptoms are suggestive of alpha-1 antitrypsin deficiency Alpha-antitrypsin deficiency This is an inherited condition that is associated with the early development of emphysema.
Q.86. A 4 year old boy is brought to clinic by his worried mother complaining that he is still unable to keep dry at night. He wets his bed in the middle of the night and has daytime wetting as well. There was no period where he managed to stay dry during the night. The mother wants to know if anything can be done to resolve this issue. What is the most appropriate management?
Correct Answer : A
Children older than 2 years of age with primary bedwetting and daytime symptoms can be reassured. If still persists, can refer to secondary care or enuresis clinic.
Q.87. A 7 year old girl is brought by her mother with bright red staining of her underpants. She gives a history that her daughter recently started taking horse riding lessons. What is the next most appropriate action?
Correct Answer : D
The likely diagnosis here is a perforated hymen given the history of horse riding. There is no need for general anaesthesia at this point as she is only having red staining. One must remember that general anaesthesia has its complications and should not be used without reason.
An attempt to examine the clinic without anaesthesia would be the preferred method. It is extremely important to reassure, explain the examination, and show equipment as this will help diminish the fears and anxiety of the child. Ensure the child's privacy and stop the examination at any time provided the child indicates discomfort or withdraws permission to continue. When should we consider general anaesthesia If the child refuses the examination and conditions requiring medical attention, such as bleeding or a foreign body, are suspected.
Q.88. A 4 week old male infant presents to the Accident & Emergency Department with vomiting after every feed. The mother describes the vomiting as projectile and non-bilious in nature. The child is also constipated and has not passed stool or flatus for 3 days. On examination, there is a right sided olive-sized abdominal mass on palpation. What is the most appropriate next step of action to diagnose the condition?

Correct Answer : B
Pyloric Stenosis:
Projectile non-bilious vomiting; Age group: 3-8 weeks; Olive-sized abdominal mass.
The child will feel hungry and want to feed despite constant vomiting
Diagnosis: Abdominal ultrasound
Treatment: Metabolic alkalosis – correct electrolyte imbalance + dehydration.
Then referral to paediatric surgery (pyloromyotomy) + nasogastric tube. Occasionally, the exam may show an abdominal X-ray and ask you for the diagnosis.This is typically what an abdominal X-ray of an infant with pyloric stenosis will look like.
Q.89. A 2 year old girl previously well is brought to A&E by her mother with a history of vomiting and diarrhoea for the last 2 days. She is unable to keep any food or liquid down in the past day. Her heart rate is 160 beats/minute and her respiratory rate is 30 breaths/minute. She weighs 9 kg. What is the most suitable indication for intravenous fluids administration?
Correct Answer : A
Normal capillary refill time is usually less than 2 seconds. Prolonged capillary refill time is a sign of clinical shock. Intravenous fluid should be started immediately.
A 2-year-old child can have a heart rate anywhere between 80 to 120 beats per minute so option D is wrong.
It is also normal to have a respiratory rate between 20 to 30 breaths per minute in a 2-year-old child thus option B is wrong.
Passing large amounts or increased frequency of watery stool is not a clinical sign of dehydration.
Q.90. A 28 year old woman has a delivery of a term baby girl 8 hours ago. She was admitted initially for prolonged rupture of the membranes. The neonate develops a temperature of 38.5 C and has probems breathing. What is the most likely causative organism?
Correct Answer : B
Group B streptococcus (GBS) infections are the most common cause of early-onset neonatal infection. This is supported by the given risk factor of the prolonged rupture of membranes. Group B streptococcus is the infection caused by the bacterium Streptococcus agalactiae.
Q.91. A 4 year old boy is brought to clinic by his worried mother complaining that he is still unable to keep dry at night. There was no period where he managed to stay dry during the night. The mother wants to know if anything can be done to resolve this issue. He is dry during the day. His medical history is insignificant and there is no history of recurrent urinary tract infections. What is the most appropriate management?
Correct Answer : C
Reassure the parents that many children younger than 5 years of age wet the bed, and this usually resolves without treatment.
This is defined as primary nocturnal enuresis.
Reassurance may be all that is required.
Remember the definitions
• Primary nocturnal enuresis refers to children that have never been dry for more than 6 months
• Secondary nocturnal enuresis refers to the re-emergence of bedwetting after a period of being dry for at least 6 months.
Q.92. A 5 year old girl is being investigated for renal failure. She has a history of urinary tract infections in the past. A congenital abnormalty of the insertion of ureters into the urinary bladder was seen on scan. What is the most likely cause for renal failure in this patient?
Correct Answer : D
Reflux nephropathy is a progressive lesion caused by repeated kidney infections. It is due to urine flowing backward from the bladder to the kidneys (vesicoureteral reflux). It is almost always found in childhood in the context of an abnormal urinary tract like in this stem.
Q.93. A 2 week old female infant born at term has gradually become jaundiced over the past few days. Both mother and newborn were visited at home by her midwife who decided to refer the newborn back to the paediatric team in the hospital due to prolonged jaundice. Her mother has breastfed her exclusively since she was born. Besides the symptoms of jaundice, the newborn has been growing well and has normal yellow coloured stool. A split bilirubin test was performed which shows elevated levels of unconjugated bilirubin. What is the most appropriate management?
Correct Answer : C
Breastmilk jaundice infants usually become jaundiced in the second week of life. They are usually well and the jaundice resolves within 6 weeks but may also continue up to 4 months.
Breast milk jaundice is the most common cause of prolonged unconjugated hyperbilirubinaemia.
It affects 15% of healthy breastfed infants. The diagnosis and occasional treatment is to stop breastfeeding (and give formula) for 24 hours.
When bilirubin is checked again, a significant fall would help diagnose this condition, after which the infant may then be safely breastfed. Although interrupting breastfeeding for 24 hours (and giving formula instead) is the most rapid way to reduce bilirubin levels, in the majority of infants, interrupting breastfeeding is not necessary or advisable.
The best option in this scenario would be to continue breastfeeding.
Q.94. A 6 week old male baby attends the emergency department appearing extremely unwell. Mucous membranes are dry on examination with sunken eyes and sunken fontanelles. Skin turgor was reduced. His blood tests show: Sodium 124 mmol/L Potassium 2.8 mmol/L What is the most appropriate initial management?
Correct Answer : B
In this case, the main clinical concern is the profound dehydration of the poor baby. There are multiple possible causes. The emphasis here is to ensure a safe INITIAL option as these cases will likely be cared for in the neonatal intensive care unit. The possible causes include sepsis and diabetic ketoacidosis.
Option B 0.9% sodium chloride with potassium chloride is the correct answer here as it is the safest option and addresses the potassium disturbance. At a GP doctor level this would be a safe option provided the correct protocols are followed for prescribing fluids in neonates.
Option A. 5% dextrose is incorrect as this would likely worsen the electrolyte disturbance by diluting the intravascular space from further electrolytes.
Furthermore, if there is diabetic ketoacidosis going on then extra glucose will make this much worse.
Option C. 0.45% sodium chloride is incorrect as at the level you are expected to be working, you would never be in a position to start this.
Only a senior colleague would be able to prescribe this. It may be helpful to know in principle/theory the reasons for giving this fluid in special cases.
Option D. 10% dextrose is incorrect for the same reason as option A.
7.5% sodium chloride is incorrect for the same reason as option C.
Q.95. A 9 year old boy has long arms, legs, fingers and toes. He is tall for his age and is noted to have scoliosis when examining his back. He started wearing glasses at a young age as he was not able to see distance. What is the most likely syndrome?
Correct Answer : C
Please see Q-34
Q.96. A 2 month old girl presents with jaundice and failure to thrive. She was delivered at term with a birth weight of 3 kg. The jaundice was first noticed in the first few weeks of life but her parents were not able to seek medical care. She has pale stools and dark urine. Her spleen is palable and her liver is enlarged and hard. What is the most likely diagnosis?
Correct Answer : D
Jaundice in newborns is an important topic within the paediatric section for exam. The signs and symptoms here along with prolonged jaundice are suggestive of biliary atresia.
Biliary atresia causes obstructive pictures where stools are pale and the urine becomes dark which is exactly what is seen here. Failure to thrive is a result of poor absorption of long-chain fats. The spleen becomes palpable after the 3rd or 4th week in biliary atresia.
The liver may become hard and enlarged as well. Kasai procedure (hepatoportoenterostomy) has a good chance of restoring the flow of bile to the bowel but that is only if the procedure is done early.
Late presentations like this one (e.g. more than 100 days), are unlikely to have a successful Kasai procedure due to advanced liver damage and cirrhosis. This baby would likely need a liver transplant in the first year of life.
Q.97. A week old infant presents with a 10 day history of non-bilious vomiting that has increased in frequency and forefulness. Despite feeding and looking well, the infant has lost weight. Abdominal ultrasound reveals a thickened pylorus. Which of the following is the most appropriate definitive management?
Correct Answer : A
This is a diagnosis of pyloric stenosis. Note that the clue does not always have to be “projectile vomiting”. It can also be described as “forceful” and is non-bilious. The abdominal ultrasound with a thickened pylorus or “an olive-shaped mass” on palpation are other clues. Note also the age range: the child usually would be older than 3 weeks.
Pay attention to what the question is asking in exam. Here they would like to know the definitive (gold standard) for management. If they had asked what is the most appropriate “next step” then the answer would be option C (usually appear one or the other in answers, or combined).
Pyloric stenosis :
- Projectile non-bilious vomiting
- Age group: 3-8 weeks
- Olive-sized abdominal mass
- The child will feel hungry and want to feed despite constant vomiting
Diagnosis:
- Abdominal ultrasound
Treatment:
- Metabolic alkalosis – correct electrolyte imbalance + hydration
- Then referral to paediatric surgery (pyloromyotomy) - first line + nasogastric tube.
Q.98. A 6 year old boy is brought into the Emergency Department by his mother’s boyfriend with a fever of 37.8 C of 3 days duration. On examination, there are purple spots on his lower back and brownish discoloration on his left forearm with left shoulder dislocation. The child is quiet and makes no eye contact while in conversation. What is the most appropriate action to be taken after attending his fever?
Correct Answer : D
This is a frequent paediatric topic on exam. This is a case of non-accidental injury. Since child abuse is suspected by the mother’s boyfriend, it is unsafe to let the boy remain in his care. Therefore, admit the child to ensure his safety and then refer him to social services.
Q.99. A 2 year old girl has had a temperature of 39 C, poor appetite, abdominal pain and urinary frequency for the last 3 days. What is the most appropriate action?
Correct Answer : A
The clinical features described are consistent with urinary tract infections for which a clean catch of urine is the next best action. Special arrangements may be needed for collecting a sample from a child. (Clean catch, catheter, or suprapubic aspiration are methods used that reduce the risk of contamination)
Routine investigations that are done in urinary tract infections are:
- Dipstick analysis of urine
- May treat as bacterial if there are positive results for nitrite and/or leukocytes
- Urine microscopy
- Leukocytes indicate the presence of infection
- Urine culture.
Q.100. A 15 month old male infant arrives to clinic for his measles, mumps, rubella (MMR) vaccine. On examination, he has a temperature of 38.1 C and has acute otitis media. Therer is also a family history of egg allergy. What is the most appropriate action?
Correct Answer : C
Paediatric immunization case stems would be similar to the one above. The history of a fever is the reason we should postpone the child’s MMR vaccine.
If the child had a minor illness without the fever, they could still go ahead with the vaccine.
Q.101. A 10 year old boy presents to the Emergency Department having fallen from a height of 150 cm and hit his head while playing in the playground. There was no loss of consciousness and he is currently haemodynamically stable. GCS 15/15. On examination, he is oriented with a swelling and tenderness on his left cheek. You are the doctor who first sees him. Which of the following is the most appropriate initial investigation?
Correct Answer : B
In this case, stem, the patient is showing no indication of neurological deficit and is asymptomatic. According to the revised NICE guidelines in 2014, CT and MRI are necessary.
By protocol, the child having fallen from such a height should be admitted and observed at least for 4 hours (NICE guidelines) in addition to the facial x-ray to rule out any zygoma fractures (due to swelling and tenderness in the cheek).
For exam if the child is doing well, asymptomatic, with GCS 15/15 and no changes in neurological functions within 1 hour of admission, go for the investigation with the least harm first.
Head injuries in Paediatrics :
- Child playing or in an athletic match
- Head / facial trauma
- Swelling, bruising on the face only.
Diagnosis:
- For this case stem: Facial x-ray (initial)
– If fractures are detected then do CT
- CT head (definitive)
- If on arrival scan within 1 hour if the child has GCS <14, neurological deficits according to guidelines
Treatment (for this case stem): Observation & Analgesia for pain.
Q.102. A 6 year old boy is brought to clinic by his worried mother complaining that he is still unable to keep dry at night. He wets his bed in the middle of the night at least three times a week but he is without daytime symptoms. There was no period in the past where he managed to stay dry during the night. The mother has tried a star chart and awarded the child a star when the child gets up to change the sheets. She has previously visited another GP who has discussed that adequate fluid intake is important and not to restrict fluids for the child. She would like to know if there is any other method that can be done to resolve this issue. His medical history is insignificant and there is no history of recurrent urinary tract infections. What is the most appropriate management?
Correct Answer : A
This child is 6 years old with primary bedwetting (without daytime symptoms). Treatment with an enuresis alarm (first-line treatment) in combination with positive reward systems (for example star charts) would be the most appropriate.
Remember, rewards should be given for agreed behaviours such as helping change the sheets or urinating in the toilet before bed rather than having a dry night. What the mom is doing in this stem is correct.
Q.103. A mother who delivered a term infant 8 days ago is now diagnosed with varicella zoster. Her infant is currently afebrile, feeding well, passing stool and urinating without difficulty. Which of the following is the most appropriate step in management?
Correct Answer : B
If the mother’s onset of rash is > 7 days before delivery or > 7 days post delivery, varicella zoster immunoglobulin (VZIG) and isolation is not necessary for the neonate; just observation.
Q.104. A 9 year old girl presents with arthralgia and purpura over her buttocks and extensor surfaces of the legs bilaterally. Laboratory results showed elevated IgA levels and creatinine. What is the most likely diagnosis?
Correct Answer : C
This is a diagnosis of Henoch-Schonlein Purpura (HSP). Take note of the child’s age.
EXAM will usually have their case stems present at less than 10 years of age (peak of 4-6 years). In haemolytic uraemic syndrome, the age group would be much younger 3 months to 3 years.
Also, be sure to be able to differentiate rashes for exam.
In HSP, the clue is purpura over extensor surfaces. For it to be idiopathic thrombocytopenic purpura, the case stem will provide clues to previous upper respiratory tract infection and/or low platelet count.
Henoch-Schönlein purpura (HSP) :
- Purpura (non-blanching) over buttocks and extensor surfaces
- Arthralgia (especially in the knees and ankles)
- Abdominal pain
Diagnosis:
- Mainly a clinical diagnosis
- Look for elevated ESR, IgA
- Raised creatinine; labs consistent with nephropathy
Treatment:
- Self-limiting; conservative management
- NSAIDs for arthralgic pain beware of choosing this option if case stem has impaired renal involvement!
- Corticosteroids can improve associated arthralgia and the symptoms associated with gastrointestinal dysfunction.
Q.105. A 9 month old infant is brought in by his mother to the paediatric clinic for a review as he is having worsening abdominal distention and a cough. His cough has been present for the past 3 weeks and it is associated with mild shortness of breath. On examination, there is an expiratory wheeze and inspiratory crackles. It is noted that he has a faltering growth and he now sits on below the 5th centile for weight his age. His oxygen saturation is 97%. His childhood immunisations are up to date. What is the most likely diagnosis?
Correct Answer : D
Most cystic fibrosis is picked up on the heel prick test. However, there is a minority like in this case where they present with clinical features later in infancy or even later in childhood.
They would subsequently undergo a sweat test to confirm the diagnosis. The symptoms vary from child to child, but as the condition gets worse over time, the lungs and digestive system become increasingly damaged. Abdominal distention occurs from malabsorption. Faltering growth is seen with untreated cystic fibrosis.
Once diagnosis is made and effective nutritional intake is given including enteric-coated pancreatic replacement therapy, their growth starts to pick up again.
Pneumonia is not entirely wrong as he is probably suffering from pneumonia as well. However, since cystic fibrosis often presents with recurrent and persistent bacterial chest infections and the stem gives a history of abdominal distention and suboptimal growth, cystic fibrosis would be a better pick.
Q.106. An infant born at term, started to have jaundice when he was 2 days old. He is now 9 days old and the symptoms of jaundice have improved for the past 7 days. He is breastfed and is gaining weight within normal limits. What is the most likely diagnosis?
Correct Answer : A
This is typical of physiological jaundice. It begins at 2 to 3 days old and disappears towards the end of the first week (in this case day 9) Breast milk jaundice usually presents in the first or second week of life, and can persist for as long as 12 weeks (usually up to 6 weeks) before spontaneous resolution.
It is considered to be a form of physiological jaundice. Galactosaemia and hypothyroidism usually have jaundice that lasts longer than 14 days. Prolonged jaundice is a term used for jaundice lasting longer than 14 days.
Q.107. A 2 year old child presents to A&E department with drooling, sore throat and loss of voice. He has fever with a temp of 38.9 C. His parents tell you that he has not been immunised because they are afraid of the side effects of the vaccination. What is the most appropriate immediate management?
Correct Answer : C
The clincher here is drooling of saliva. If you find any questions with a child with drooling saliva, this is likely acute epiglottitis.
Summon the most experienced anaesthetist to intubate before obstruction occurs.
Q.108. A 9 year old patient attends the outpatient department with complaints of fever, malaise, weight loss, anorexia and productive cough. Examination reveals a temperature of 39.1 C, and a pulse of 120 beats/minute. His mother says that he has a history of recurrent chest infections since young. What is the most likely causative organism?
Correct Answer : A
This is a very vague question. The stem does give some hint of a diagnosis of cystic fibrosis given the history of the recurrent chest infections. It is important to note that the diagnosis of cystic fibrosis is usually made within the first 6 months of life, however over the past decade the diagnosis of cystic fibrosis later in life has been reported with increasing frequency.
Organisms which frequently colonise CF patients:
- Staphylococcus aureus
- Pseudomonas aeruginosa
While it is a known fact that Pseudomonas infections are known as opportunistic meaning the bacteria only cause infections when a person has CF or another condition that weakens the body's immune system, it is not actually the most frequent chest infection in cystic fibrosis patients.
Pseudomonas is one of the most common bacteria found in people with CF but Staphylococcus aureus (SA) is the most prevalent organism infecting the respiratory tract of CF children, and remains the second most prevalent organism in CF adults.
Cystic fibrosis in childhood and early teenage years - Staphylococcus aureus most common - Haemophilus influenza second most common.
Cystic fibrosis in teenage years and adult life Pseudomonas aeurginosa most common.
Q.109. A previously health 2 year old girl is brought to the Emergency Deparment by her mother after having witnessed the child’s body suddenly going stiff followed by uncontrolled twitching of the arms and legs for about 5 minutes. There was frothing at the mouth and on examination now the child is drowsy. Temperature on admission was 38 C. This was a first time event. What is the next appropriate management?
Correct Answer : A
This is a diagnosis of simple febrile seizure. Under current guidelines, this is a first occurrence, therefore only option A is needed. There are no indications that there is meningitis in the stem and also the patient is currently in a postictal state (“drowsy); therefore, lumbar puncture is not appropriate at this time. If this is only a first-time event, both options D and B are not necessary unless indications point to a more serious pathology (haemorrhage, status epilepticus).
Diazepam under current guidelines is useful as a preventative measure if febrile seizures occur frequently or if the seizure has not stopped while in an Emergency.
Febrile seizures are a clinical diagnosis but other pathology must be ruled out.
Other investigative steps include:
• Blood and urine test to rule out infection
• Consider lumbar puncture for meningitis if it is highly suspicious only.
Q.110. A 9 year old has just been diagnosed with insulin dependent diabetes mellitus. He refuses to take his insulin or to stick to the dietitician’s advice. He is often sullen and withdrawn at home and his teacher complains that he has stopped associating with his friends at school. What is the most appropriate referral for this patient?
Correct Answer : C
The main debatable point in this question is if we need to send this child to a child psychologist or a psychiatrist. A psychiatrist is a person that has a medical degree and who can prescribe psychotropic medication. A psychiatrist would be involved in complicated care involing prescriptions and medication management.
Since this child is clearly in need of talk therapy to help him come to terms with his newly diagnosed and chronic disease, referring him to a psychologist is the correct choice.
Q.111. A 6 week old formula fed baby is found under the healthy child programme to be deeply jaundiced. He was born at term with a birthweight of 3.2 kg. The infant and mother were unfortunately lost to follow up by their midwife. His weight gain is poor. His stools are pale and urine colour is dark. A split bilirubin reveals increased levels of serum bilirubin of 170 micromol/L, with 150 micromol/L conjugated. What is the most likely diagnosis?
Correct Answer : C
The signs and symptoms here along with prolonged jaundice are suggestive of biliary atresia. Biliary atresia causes obstructive pictures where stools are pale and the urine becomes dark which is exactly what is seen here.
Galactosaemia may cause prolonged jaundice too but does not present as an obstructive picture with stools being pale and dark urine.
Glucose-6-phosphate dehydrogenase (G6PD) deficiency like other haemolytic diseases has an onset of jaundice usually less than 24 hours Haemolytic disease of the newborn (rhesus) and congenital viral infection usually has an early onset of jaundice and is not prolonged.
Q.112. An 18 month old female child is able to walk up steps, plays well with others in daycare, build blocks, and is able to hold crayons scribbling on paper. Her mother is concerned because despite her daughter having a vocabulary of more than 10 words, she is not able to speak in sentences nor is she able to run. What is the best management strategy?
Correct Answer : B
For the exam, it is important to memorize the important developmental milestones. The questions that come up for development are similar to the ones above. A scenario is presented where the mom is concerned and you would be told to give the best advice/management.
You must answer accordingly depending on the scenario. This child is on par with her developmental milestones. While running and speaking in sentences start at 18 months, the child has up till at 2 years old to progress to that stage. If she still cannot perform these two tasks at 3-4 years old, then we would need to re-assess.
Q.113. A 4 week old female infant presents to the Emergency Department with vomiting after every feed. The child is also constipated. On examination, there is a right sided olive-sized abdominal mass on palpation. What is the most likely diagnosis?
Correct Answer : C
This is a classic presentation of pyloric stenosis on exam. “Olive-sized abdominal mass” is a classic phrase used in describing pyloric stenosis.
Q.114. A 5 year old boy is brought by his mother to the GP surgery with a 3 day history of cough and fever. He has no medical history of relevance and his birth was uncomplicated. During the examination, a soft cardiac murmur is heard upon auscultation of his chest. The murmur can only be heard during systole and is 2/6 in intensity. It can be heard clearly when the patient is supine but disappears completely when he stands upright. What is the most likely type of murmur in this patient?
Correct Answer : D
This patient has an innocent murmur. Synonyms for an innocent murmur include functional murmur and physiologic murmur. It is a benign murmur that is inconsequential. It usually disappears as the child grows. Innocent heart murmurs are picked up between infancy and early childhood, most commonly between the ages of 3 and 8 years.
The chest wall of children is thinner and their great vessels are more angulated which results in murmurs becoming more audible. It is heard during routine check-ups or incidentally when the child presents for other issues. Acute illness, such as fever, can increase the intensity of the innocent murmur since there is an increase in blood flow.
This may well disappear when the child has recovered. They are usually 1/6 or 2/6 in intensity, rarely they are 3/6 but never louder.
There is a good mnemonic to remember for the hallmark of an innocent murmur.
It can be represented by the letter “S”
– InnoSent murmur
- ASymptomatic
- Soft-blowing murmur
- Systolic murmur
- Left Sternal edge
Q.115. You are called by the neonatal ward nurse to assess a 5-day old infant with respiratory distress. He was born at 30 weeks gestation weighing 1050 g. His antenatal ultrasound scans were unremarkable. He was intubated immediately after delivery due to poor respiratory efforts. His condition improved over the past 4 days but had suddenly worsened today. Auscultation of his chest reveals a systolic murmur best audible at the left infraclavicular area. What is the best description of the murmur?
Correct Answer : A
This infant has a ductus arteriosus that has not closed yet. The ductus arteriosus is a normal vascular connection during intrauterine life that connects the pulmonary artery to the descending aorta. It normally closes within 48 hours after birth in term babies.
In preterm infants, such as in the above stem, the ductus arteriosus may remain open which is termed patent or persistent ductus arteriosus (PDA).
The type of murmur that is heard in a PDA is known as a machinery murmur. It is the hallmark physical finding of a PDA. A machinery murmur is a continuous murmur and is best heard in systole beneath the left clavicle. The murmur continues into diastole.
Q.116. An 8 month old boy presents to the Paediatric Emergency Department with a high temperature, cough and shortness of breath. His mother is concerned as he has not been eating or drinking well for the past 24 hours. Over the past few hours, he ahs been responding less to social cues. On examination, his mucous membranes are dry and he is noted to have nasal flaring. He is seen grunting with a respiratory rate of 70 breaths/minute. His temperature is 38.9 C. Which is the most worrying clinical feature?
Correct Answer : C
Knowledge of the traffic-light system is important. Any child with fever and any of the symptoms or signs in the red column should be recognized as being at high risk. In this stem, a respiratory rate of more than 60 breaths/minute is very concerning.
Q.117. A 5 month old girl was admitted with fever and lethargy. Her mother reports poor feeding and offensive-smelling urine. A urine analysis at the time of admission showed leukocyte esterase negative and nitrites positive. The urine sample was sent for microscopy and culture and she was started on antibiotics. 2 days later, she is still febrile at 38.9 C and her symptoms have not improved. What is the most appropriate investigation?
Correct Answer : C
Micturating cystourethrogram (MCUG) should be organized as she has not responded to antibiotics within 48 hours. If MCUG is indicated, it is usually performed on the second day after prophylactic antibiotics have been given. Contrast dyes are introduced into the bladder through the urethral catheter to visualize the bladder, and urethral anatomy and detect vesicoureteral reflux. Ultrasound needs to be performed but this should be done as an urgent test rather than at 6 weeks.
A dimercaptosuccinic acid (DMSA) scan should also be requested. However, this is not done urgently and would be booked for 4 to 6 months after the acute infection. There is no value in repeating a mid-stream urine for culture and sensitivity at this stage.
Q.118. A 6-month-old child presents with fever and cough. His mother has rushed him to the emergency departmen asking for help. Examination: temp=39 C and the child is feeding poorly. What is the diagnosis?
Correct Answer : A
Bronchiolitis Management:
1. Oxygen inhalation
2. Nasogastric feeding
DON’T USE: i) bronchodilator ii) steroid iii) antibiotics routinely.
Q.119. A 16-month-old child presents with drooling, sore throat and loss of voice. He has fever with a temp of 38.2C. What is your next step towards management?
Correct Answer : C
This is a case of epiglottitis. In given case urgent intubation is needed to secure airway to prevent closure of airway. Call anesthesiologist as an expert to intubate.
Q.120. A child presents with clean wound, but he has never been immunized as his parents were worried about it. There is no contraindication to immunization, what is the best management?
Correct Answer : A
Full course of DTP
Q.121. An 11-year-old boy is being checked by the diabetic specialist nurse. His HbA1c was high and he has been skipping meals recently. He has been unhappy at school. Which member of the clinical team would you refer him to next?
Correct Answer : D
Skipping meals, unhappy at school these are psychological issues. So he should be referred to a clinical psychologist.
Q.122. A 2-year-old boy fell off his tricycle and hurt his arm. He got up to start crying, but before there was any sound, he went pale, unconscious and rigid. He recovered after 1-2 minutes but remained pale. After an hour he was back to normal. His mother says she was afraid he was going to die, and that he had a similar episode 3 months prior after falling down some steps. What investigation is indicated?
Correct Answer : D
Diagnosis is breath-holding spells. Breath-holding spells are the occurrence of episodic apnea in children, possibly associated with loss of consciousness and changes in postural tone. Breath-holding spells occur in approximately 5% of the population with equal distribution between males and females.
They are most common in children between 6 and 18 months and usually not present after 5 years of age. They are unusual before 6 months of age. A positive family history can be elicited in 25% of cases. Breath-holding spells usually occur when a young child is angry, frustrated, in pain, or afraid.
Q.123. A 5 months baby presents with recurrent vomiting. Mother noticed some of the vomitus is blood stained. Choose the most appropriate investigation?
Correct Answer : A
Probable diagnosis is infantile pyloric stenosis.
Pyloric stenosis usually affects babies between 2 and 8 weeks of age but can occur anytime from birth to 6 months. Slight hematemesis of either bright-red flecks or a coffee-ground appearance is sometimes observed. Preferred investigation is ultrasonography.
If US can not establish the diagnosis we go for a barium meal and if both are non-diagnostic we go for an endoscopy. As the question wants most likely investigation it means the definitive or gold standard investigation which is upper GI endoscopy.
Q.124. A 4 weeks girl has been diagnosed of having breast milk jaundice. She is otherwise well. What is the most appropriate management?
Correct Answer : A
If jaundice lasts past the first week of life in a breastfed baby who is otherwise healthy, the condition may be called "breast milk jaundice.” This is predominantly unconjugated hyperbilirubinaemia. The cause may be actors in a mother's milk that helps a baby absorb bilirubin from the intestine.
Q.125. A 12-year-old girl when playing in the garden accidentally stepped on a hive and was bitten several times. She has numerous wheals on her body and complains of severe itching. What is the most appropriate management?
Correct Answer : A
Intravenous antihistamines are used as an adjunct to adrenaline in the emergency treatment of anaphylaxis and angioedema. Parenteral antihistamine is not recommended in less severe allergic reactions (other than anaphylaxis).
Following are the indications of adrenaline in anaphylaxis:
1. Horseness of voice
2. Wheeze
3. Shortness of breath
4. Shock
5. Stridor
6. Swelling of the tongue and cheek
7. Facial swelling
Q.126. A term baby born to a 30 year old woman of blood group A-ve develops severe jaundice within the first 24 hours of birth. What is the most likely diagnosis?
Correct Answer : D
Rh incompatibility is a condition that occurs during pregnancy if a woman has Rh-negative blood and her baby has Rh-positive blood.
Q.127. A 4-year-old girl is found to have bounding pulse and continuous machinery murmur. What is the most probable diagnosis?
Correct Answer : D
Patent ductus arteriosus (PDA) is a medical condition in which the ductus arteriosus fails to close after birth: this allows a portion of oxygenated blood from the left heart to flow back to the lungs by flowing from the aorta, which has a higher pressure, to the pulmonary artery.
Continuous mechinary murmur is a well-known feature of PDA. Other features are bounding pulse, widened pulse pressure, increased cardiac output, differential cyanosis (cyanosis of the lower extremities but not of the upper body).
Q.128. A 12-year-old child with episodes of sudden bluish discoloration and brief loss of consciousness. Exam: clubbing, central cyanosis, systolic thrill with systolic ejection murmur in 2nd left ICS. What is the most probable diagnosis?
Correct Answer : A
OF usually does not become symptomatic at birth or early infancy and given features (central cyanosis and clubbing with the murmur of right ventricular outflow obstruction i.e. ejection systolic murmur in 2nd left ICS) are well-known features of TOF.
Tetralogy of Fallot = 1. VSD + 2. Overriding of the aorta + Right ventricular outflow tract obstruction + Right ventricular hypertrophy.
Q.129. A 4-year-old child presents with pain of spontaneous onset in his knee of 2 days duration. He has developed mild fever in the 2nd day. He can walk but has a limp. Examination: painful restriction in the right hip. What is the most probable diagnosis?
Correct Answer : B
Points in favour of diagnosis:
i) Pain in joints (knee and hip). In osteomyelitis, there is no joint pain but pain in other parts of the bone like the shaft.
ii) Fever
iii) Painful restricted movement of joint
Q.130. A 3-year-old child who looks wasted on examination has a history of diarrhea on and off. The mother describes the stool as bulky, frothy and difficult to flush. What is the investigation most likely to lead to diagnosis?
Correct Answer : B
The diagnosis is celiac disease. It is not cystic fibrosis as lung problem is most commonly seen in cystic fibrosis along with GI problems like indigestion.
Q.131. A 6-year-old patient comes with easy bruising in different places when she falls. CBC: WBC 25, Hgb 10.9, Platelets 45. Her Paul bunnel test +ve. What is the most likely diagnosis?
Correct Answer : A
Suggestive lab. Values: WBC=25 (leucocytosis), Hgb 10.9 (usually patient is not anaemic), Platelets 45 (thrombocytopenia-leading to easy bruising), Positive Paul bunnel test.
Q.132. A 5-year-old boy is referred to the hospital and seen with his father who is worried that he has been listless. He is not sure why his GP suggested he should come to the emergency department and is keen to get some tablets and go home. Examination: tired and irritable, swelling around eyes. Renal biopsy: remarkable for podocyte fusion on electron microscopy. What is the most probable diagnosis?
Correct Answer : D
Minimal change glomerulonephritis.
Podocyte fusion on electron microscopy is diagnostic of minimal change glomerulonephritis.
Q.133. A 4-year-old baby has generalized tonic-clonic seizure and fever of 39C. his mother informs you that this has happened 3-4 times before. What is the most likely diagnosis?
Correct Answer : A
Febrile convulsion. Points in favour: seizures in the presence of high fever. The same previous illness indicates seizures during fever which goes against epilepsy.
Though usually febrile convulsion doesn’t tend to recur but it can recur as well. Epilepsy has no relation to fever but is due to pathology in the brain.
Q.134. An 8 month infant presented with FTT (failure to thrive) and constipation. Examination: large tongue and history of prolonged neonatal jaundice. What is the most likely diagnosis?
Correct Answer : D
Congenital hypothyroidism (CH) is inadequate thyroid hormone production in newborn infants. It can occur because of an anatomic defect in the gland, an inborn error in thyroid metabolism, or iodine deficiency.
FTT (failure to thrive), constipation, macroglossia, and prolonged neonatal jaundice are well-known features of congenital hypothyroidism.
Q.135. A mother comes with her 15 months child. Which of the following will bother you?
Correct Answer : B
Vocabulary consists of only 2 meaningless words. At 15 months the child can clearly say 5 words and his first meaningful clear word he says at 12 months.
Q.136. A 6 weeks child is brought in with vomiting, constipation and decreased serum K+. What is the diagnosis?
Correct Answer : A
Why not duodenal atresia?
Pyloric stenosis is much more commoner than duodenal atresia; in duodenal atresia the vomitus should contain bile, which is not the case in pyloric stenosis.
Q.137. A child is brought in with high grade fever, runny nose and bark-like cough. What is the most appropriate treatment for this child?
Correct Answer : A
In epiglottitis there is no cough and a bark-like cough is diagnostic of croup. High fever, and bark-like cough in a child suggest croup which is treated with corticosteroids.
Q.138. A 5 month child can’t speak but makes sounds. She can hold things with palm, not fingers. Can’t sit independently but can hold her hand and sit when propped up against pillows. How’s the childs development?
Correct Answer : A
Normal
Q.139. An 11 month baby had an apnea event. The parents are worried that if something like this happens in the future, how they are to deal. Advise them about infant CPR. WHAT SHOULD WE DO?
Correct Answer : A
Index and middle finger compression
Q.140. A 3-year-old child has a high temperature for 4 days and he had not seen a doctor. Then mother notices rashes on buccal mucosa and some around the mouth. What is the most appropriate diagnosis?
Correct Answer : A
Measles. Rash on the buccal mucosa (koplicks spot) are characteristic of measles.
Q.141. A 6-weeks-old child presents with progressive cyanosis, poor feeding, tachypnea over the first 2 wks of life and holosystolic murmur. What is the most appropriate condition?
Correct Answer : C
Tricuspid atresia
Q.142. A baby born at 34 weeks with a heart murmur is kept in the incubator for almost 4 weeks. There is no murmur at discharge. What is the likely cause of this murmur?
Correct Answer : A
PDA (patent ductus arteriosus)
The diagnosis is PDA which is more common in premature babies.
Q.143. A 6-year-old girl who has previously been well presented with a history of tonic-clonic seizures lasting 4 minutes. Her mother brought her to the hospital and she appeared well. She is afebrile and didn’t lose consciousness during the episode of seizure. She has no neurologic deficit. What is the most appropriate investigation for her?
Correct Answer : B
Serum electrolytes.
In hypoglycemic seizures there is loss of consciousness but in the given case the girl didn’t lose consciousness. Here likely cause may be electrolyte imbalance for which serum electrolytes should be done.
Q.144. A 2-year-old child playing in the garden had a clean cut. She didn’t have any vaccinations. Also, there is no contraindication to vaccinations. Parents were worried about the vaccine side effects. What will you give?
Correct Answer : D
Give complete DPT vaccine course
Q.145. A 6-year-old girl started wetting herself up to 6 times/day. What is the most appropriate treatment?
Correct Answer : D
Behavioral training. In diurnal enuresis first behavioural training is tried and if fails pharmacotherapy is given (oxybutynin).
Q.146. What advice would you give for the parents of a child with repeated UTI?
Correct Answer : B
Prophylactic antibiotic.
For repeated UTI prophylactic antibiotic should be given.
Q.147. A child presents with eczema. She was given two creams by the GP – emollient and steroid. What advice would you give her regarding application of the cream?
Correct Answer : B
First use emollient, then steroid. Emmolient 30 minutes before steroid.
Q.148. A 1-month-old boy has been brought to the emergency department, conscious but with cool peripheries and has HR 222bpm. He has been irritable and feeding poorly for 24 hour. CXR borderline enlarged heart with clear lung fields. ECG regular narrow complex tachycardia, with difficulty identifying p wave. What is the most appropriate immediate treatment?
Correct Answer : D
Synchronized DC cardioversion.
As the patient is in probable hemodynamic instability (suggested by cool peripheries due to low BP or inadequate CO) we should go for DC cardioversion. The probable diagnosis is SVT.
Q.149. A child living with his stepfather is brought by the mother with multiple bruises, fever and fractures. What do you suspect?
Correct Answer : A
H/O living with stepfather, multiple bruises, fever and fractures are suggestive of Non accidental injury / battered baby syndrome.
Q.150. A child during operation and immediately after showed glycosuria, but later his urine sugar was normal. Choose the most probable diagnosis.
Correct Answer : B
Stress-like surgery resulted in the release of stress hormones that is cortisol in excess than normal and caused transient hyperglycemia as evidenced by glycosuria. This is a normal phenomenon and when stress is over cortisol level comes to normal and hyperglycemia and glycosuria resolve.
Q.151. A child was woken up from sleep with severe pain in the testis. Exam: tenderness on palpation and only one testis was normal in size and position. What would be your next step?
Correct Answer : C
Refer urgently to a surgeon. Probable torsion of testis. Urgent referral to a the surgeon is indicated.
Q.152. A 6-months-old boy has been brought to emergency department following an apneic episode at home. He is now completely well but his parents are anxious as his cousin died of SIDS (Sudden Infant Death Syndrome) at a similar age. The parents ask for guidance on BLS (basic life support) for a baby of his age. What is the most recommended technique for cardiac compressions?
Correct Answer : D
Index and middle fingertips of one hand
Q.153. A 3-year-old child brought to the emergency department with a swelling over the left arm. X-ray shows multiple callus formation in the ribs. Exam: bruises on childs back. What is the most appropriate next step?
Correct Answer : C
Skeletal survey is a series of x-rays which is usually used in NAI (non-accidental injury) after survey should think of child protection.
Q.154. A 17-year-old man has acute pain and earache on the right side of his face. Temperature 38.4C and has extensive pre-auricular swelling on the right, tender on palpation bilaterally. What is the most likely diagnosis?
Correct Answer : D
Mumps.
C/F: Prodromal malaise, increased temperature, painful parotid swelling, becoming bilateral in 70%.
Q.155. A 6-year-old boy is clinically obese, his BMI >95th centile. He has no other medical problems, examination is unremarkable. His mother says that she has tried everything to help him lose weight. What is the most probable diagnosis?
Correct Answer : D
Primary obesity.
People are generally considered obese when their body mass index (BMI) is over 30 kg/m2. Obesity is most commonly caused by a combination of excessive food intake, lack of physical activity, and genetic susceptibility. A few cases are caused primarily by genes, endocrine disorders, medications, or mental disorders.
Q.156. A 10-year-old boy is clinically obese and the shortest in his class. He had a renal transplant last year and his mother is worried that he is being bullied. What is the most probable diagnosis?
Correct Answer : A
Cushing’s syndrome.
Renal transplant--> immune suppression is needed-> exogenous steroid-->cushing syndrome. short stature--> if steroids are used at an early age then they cause premature fusion of growth plate/calcification.
Q.157. An 8-year-old boy has longstanding asthma. He has admitted with a severe episode and is tired and drowsy. He has not improved on oxygen, inhaled B2 agonist and IV hydrocortisone. CXR shows bilateral hyperinflation. He is too breathless to use a peakflow meter and is O2 sat <90%. What is the most appropriate investigation?
Correct Answer : A
It will point toward acidosis and indicate whether assisted ventilation is needed or not.
Q.158. A 10-year-old boy who takes regular high dose inhaled steroids for his longstanding asthma has been advised to use bronchodilators to control his acute attacks. His parents are unsure when should he use his bronchodilator. What is the most appropriate investigation?
Correct Answer : C
Peak flow rate diary.
Peak flow rate diary shows diurnal variation. This diary shows when the bronchoconstriction remains worse and guides the use of bronchodilators prior to that time.
Q.159. A 6 weeks formula fed baby boy is found at the child health surveillance to be deeply jaundiced. His weight gain is poor and his stools are pale. What is the most likely diagnosis?
Correct Answer : B
Deep jaundice at 6th week with pale stools suggests obstructive jaundice. So most likely diagnosis here is biliary atresia.
Q.160. An 18-month-old boy has been brought to the emergency department because he has been refusing to move his left arm and crying more than usual for the past 24 hours. He has recently been looked after by his mother’s new boy friend while she attended college. Assessment shows multiple bruises and a fracture of the left humerus which is put in plaster. What is the most appropriate next step?
Correct Answer : A
This is NAI (nonaccidental injury). So the a child cannot be handover to the risk again and should be admitted to protect him from further the injury done by the mother's boyfriend while serial x-rays and relevant investigations were done and asked for the child protection unit’s help.
Q.161. A 15-month-old child is due for his MMR vaccine. There is a family history of egg allergy. He is febrile with acute OM. What is the most appropriate action?
Correct Answer : A
Defer immunization for 2 wks.
Q.162. A 3-month-old baby was miserable and cried for 2hour following his 1st routine immunization with DTP, HiB and meningitis. What is the most appropriate action?
Correct Answer : D
Proceed with standard immunization schedule.
Q.163. A mother is concerned that her 18 month old son has a vocabulary of ten words but can’t form a sentence. What is the best management strategy?
Correct Answer : C
Two words joining can be done in 2yrs and inability to form a sentence in 18 months is quite normal. So the option is reassurance.
Q.164. A 9-months-old child is brought to the emergency department with an irreducible firm swelling which descended into the left groin when the child has been crying. Exam: both testicles are palpable in the scrotum. What is the most appropriate management strategy?
Correct Answer : C
If there was features of strangulation we would go for emergency herniotomy. But as only irreducible we shall proceed to elective herniotomy.
Q.165. A mother presents with her 12 month old daughter. The child has no meaningful words, is unable to sit unaided and can’t play with her toys. She doesn’t laugh and has poor interaction with her siblings. What is the best management strategy?
Correct Answer : B
At 12 month one word should be said clearly, in 8 months child can sit independently, smiles at 2 months and plays with toys since early infancy. So she needs to assess developmental milestones.
Q.166. A 6-year-old girl has had 2 short episodes of cough and wheeze over the last 12 months. These 2 acute episodes responded quickly to bronchodilator, she has no symptoms or abnormal physical signs. She has slight eczema and her mother has asthma. What is the most appropriate investigation?
Correct Answer : D
Spirometry is the preferred initial test (if available) to assess the presence and severity of airflow obstruction less effort dependent and more repeatable though less applicable in acute severe asthma.
Q.167. A 4-year-old boy is brought by his parents with complains of wetting his bed at night and whenever he gets excited. What would be the most appropriate management for this child?
Correct Answer : D
Before 5 years of age enuresis is considered normal and reassure that in most cases it resolves within 5 yrs of age without any intervention.
Q.168. A 6-weeks-old child with profuse projectile vomiting. What is the first thing you will do?
Correct Answer : D
IV fluids
Q.169. A 10-year-old boy is taken to his GP by his parents with behavioural problems. He attends a special school due to inappropriate behavior and during the interview with his parents the boy barks at infrequent episodes and shouts expletives. What is the most likely diagnosis?
Correct Answer : D
Tourette’s syndrome.
Tourete’s syndrome may have motor tics like blinking, facial grimacing, shoulder shrugging.
Other complex motor tics may be sniffing, touching objects, hopping, jumping, bending or twisting. It has vocal tics like throat clearing, sniffing, grunting or barking and more complex like coprolalia (uttering socially inappropriate words) or echolalia (repeating the word or phrase of others).
Q.170. A mother presents her 6 month old son who is vocalizing. She has noticed that he doesn’t respond to loud noises. His motor milestones are normal. What is the best management strategy?
Correct Answer : A
Arrange a hearing test.
Normal motor milestones indicate normal development but unable to respond to loud noise at 6 months may indicate deafness.
Q.171. A 4-months-old girl has severe FTT (Failure To Thrive) and increasing jaundice which was 1st noticed at 1wk of age. She has an enlarged liver and scratches on her skin. Her parents have been unable to seek medical care. What is the most likely diagnosis?
Correct Answer : A
Biliary atresia.
Increasing jaundice at this age with failure to thrive, enlarged liver and scratches (itching) indicate cholestatic jaundice occurs likely from biliary atresia.
Q.172. A child admitted with progressive muscle weakness and frequent falls. What is the most probable diagnosis?
Correct Answer : A
Duchenne’s MD
Q.173. A 4-year-old boy has a cough and arthritis followed by rash on legs which are nonblanching on glass test. No history of fever. PT 13, APTT 31, Hgb 12, WBC 6.5, Platelets 300. What’s the most likely diagnosis?
Correct Answer : C
Usually occurs below 10 years of age. The characteristic rash and lab findings match with HSP.
Q.174. A 6-year-old child presented with drooling of saliva and severe stridor. He is febrile and sick looking. X-ray Neck in extension shows a thumb sign. Choose the most likely diagnosis.
Correct Answer : D
Acute epiglottitis.
Drooling of saliva and stridor along with thumb sign in neck X-ray are features of acute epiglottitis.
Q.175. A mother presents with her 3-year-old son who has indistinct nasal speech. He snores at night and has restless sleep. He is tired by day. What is the best management strategy?
Correct Answer : C
Refer to ENT surgeon.
Probable enlarged adenoid.
Q.176. A 3-year-old boy has a sudden onset of fever, vomiting and bilateral face swelling. Few days earlier the GP saw him for bilateral parotid pain and gave analgesics. What is the most appropriate next step?
Correct Answer : D
Reassurance.
A case of mumps. Self-limiting condition.
Q.177. A 6-year-old boy has completed an induction course of chemo for ALL. He has an enlarged left scrotum. What is the most appropriate next step?
Correct Answer : C
Biopsy.
Relapse may directly involve testis and excisional biopsy is done to confirm recurrence of leukemia.
Q.178. An 8-year-old boy diagnosed with asthma is on salbutamol and beclomethasone. However, he wakes up at night due to his symptoms. What is the next appropriate management?
Correct Answer : C
LTRA
Q.179. A 2-year-old child aspirated a foreign object which was removed at the hospital. The parents are now asking how to remove it if that ever happens at home. What do you advise?
Correct Answer : C
Turn the child on his back and give thumps
Q.180. A 3-year-old child with severe diarrhea and vomiting, looks lethargic, has sunken eyes and a feeble cry. What is the choice of fluids?
Correct Answer : A
Patient has features of severe dehydration and should be resuscitated first and for resuscitation fluid of choice is 0.9% NS.
Q.181. You are on emergency department shift when a mother brings her 2 year old son to you with a 1 hour history of noisy breathing. She states that although he had mild coryza over the last week, he was improving and so they had gone to a children’s picnic with nursery friends. Another parent had found him coughing and spluttering, and ever since his breathing has remained noisy. Though he appears well in the emergency department, his current observations demonstrate a raised RR (respiratory rate) and sat=91% on air. What is the most likely diagnosis?
Correct Answer : C
Foreign body aspiration
Q.182. A 1-year-old child is brought to emergency department. He woke up in the middle of the night crying severely. What initial measure should be taken for this child?
Correct Answer : C
Analgesia
Q.183. Anxious parents ask you for resuscitation technique for their 3-year-old. What do you tell them?
Correct Answer : C
15 compression: 2 breaths with nose pinched
Q.184. A 2-year-old male patient was brought by his mother with a swelling in the right side of his neck extending from the angle of the mouth to the middle 1/3 of the sternocleidomastoid muscle. The swelling was on the anterolateral side of the sternocleidomastoid and was brilliantly transilluminant. What is the likely diagnosis?
Correct Answer : A
Both lymphangioma and branchial cyst are lateral neck masses. 90% of lymphangioma occur in children less than 2 yrs. Branchial cyst usually does not transilluminate whereas lymphangioma usually transilluminates brilliantly.
Q.185. A 2-year-old girl previously well presents with a history of vomiting and diarrhea for 4 hours. What is the most suitable indication for IV fluid administration?
Correct Answer : A
Capillary refill time > 4s is the sign of severe dehydration indicating the need for IV fluid administration.
Features of severe dehydration:
i) Abnormally sleepy or lethargic
ii) Sunken eyes
iii) Drinking poorly or not at all
iv) Reduced skin turgor > 2 seconds
v) Dry tongue and mucous membrane
vi) Absent tears
vii) Oliguria
viii) Hypotension
ix) Tachycardia
x) Prolonged capillary refill time
xi) Depressed anterior fontanelle
Q.186. A young boy presented with bilateral periorbital edema, ankle swelling and increase in body weight. What is the most likely diagnosis?
Correct Answer : B
Nephrotic syndrome
Q.187. An 8-year-old child presents with recurrent abdominal pain, occasional headaches but maintains a good appetite. Exam: normal. CBC, BUE, etc are normal. What would you do for her next?
Correct Answer : C
Recurrent abdominal pain and headaches with no abnormal finding on examination and investigation points to Abdominal Migraine.
Management is reassurance.
Q.188. Parents of a 3 months baby are worried about cot death. What advice would you give?
Correct Answer : B
Lay on the back with feet towards feet end
Q.189. A child born at 36 weeks developed difficulty in breathing with intercostal recession and nasal flaring. His temp is normal but his mother had PROM 48 hours ago. What is the most likely investigation that will lead to treatment?
Correct Answer : A
Blood culture.
In neonates investigations of pneumonia are for sepsis as pneumonia at this age is always secondary to sepsis or a part of sepsis. Probable diagnosis is Neonatal Pneumonia as there are respiratory signs and a history of PROM.
In extremes of age pneumonia or sepsis may be with normal temperature or even there may be hypothermia. Here pneumonia is a part of sepsis and the investigation is not CXR but blood culture.
Chest X-ray will give signs of lung lesions but will not lead to specific treatment. Blood culture will give the results that will lead to a particular treatment.
Q.190. A 15-year-old boy presents with recurrent breathlessness and wheeze especially after exercise. What is the most diagnostic investigation?
Correct Answer : B
Lung function test.
Assessment of severity of airflow obstruction can diagnose asthma and COPD.
Q.191. A 6-year-old child presents with edema and mild proteinuria. No hematuria. What is the most likely diagnosis?
Correct Answer : C
Minimal change GN is usually seen in young children. It presents as edema and proteinuria.
Q.192. A 12-year-old boy presented with itching in his hands. Examination: skin is dry and red. His mother is asthmatic and elder brother has hay fever. What is the most likely causative factor?
Correct Answer : C
Itchy lesion and family history of asthma and hay fever in 1st-degree relatives favours the diagnosis of eczema.
Q.193. A 4-year-old girl is taken by her mother to the emergency department and complains of feeling unwell, urinary urgency and temperature 39 C. What is the next best investigation?
Correct Answer : B
The clinical features described are consistent with urinary tract infection for which clean catch of urine is the next best investigation.
Q.194. A 2-year-old girl presents with a 4 day history of fever that started with a cough. Her RR (respiratory rate) 45 bpm, saturation 94%, temperature 38.9C, capillary refill time 1s. There are crepitations at the left base on auscultation. Urine shows negative dipstick. What is the investigation most likely to lead to diagnosis?
Correct Answer : C
The features are consistent with RTI (probable pneumonia) for which CXR is the investigation of choice.
Q.195. A 3-year-old girl presents with fever for 2 days. She is drowsy and had a seizure causing twitching of the right side of the body for 4 minutes. Her RR (respiratory rate) 30 bpm, saturation 90%, temperature 38.9C, capillary refill time 2s. Urine negative on dipstick. What is the investigation most likely to lead to diagnosis?
Correct Answer : D
It is very difficult to differentiate between encephalitis and meningitis. Encephalitis is mostly viral and Meningitis also has a viral predominance though less than encephalitis.
Because encephalitis involves infection of the brain itself, symptoms of altered brain function like confusion or decreased alertness are usually present, while in cases of meningitis the patient is initially alert and, though understandably distracted by pain and misery, still in command of their mental processes.
As CSF can not differentiate between meningitis and encephalitis we have to take the help of imaging like MRI. In herpes simplex encephalitis there is characteristic hyperintensity in the frontotemporal region. In the given case there are features of raised intracranial pressure like drowsiness and seizer so we cannot proceed for LP unless guided by CT (or MRI).
On the other hand, there is no other option that can be diagnostic of the given condition. So we have to be happy with CSF analysis as the key though at this moment we have to withhold this procedure.
Q.196. A 6-months-old boy is admitted with persistent irritability. He is lethargic and is not feeding as well as usual. His RR (respirarory rate) is 30 bpm, saturation 97%, temperature 38.0C, capillary refill time 2 seconds. Urine reveals leucocytes on dipstick. What is the investigation most likely to lead to diagnosis?
Correct Answer : D
Urine for culture and sensitivity. Dipstick test if leucocytes or nitrites is suggestive of UTI. So to confirm it we should do urine C&S.
Q.197. A 3-year-old boy presents with a 1 day history of being unwell. He appears shocked and has 3 hour old rash made up of urticarial and purpural spots. His RR (respiratory rate) is 30 bpm, saturation 94%, temperature 39.0C, capillary refill time 1 second. Urine is clean on dipstick. What is the investigation most likely to lead to diagnosis?
Correct Answer : A
Blood for C&S.
Likely diagnosis is septicemia for which Blood culture is the investigation of choice.
Q.198. A child is diagnosed with VUR. What would you tell his parents?
Correct Answer : A
Practically it is established that the majority of VUR will cure with time with prophylactic antibiotics and need no surgery! Only a minority needs surgery.
Q.199. A 2-year-old child presents with severe vomiting. Examination: mass felt in abdomen. What investigation is most appropriate?
Correct Answer : A
US
Q.200. A 7-year-old girl is brought by her mother with bright red staining of her underpants. She also gives a history that her daughter recently started taking horse riding lessons. What is the most appropriate next action?
Correct Answer : A
Local exam. If child refuses local exam then exam under GA.
Q.201. A 7 day old baby whose birth weight was 3.5kg and now is 3kg. What is the most appropriate next step?
Correct Answer : D
Continue regular child care.
In 1st week the baby loses some weight then starts to gain weight again. It is normal. So the option is to continue regular child care.
Q.202. A 6-year-old child fell on his nose 2 days ago. His parents have now brought him with difficulty in breathing. Examination: fever, nasal bones are straight. What is the most likely diagnosis?
Correct Answer : B
Septal hematoma.
Septal abscess takes a bit more time and a considerable portion of case of septal hematoma is associated with fever.
Q.203. A 12-year-old patient came to the OPD with complains of fever, malaise, weight loss, anorexia andproductive cough. Examination: temperature 39C, pulse 100bpm. His mother says that he has a history of recurrent chest infections and he is not thriving well. What is the most likely causative organism?
Correct Answer : B
In younger age - Staphylococcus and by 18 years of age, 80% of patients with classic CF (cystic fibrosis) harbor P. aeruginosa, and 3.5% harbor B. cepacia.
Q.204. A 3-year-old child brought by his mother. Examination: bruises on the buttocks. Mother also gives history of runny nose 2 weeks ago. What is the most appropriate next action?
Correct Answer : B
Henoch schonlein purpura occurs mostly in the winter months. About 50-90% of patients have a preceding upper respiratory tract infection (URTI).
There is a symmetrical, erythematous macular rash, especially on the back of the legs, buttocks , and ulnar side of the arms. Within 24 hours, the macules evolve into purpuric lesions, which may coalesce and resemble bruises.
Plasma D-dimer - This may be substantially increased. PT and aPTT - May be reduced (eg, hypoprothrombinemia).
Q.205. A 4-year-old is brought to the emergency department by ambulance. His mother reports that he has been unwell with a sore throat for 8 hours. He is sitting on his mother’s knee and is tolerating an oxygen mask but looks unwell. He has constant noisy breathing and he is drooling saliva. His temp=39C. What is the most important diagnosis?
Correct Answer : D
Epiglottitis.
Q.206. A child was brought in to emergency department by his parents for taking his granddad’s medicines. There is an extra systole in the ECG. Which drug was taken?
Correct Answer : A
Both digoxin and amitryptiline can cause extrasystole.
Q.207. A 12-month-old child with AIDS is due for his MMR vaccination. What is the most appropriate action?
Correct Answer : B
MMR is a live attenuated vaccine that should be avoided in AIDS.
*** Please note, in similar question where asked about HIV-positive children’s vaccination and the answer was to give all vaccines except BCG.
HIV positive is not in an immunodeficient state and can receive live attenuated vaccines (except BCG), whereas as a child with AIDS, he has criteria of immunodeficiency already for which all live attenuated vaccines should be avoided. Please note the two terms “HIV positive” and “with AIDS”.
Q.208. A 6 weeks baby with vomiting, irritability and palpable mass in the abdomen on feeding. Choose the most likely investigation?
Correct Answer : C
Palpable mass in the abdomen “ON FEEDING” (just after feeding the mass becomes more prominent and can be palpated more easily) is suggestive of pyloric stenosis. The US is used to diagnose this.
Q.209. A 10-year-old boy is brought to the hospital with a rash over his buttocks a/w abdominal pain and vomiting. In the emergency department, he is accompanied by his mother and stepfather. His mother had left him for the weekend with the stepfather and was called to come back from holiday as he started to have some hematuria with the rash. Social services had been notified on arrive to hospital. What is the most probably diagnosis?
Correct Answer : C
Rash over buttock, abdominal pain and vomiting, blood in urine or stool suggest HSP.
Q.210. A child distressed with fever, stridor and unable to swallow saliva. His RR 40 bpm. What is the initial step that needs to be taken?
Correct Answer : B
Probable epiglottitis. So airway should be secured.
Q.211. A 7-year-old school boy has been diagnosed with meningococcal meningitis. What is the advice for schoolmates and staff?
Correct Answer : A
Rifampicin for the whole class and family.
In contacts of meningococcal meningitis chemoprophylaxis is given with Rifampicin.
Q.212. A 6-year-old child presents with history of recurrent jaundice. Between the episodes he is totally fine. Mother gives history of jaundice being brought about by ongoing infections. What is the most likely diagnosis?
Correct Answer : B
There are some precipitating factors of hemolysis causing jaundice in patients with G6PD deficiency among which infection is a recognized one.
Q.213. A child was admitted with fever, generalized skin lesion, some of them are weeping lesions and some of them are crusted. What is the most probable diagnosis?
Correct Answer : A
Please consider the diagnosis of impetigo if specifically mention honey (or yellow or golden) coloured lesions or distribution described to be on the face and limbs predominately. Otherwise, consider chickenpox.
Q.214. A child had a patchy rash following treatment for sore throat & cervical LN enlargement. Which is the most likely antibiotic?
Correct Answer : A
Infectious mononucleosis can present with a sore throat and lymphadenothy-like tonsillitis and if treated with ampicillin leads to an eruption of patchy rashes.
Q.215. A child with a history of asthma is brought to emergency department with a cut on knee and sprained on her left wrist. Which is the best analgesic for her?
Correct Answer : A
NSAIDs including ibuprofen can precipitate asthma and Cocodamol is also advised to avoid in asthma (due to its codeine content). So paracetamol is the best option here.
Q.216. A 15-month-old baby girl presented to the emergency department with difficulty in breathing. Examination: she has intercostal recessions and a wheeze. Temperature normal. What is the most likely diagnosis?
Correct Answer : C
Asthma and bronchiolitis have similar sign symptoms. The difference is in pathology. In asthma there is bronchoconstriction but in bronchiolitis, there is oedema of the airway wall. In infants and younger children, bronchiolitis is commoner than asthma and it is seen that many of the children with bronchiolitis usually followed by asthma.
Q.217. An 8-year-old boy develops a seizure affecting his right arm, seizure lasts for several minutes. He doesn’t remember anything what happened. On his CT: lesion in left hemisphere. What is the most probable diagnosis?
Correct Answer : B
This is a complex partial seizure due to a space-occupying lesion.
Q.218. A 14-year-old boy has been diagnosed with nephrotic syndrome. 5 days later he presents with flank pain, hematuria and fluctuating urea levels. A diagnosis of renal vein thrombosis is made. What is the most likely cause for renal vein thrombosis?
Correct Answer : C
Loss of antithrombin III
Q.219. A 2-days-old baby’s mother is worried about the baby’s hearing. Mother has a history of conductive hearing loss. What is the most appropriate test?
Correct Answer : A
A BAER (brainstem auditory evoked response) test can help to diagnose hearing loss and nervous system disorders, especially in newborns, young children, and others who may not be able to participate in a standard hearing test.
Q.220. A healthy 8-year-old boy had antibiotic treatment for meningitis. Initially he wasn’t resuscitated. What will be the outcome if he receives full treatment?
Correct Answer : A
He will recover fully to his previous health.
Q.221. A mother presents with her 14-month-old child. He holds furniture and other things to help him stand and walk. He can say ‘mama’ and ‘papa’. He makes eye contact and smiles. He can transfer objects from one hand to another. He responds to his name. what do you interpret from his development?
Correct Answer : D
Normal development
Q.222. A young child, 3 year old, has presented with vomiting for 3 days. Examination: mild to moderate dehydration. What is his ABG (arterial blood gas) profile likely to show?
Correct Answer : D
pH high, PCO2 high.
Prolonged vomiting causes loss of H+, Cl-, and Na+. There is also hypokalemia. There occur metabolic alkalosis. Compensation for metabolic alkalosis occurs mainly in the lungs, which retain carbon dioxide (CO2) through slower breathing, or hypoventilation (respiratory compensation) leading to high PCO2.
Q.223. A 7-year-old girl with allergy became acutely unwell while visiting a friend’s house and has been brought immediately to the emergency department. She is fully conscious but has got stridor, wheeze and erythematous rash. She is receiving oxygen. What is the immediate management?
Correct Answer : B
Give 0.25ml in 1000U epinephrine IM.
Stridor is one of the indications of IM epinephrine in anaphylaxis.
Q.224. A child has hypothyroidism. What feature goes along with it?
Correct Answer : B
Prolonged neonatal jaundice is a well-known feature of hypothyroidism.
Q.225. A 2-weeks-old girl presents with E-coli which is confirmed by urine culture. What is the most appropriate next investigation?
Correct Answer : A
Infants and children who have had a lower urinary tract infection should undergo ultrasound (within 6 weeks) only if they are younger than 6 months or have had recurrent infections. Reference: NICE guideline (To exclude VUR which is a cause of recurrent UTI).
Q.226. A young boy presented with peri-oral blisters. Some of which are weeping and others are crusted. What is the most appropriate diagnosis?
Correct Answer : A
Impetigo.
Distribution of varicella-zoster is centripetal (more in the central area (trunk) and less in limbs and face. On the other hand, if blisters are present mainly on the face or limbs and/or described as golden, yellow, or honey-coloured crusts, are impetigo.
Q.227. A 6-weeks-old baby has a blue mark near coccyx since birth. His mother is worried. What would you do?
Correct Answer : A
Reassure.
This is a benign condition known as “Mongolian spot” or “Mongolian blue”.
Mongolian spot refers to a macular blue-gray pigmentation usually on the sacral area of healthy infants. The Mongolian spot is usually present at birth or appears within the first weeks of life. Mongolian spot typically disappears spontaneously within 4 years but can persist for life.
Q.228. A 9-year-old girl with weekly abdominal pain and occasional headaches but not along with vomiting or diarrhea. She maintains a good appetite. Laboratory findings: normal. CBC, BUE, etc are normal. Examination: no abnormality found and the abdomen was soft and non-tender. What would you do for her next?
Correct Answer : D
Reassure.
Probable case of abdominal migraine a benign condition for which reassurance is appropriate. Abdominal migraine is a form of migraine seen mainly in children. It is most common in children ages five to nine years old but can occur in adults as well.
Attacks of abdominal pain lasting 1-72 hours (untreated or unsuccessfully treated).
Q.229. A 6-weeks-old baby has been diagnosed as HIV+ve. Which immunization plan will you opt for him?
Correct Answer : D
Give all vaccines except the BCG vaccine.
There are two terms HIV +ve (not immune deficient yet) and AIDS (immune deficient state). In HIV +ve cases live attenuated vaccines can be given except BCG and if AIDS all live attenuated vaccines are avoided.
Q.230. A 2-year-old girl has had a temperature of 39C, poor appetite, abdominal pain and urinary frequency for 3 days. What is the most appropriate investigation?
Correct Answer : B
Clean catch urine specimen for culture.
Q.231. A child with T1DM who is not compliant with medicines and eats a lot. He thinks that he is short in his class. He is not happy. What would you do next?
Correct Answer : A
Not compliant with medicine, eating a lot, thinking of being short, and being unhappy are psychological issues. So he should be referred to a psychologist.
Q.232. An 8-year-old boy with a BMI of 28 was admitted to a surgical ward following a MVC (motor vehicle collision). He was found to have glycosuria. When he recovered from his injury the glycosuria resolved. What is the most appropriate follow-up investigation?
Correct Answer : A
Fasting blood glucose concentration.
The boy had glycosuria while treated in hospital following an MVC (motor vehicle collision).
It may be due to stress-related cortisol release causing hyperglycemia which later became nil as the boy recovered from trauma. But yet to be certain that he is not diabetic fasting blood glucose concentration should be done in a follow-up visit.
Q.233. At birth, a baby boy at 38 weeks GA (gestational age) weighs 1.8kgs. He has hepato-splenomegaly and a rash. Blood test show raised level of bilirubin and liver enzymes. What is the most likely diagnosis?
Correct Answer : D
Congenital infections affect the unborn fetus or newborn infant. They are generally caused by viruses that may be picked up by the baby at any time during the pregnancy up through the time of delivery.
The more common viruses linked to congenital infections include the Cytomegalovirus (CMV), Herpes, Rubella (German measles), Parvovirus, Varicella (chickenpox), and Enteroviruses.
Q.234. A 12-year-old boy with T1DM (type 1 diabetes mellitus) has poor long-term control. He is unconscious, hyperventilating and dehydrated. His blood glucose is 28mmol/l. What is the most important initial treatment?
Correct Answer : D
Probable diabetic ketoacidosis. Initial treatment is IV fluid (0.9% saline).
Q.235. A 14-year-old boy presents with recurrent abdominal pain, malaise and weight loss over 6 months. Examination: vague mass is felt in RIF. Colonoscopy shows transmural inflammation and granulomata. What is the most appropriate management?
Correct Answer : A
Drug of 1st preference is Steroids, then immunosuppressants, then amynosalicylates (such as sulfasalazine). Metronidazole is used if there is infective complications like infected perianal fistula.
Q.236. A 13-year-old boy with umbilical pain for the last 12 hours presents with anorexia, nausea and has not passed a bowel motion for 24 hours. What is your diagnosis?
Correct Answer : D
Meckel’s diverticulum.
In appendicitis pain shifts to rt iliac fossa within a few hours.
Q.237. A 10-year-old boy with lower abdominal pain for the last 10 days presents with a history of passing 6-8 loose stools. Temperature 38.8C. He is tender in the right lower quadrant and has an anal fistula. Choose the most likely cause of abdominal pain.
Correct Answer : A
Likely diagnosis is crohn’s disease which is often associated with perianal fistula formation.
Q.238. A young child diagnosed with chicken pox. Usually goes to day care. What is the most appropriate advice?
Correct Answer : C
Advice that he can go back to nursery when the rash is crusted over. At this stage patient is no more infectious.
Q.239. A 7-year-old boy is brought by his mother. There are multiple perioral and forehead vesicles. Some vesicles are crusted and some are not. The face is warm to touch. What is the most likely diagnosis?
Correct Answer : D
Distribution of varicella zoster (chickenpox) is centripetal and is mainly on the trunk. Impetigo mostly occurs centrifugally which is more on the face and limbs. Impetigo also has characteristics of yellow or honey-coloured scrub. Herpes zoster usually occurs in the elderly and is unlikely to occur in children.
Q.240. A 5-year-old boy is rescued from a burning building and is presented to the emergency departmnt. He has 5% partial thickness burns over the arms and legs and had soot in the mouth and nose. His breathing has become noisy. What is the most immediate management?
Correct Answer : D
Intubation of the airway.
Soot in the mouth and nose and noisy breathing occur in inhalation injury where intubation of the airway is indicated.
Q.241. A mother got infected with Hep B during pregnancy. Her child is born and she is worried about the risk of infection to the baby with Hep B. What would you give to the baby?
Correct Answer : B
Hep B full vaccine and Ig.
Q.242. A 9-year-old child doesn’t play with his peers and has collected 200 cars. He doesn’t respond to any criticism. What is the diagnosis?
Correct Answer : A
Autism.
Q.243. A 6-monhs-old infant has breast milk jaundice. He is otherwise feeding well and is not dehydrated. What would his LFTs look like?
Correct Answer : A
Total bilirubin:40, conjugated bilirubin<5%.
Brest milk jaundice is characterized by indirect hyperbilirubinemia.
Q.244. A child has developed rash after the treatment of penicillin. What will be the cause of rash?
Correct Answer : A
Drug reaction.
Q.245. A child comes with recurrent joint pain, multiple bruises, swollen ankle and unable to move his legs. What is the investigation of choice?
Correct Answer : C
Clotting factors.
Probable diagnosis is hemarthrosis due to hemophilia.
Q.246. A 3-year-old boy presents with difficulty in walking and skin lesions. What is the most likely causative agent?
Correct Answer : C
Parvovirus.
Sometimes there may occur arthropathy for which children have difficulty walking. There occurs macular morbilliform rash in parvovirus infection following the disappearance of a rash of the cheeks.
Q.247. A 7-year-old boy presents with his mother to GP. His mother describes he had presented this since 3 weeks ago. He had not experienced any trauma. No other symptoms along with the condition. Examination: non tender swollen ankles bilaterally. There is no rash or lesion. He is otherwise well. Which test would be the best as an initial assessment?
Correct Answer : B
Likely cause of ankle oedema from hypoalbuminema.
Q.248. A young boy presents with fever and cough. His father was diagnosed with TB a week ago. The parents don’t want him to have a BAL under anesthesia. Which other samples can be taken for diagnosis?
Correct Answer : D
A young boy can cough up sputum unless it is a dry cough where suspected TB is diagnosed by broncho-alveolar-lavage (BAL). As in dry cough, TB bacteria contaminate saliva and go to the stomach with swallowed contaminated saliva Gastric washing can bring out bacteria and detect thereby.
So gastric-washing is an alternative to BAL in dry cough.
Q.249. A 6-year-old girl is being investigated for renal failure. She is found to have a congenital abnormality of the insertion of the ureters into the urinary bladder. What is the most likely cause for renal failure in this patient?
Correct Answer : D
Reflux nephropathy is kidney damage (nephropathy) due to urine flowing backward (reflux) from the bladder toward the kidneys; the latter is called vesicoureteral reflux (VUR).
Q.250. A child came to the emergency department with severe asthma and not responding to salbutamol nebulizer and vomiting many times. What is the most appropriate management?
Correct Answer : D
In acute attack there is no place for salmeterol. In the given case most appropriate management is IV salbutamol.
Q.251. A 4-year-old child comes with a sprain in his foot. History reveals that the child has had recurrent admissions to the hospital due to severe asthma. What is the most appropriate analgesic?
Correct Answer : C
Paracetamol
Q.252. A girl presents with signs of hyperventilation. What is the most likely ABG derangement?
Correct Answer : C
pH increased, PCO2 decreased
Q.253. A 5-week-old breast fed baby whose birth weight was 3.5kg and is now 4.5kg is thriving well but is deeply jaundiced. What is the most likely diagnosis?
Correct Answer : B
Breast milk jaundice is a type of neonatal jaundice associated with breastfeeding. It is characterized by indirect hyperbilirubinemia, presents in the first or second week of life, and can persist for as long as 12 weeks before spontaneous resolution. It is normal thrive and weight gain. In galactosemia there will be lethargy, vomiting, diarrhea, and failure to thrive.
Q.254. A 4-year-old child presents with repeated chest infections. He has yellow discoloration of sclera and the mother gives a history of diarrhea as well. What is the investigation most likely to lead to a diagnosis?
Correct Answer : A
Repeated chest infections and jaundice suggest a diagnosis of cystic fibrosis. In the hepatobiliary system which is damaged in about 25 to 30% of cystic fibrosis patients, malfunctioning secretion can cause liver disease and gallstones, leading to pain and jaundice. For cystic fibrosis sweat chloride test can be done.
Q.255. A newborn that is electively intubated at birth and is due for surgery 48 hours after birth. The condition was suspected on antenatal US on CXR. What is the most likely diagnosis?
Correct Answer : B
Congenital diaphragmatic hernia
Q.256. A mother brings her newborn to the hospital concerned about a blue patch on the buttocks. The newborn is of mixed race and was delivered normally. What is the most appropriate management?
Correct Answer : A
Reassurance.
The diagnosis is Mongolian blue or spot. Mongolian spot refers to a macular blue-gray pigmentation usually on the sacral area of healthy infants.
The Mongolian spot is usually present at birth or appears within the first weeks of life. Mongolian spot typically disappears spontaneously within 4 years but can persist for life. It is a benign condition requiring no intervention.
Q.257. A child suffering from CF (cystic fibrois) developed pneumonia. Which organism is responsible for this pneumonia?
Correct Answer : C
During the first decade of life of CF patients, Staphylococcus aureus and Hemophilus influenzae are the most common bacteria isolated from the sputum, but in the second and third decade of life, Pseudomonas aeruginosa is the prevalent bacteria.
Q.258. A 5-year-old previously healthy child has a 1-day history of severe pain in the throat, breathing difficulties and fever. On examination you find an anxious, septiclooking child with drooling of saliva and stridor. Which is the most appropriate initial management?
Correct Answer : A
Intubation under general anesthesia.
Acute epiglottitis - Should intubate to save from closure of airway.
Q.259. A previously healthy, 10 months female child presents to your clinic with a 1-day history of high fever, runny nose and conjunctivitis. The child looks unwell and is irritable. Examination: child's oropharynx shows that it is inflammed and there are small white spots on the oral mucosa. Which is the most likely diagnosis?
Correct Answer : D
Koplick’s spots are characteristic of measles.
Q.260. A 3 day term, breast-fed infant is brought by the mother who reports that the child has not been active and not feeding well. She also notices jaundice, which was not present at birth and is increasing. Examination: the temperature 35.4°C, and the liver is palpable 2 cm below the costal margin. Which is the most likely diagnosis?
Correct Answer : D
Not active, not feeding well, increasing new onset jaundice and hypothermia are suggestive of neonatal sepsis.
Q.261. A 6-year-old boy presented about 4 hour ago with acute severe pain on the testis with the left half slightly higher than the right. Pain was not relieved by any strong analgesic. What is the initial management?
Correct Answer : D
Immediate surgical referral. Diagnosis is torsion of testis.
Q.262. A healthy 2-year-old boy is brought to the emergency department having cut his hand playing in the garden. He has a 2 cm clean laceration. He has not received any routine immunizations as his parents are concerned about possible side effects. There are no contraindications to immunizations. What is the most appropriate course of action?
Correct Answer : A
The child is unimmunized and has no contraindication to vaccination. Keeping in mind his age, single injections would be useless and would not help the patient. Courses on the DPT vaccine would be the best choice in this case.
Q.263. A 6 weeks child has history of frequent vomiting which became worse during the last weeks. He has no fever, recently he has passed stool only once every 2-3 days. What investigation will you do to confirm the diagnosis?
Correct Answer : A
Abdominal US.
The age and symptoms point towards pyloric stenosis.
Q.264. A healthy baby boy is born at term to a woman who was unwell with confirmed acute hepatitis B during pregnancy. The mother is very concerned that she may have infected the baby with hepatitis B. What preventative intervention should be given to the baby?
Correct Answer : C
Hepatitis B vaccine and hepatitis B immunoglobulin.
Babies born to mothers infected with hepatitis B have a high risk of acquiring infection, which can be prevented by vaccination at birth. All babies with seropositive mothers should have the full primary course of hepatitis B immunization and should also have HBIG within 24 hours of birth.
Q.265. A 4-year-old girl has had a temperature 38.5C for 2 days and has not wanted to eat her food. Yesterday she developed a sore throat and small, painful ulcers inside her mouth. Today she has small blisters on the palms of her hands and soles of her feet which are painful but not itchy. What is the most likely underlying cause?
Correct Answer : A
Coxsackie virus The patient is suffering from HFMD (Hand, Foot and Mouth Disease) • HFMD is due to an infection that usually causes a typical illness, including a typical rash. It is most commonly caused by the Coxsackie A16 virus;
• HFMD most commonly affects children under 10 years of age
• This might include a high temperature (fever). After this, a sore throat commonly occurs, quickly followed by small spots that develop inside the mouth. These soon progress into small mouth ulcers
• In many cases, spots also develop on the skin. This is typically a day or so after the mouth ulcers develop. The spots are small lumps that are a few millimeters in diameter and usually appear on the hands and feet, they are not usually itchy but sometimes they can be a little bit sore.
Treatment: No treatment will take away the virus.
Q.266. An 8-year-old girl is complying with her asthma treatment of low-dose inhaled corticosteroid prophylaxis and short-acting bronchodilators as required. Her inhaler technique is good. She now has a frequent night cough and mild exercise-induced wheeze. What would be the most appropriate change in her treatment?
Correct Answer : A
Add leukotriene antagonist. According to latest guideline.
Q.267. A 4-year-old boy complains of pain around his right eye. He is unwell, febrile and also suffers from pain on the right side of his face. What is the most probable diagnosis?
Correct Answer : D
Periobital cellulitis
Q.268. An infant is being examined as part of a routine examination. The child can hold its head up and lifts its chest off a table. He has a palmer and rooting reflex as well as a social smile. He is not afraid of strangers. What is the most likely age of this child?
Correct Answer : C
At 6 months:
1. Gross motor skill- sits briefly without support; rolls from back to tummy.
2. Fine motor skill- passes a toy from one hand to another: bangs the toy on the table.
3. Self-help skill- holds own bottle or cup during feedings.
4. Cognitive skill- reaches for a toy out of reach; likes to be with people.
5. Speech skill- begin to pronounce consonants like "ba," "da," and "ga". Starts to babble ("baba baba"). Begins to recognize his or her name. Understands a few words, such as "bath". Uses his or her voice to get attention and express feelings.
Q.269. A mother is concerned because her 1m boy has a swelling in his scrotum. He was born prematurely. On examination the swelling is seen to transilluminate. The likely cause is?
Correct Answer : C
Transilluminating scrotal swelling is likely a case of hydrocele. 1- 2% neonates present with congenital hydrocele which disappears by 1-2 years.
Q.270. A 2-month-old girl has an ante-natal diagnosis of right hydronephrosis. Postnatal serial US exams revealed increasing dilatation of the right pelvicalyceal system. No reflux was demonstrated on a MUCG. Appropriate management should include?
Correct Answer : C
Antenatal hydronephrosis and increasing postnatal hydronephrosis in the US should go for Diuresis renography for evaluation of possible pyeloplasty.
Q.271. A mother brings her 1-year-old infant to her pediatrician. She describes that following a common cold her child's voice has become hoarse and has developed a cough that sounds harsh and brassy and was worse at night. Examination: the child was noted to have trouble drawing air into its lungs between coughs and had trouble drawing air into its lungs. There was visible stridor on inhalation. The cause is most likely to be?
Correct Answer : C
Parainfluenza virus causes croup. A rough barking cough with hoarseness and wheezing, labored breathing, runny nose, fever, cough, and decreased appetitie are common features.
Q.272. An infant has diarrhea for 3 days with weight loss from 10 kg to 9 kg. Examination: he is noted to have dry mucous membranes, poor skin turgor, markedly decreased urine output, and tachycardia. His BP=normal and compression-release of the nail beds shows satisfactory refilling. Appropriate treatment would include?
Correct Answer : C
Severe dehydration. Treatment is rehydration. For severe dehydration initially fluid bolus is given with either 0.9% normal saline or Lactated Ringers injection in IV route.
Q.273. An 18-month-old girl who has had single UTI is seen in the OPD. She has fever and vomiting but these improved with course of trimethoprim. Subsequently, MCUG showed bilateral vesicoureteric reflux. Single most appropriate management?
Correct Answer : D
Ureteric surgery.
Q.274. A 4-year-old baby has a generalized tonic-clonic convulsions and fever of 39C. His mother informs you that this has happened 3-4 times ebfore. What is the most probable diagnosis?
Correct Answer : A
Febrile convulsion
Q.275. A 4-year-old girl who has had a runny nose for 12 hours has woken up 2’oclock in the morning with difficulty in breathing, a barking cough. What is the most likely diagnosis?
Correct Answer : D
Age, runny nose, dyspnea, and barking cough are suggestive features of croup.
Q.276. A 5-year-old girl who suffered from extensive burns has returned to the general ward after 2 weeks in the intensive care unit (ICU). She has a large hematemesis. Full blood count and coagulation screen are normal. What is the next invstigation?
Correct Answer : C
Barium's study of the upper GI tract. In curling ulcer barium study is preferred as endoscopy has the risk to cause perforation.
Q.277. A 2-week-old boy born with cesarean section because of placental abruption vomits altered blood. He is well hydrated and systemically well. What is the next investigation of choice?
Correct Answer : D
Discriminate between fetal and maternal blood cells (APT test).
The alkali denaturation test, also known as Apt–Downey test or Apt test, is a medical test used to differentiate fetal or neonatal blood from maternal blood found in a newborn's stool or vomitus.
Q.278. A 4-year-old presents with petechiae after a diarrheal illness and is found to have thrombocytopenia and hypertension. His stool studies are positive for E. coli 0157: H7. Which of these lab results would be expected?
Correct Answer : A
This child has hemolytic uremic syndrome (HUS) secondary to enterotoxic E. coli. Children will present with abdominal pain and fever. HUS is characterized by the triad of microangiopathic hemolytic anemia, thrombocytopenia, and acute renal failure. Given this patient's hypertension, it is likely he has laboratory evidence of acute renal injury as seen with an elevated creatinine. HUS leads to intravascular hemolysis; therefore, the red blood count is expected to be low and RBC fragments (schistocytes) are often seen on a blood smear. The hemolysis often leads to low haptoglobin as it is bound with hemoglobin from hemolyzed cells and an elevated LDH due to the cell lysis. The direct Coombs test, however, would be negative as patients with HUS do not have an antibodymediated hemolysis.
Q.279. A 11-year-old boy is brought to the doctor with left knee pain. The pain worsens with activity and improves with rest. He denies any history of trauma. Which of the following is the most likely diagnosis?
Correct Answer : B
1. Inflammation of the insertion of the patellar tendon in the tibial tubercle (tibial tubercle apophysitis).
2. It is more common in adolescent boys active in sports.
3. OSD is characterized by pain and swelling at the tibial tubercle, the point of insertion of the patellar tendon.
4. OSD generally occurs in children 9 to 14 years of age who have undergone a rapid growth spurt. It I bilateral in 25 to 50 percent of cases, although the involvement is typically asymmetric.
5. OSD occurs most frequently in participants of sports that involve running, cutting, and jumping (eg, soccer, football, basketball, volleyball, gymnastics, figure skating, ballet).
6. OSD disease is an overuse injury caused by repetitive strain and chronic avulsion of the secondary ossiffication center (apophysis) of the tibial tubercle.
7. The most common presenting complaint is anterior knee pain that increases gradually over time, from a low-grade ache to pain that causes a limp and/or impairs activity. Pain is exacerbated by direct trauma, kneeling, running, jumping, squatting, climbing stairs, or walking uphill, and is relieved by rest.
Q.280. Which of the following options presents the ECG feature of a patient with an Ostium secundum atrial septal defect?
Correct Answer : D
An ECG demonstrates sinus rhythm, often with evidence of right atrial enlargement manifested by tall, peaked P waves (usually best seen in leads II and V2) and prolongation of the PR interval. The QRS axis is slightly directed to the right (+100°), and the precordial leads reveal right ventricular enlargement of the so-called volume overload type that is characterized by an rSR' pattern in leads V3 R and V1 with normal T waves. The QRS duration may be mildly prolonged because of right ventricular dilation. This mimics the finding in right ventricular conduction delay. A significant proportion (20-40%) of children with secundum atrial septal defect may not have abnormal ECG findings.
Uncommonly, a patient with a secundum atrial septal defect may demonstrate a superior QRS axis with right ventricular enlargement, mimicking findings observed in the ECG of a patient with an ostium primum atrial septal defect.
Q.281. Pediatric patient has symptoms of epiglottitis with stridor and distress. What's your next step?
Correct Answer : A
Epiglottitis is associated with fever, difficulty in swallowing, drooling, hoarseness of voice, and typically stridor. Stridor is a sign of upper airways obstruction and is a surgical emergency. The child often appears acutely ill, anxious, and has very quiet shallow breathing with the head held forward, insisting on sitting up in bed. The early symptoms are insidious but rapidly progressive, and swelling of the throat may lead to cyanosis and asphyxiation. Epiglottitis may require urgent tracheal intubation to protect the airway, though this is not always the case. Tracheal intubation can be difficult due to distorted anatomy and profuse secretions. Spontaneous respiration is ideally maintained until tracheal intubation is successful. A surgical airway opening (cricothyrotomy) may be required if intubation is not possible.
Q.282. A 12-year-old girl presents with lack of pubertal development, short stature, and broad chest. What are the appropriate next steps in evaluating this patient?
Correct Answer : A
The features presented here most likely represent those of Turner syndrome, or monosomy X. Approximately 25-30% of patients have associated congenital heart disease, predominately left-side obstructive lesions.
Coarctation of the aorta is present in 10-20% of patients; therefore, screening for coarctation is indicated at 5-year intervals. Unlike hypoplastic aortic arches, major intracardiac anomalies are not commonly found with isolated coarctation of the aorta; however, there is a high association of this lesion with Turner syndrome and with bicuspid aortic valve. Genetic testing of the genes involved in Noonan syndrome would not be indicated unless Turner is ruled out. There can be overlap of the features between Noonan and Turner. Genetic testing for Alagille syndrome is not indicated. While an MRIof the heart may be a more sensitive way to detect subtle coartcation, it is not indicated as the first-line test.
Q.283. A 10-year-old male presents to the emergency department with a large, erythematous targetoid lesion on his arm after returning from a family trip in Connecticut. You suspect Lyme disease. What is the first-line treatment for Lyme disease?
Correct Answer : B
Doxycycline is the drug of choice for treatment of early, localized Lyme disease in children 8 years of age and older. Treatment duration is for 14 days. For children under 8 years of age, amoxicillin is recommended. Precautions with doxycycline include avoidance of exposure to the sun (eg, the use of sunscreen) because a rash develops in sun- exposed areas in about 20% of persons on the drug. Treatment in early stages of Lyme, when only erythema migrans is present but systemic symptoms are lacking, almost always prevents later stages from occurring.
Q.284. A child is observed to walk a distance of 10 feet and climb stairs. Although he cannot yet form full sentences, the child can speak a few words. The age of this child is most likely :
Correct Answer : B
Age 12 to 18 Months Gross Motor Skills (view handouts) can get to standing position alone creeps up stairs can scoop and recover an object by 15 months, walks well alone walking, pulls a pull-toy seats self on chair Language Development (view handouts) has 10-15 words will point to one body part will point to at least one picture uses jargon, i.e., unintelligible "foreign" language with inflection imitates some words follows simple directions accompanied by gestures answers simple questions nonverbally points to objects, pictures, and family members makes animal sounds such as "moo."
Q.285. A patient with diagnosis of rhinosinusitis has presented to you again for his symptoms. Which of the following is most sensitive test for maxillary sinus?
Correct Answer : B
Rhinosinusitis is typically divided among four subtypes: acute, recurrent acute, subacute, and chronic, based on patient history and a limited physical examination. In most cases, therapy is administered based on this classification.
Antibiotic therapy along with hydration and decongestants is indicated for 7 to 14 days in patients with acute, recurrent acute, or subacute bacterial rhinosinusitis. For patients with chronic disease, the same treatment regimen is indicated for an additional 4 weeks or more, and a nasal steroid may also be prescribed if inhalant allergies are suspected as an etiologic agent. Nasal endoscopy and computed tomography of the sinuses are reserved for circumstances that include a failure to respond to therapy as expected, spread of infection outside the sinuses, a question of diagnosis, and when surgery is being considered. Laboratory tests are rarely needed and are reserved for patients with suspected allergies, cystic fibrosis, immune deficiencies, mucociliary disorders, and similar disease states. X ray is best initial test. CT is most accurate test.
Choose a Question
×Choose a Question
×
Trial Access Limit Reached
You’ve reached the limit of free content. Subscribe to continue learning without restrictions.