

Hello,
Dr. Batman
Hello Doctor, Welcome!
Profile

Name: Batman
Email: batman@gotham.com
PHARMACOLOGY
(Total Questions - 69)Q.1. A 68 year old male patient is on Ramipril 10 mg daily and Bendroflumethiazide 2.5 mg daily for hypertension. He has come for his routine checkup with a blood pressure of 135/85 mmHg. His blood tests show: Serum potassium level 5.9 mmol/L Serum sodium 126 mmol/L Serum creatinine 79 micromol/L. What is the most likely side effect of thiazide diuretics which contributed to his blood results?
Correct Answer : A
One of the many known adverse effects of thiazides is postural hypotension.
Common adverse effects of thiazides worth remembering include:
• Postural hypotension
• Hyponatraemia, hypokalaemia
• gout.
THIAZIDE DIURETICS, LOOP DIURETICS, POTASSIUM-SPARING DIURETICS COMPARISON Important key points:
• Thiazide and Loop diuretics – Hyponatraemia, hypokalaemia and also gout
• Thiazide diuretics – Postural hypotension
• Spironolactone – Hyponatraemia, hyperkalaemia Thiazide diuretics The main use of bendroflumethiazide was in the management of hypertension but recent NICE guidelines now recommend other thiazide-like diuretics Commonly asked side effects include
• Postural hypotension
• Hyponatraemia
• Hypokalaemia
• Gout
• Impaired glucose tolerance Loop diuretics Example: Furosemide – Used especially in heart failure Commonly asked side effects include
• Hyponatremia
• Hypokalaemia
• Gout Potassium-sparing diuretics
Example: Spironolactone Commonly asked side effects include
• Hyperkalaemia
•Hyponatraemia
• Gynaecomastia.
Q.2. A 55 year old man on anti-hypertensives develops hyperkalaemia. What is the most likely anti-hypertensive drug to cause it?
Correct Answer : B
ACE inhibitors can cause hyperkalaemia.
Concomitant treatment with NSAIDs increases the risk of renal damage, and potassium-sparing diuretics increase the risk of hyperkalaemia.
It would be a good idea to recognize common ACE inhibitors – Ramipril, Enalapril, Captopril, Perindopril, and Lisinopril.
If there is no option for ACE inhibitors,
then angiotensin-II receptor blockers (ARBs) would be the next best option as these can too cause hyperkalaemia.
Common ARBs to know are Losartan, Candesartan and Valsartan.
Q.3. A 10 month old child who weighs 10 kilograms has been diagnosed with a urinary tract infection. He has been prescribed trimethoprim at a dose of 4 mg/kg to be given twice daily. The preparation of trimethoprim is 50 mg/5 ml. What dose will you advise the parents to give to the child?
Correct Answer : C
This question requires a sound understanding of mathematics and not medicine. The prescribed dose is 4 mg/kg body weight. The child weighs 10 kilograms, therefore the dose needed will be 40 mg.A preparation of 50 mg/5 ml is equivalent to 10 mg per mL.
Therefore, 40 mg is equivalent to 4 ml. It has to be given twice daily so 4 ml BD is the correct answer.
Q.4. Which of the following drugs can cause bronchoconstriction?
Correct Answer : D
Atenolol is a beta-blocker.
Beta-blockers are known to cause bronchoconstriction. Salbutamol and salmeterol are beta agonists.
They are used to treat bronchospasm thus they have bronchodilating effects.
Ipratropium bromide inhibits bronchoconstriction Theophylline also relaxes the bronchial smooth muscle causing bronchodilation.
Q.5. A 56 year old man whose pain was relieved by oral Morphine, now presents with progressively worsening pain. Increasing the dose of oral morphine helps to relieve his pain. However, he now complains that the increased morphine makes him drowsy and he is unable to carry out his daily activities. What is the most appropriate next step?
Correct Answer : C
In general, oxycodone should be used when patients are still in pain but have side effects of opioids. This is because oxycodone has twice the potency of morphine to manage pain but with fewer side effects compared to morphine. The pain ladder consists of 3 steps:
1: Simple analgesia like paracetamol. Aspirin, NSAIDs +/- adjuvant therapy
2: Weak opiates: e.g codeine, tramadol, dihydrocodeine +/- adjuvant therapy
3. Strong opiates: morphine, fentanyl patches, diamorphine, oxycodone +/- adjuvant therapy.
If the patient is still in pain, you should never go back a step on the pain ladder, only go forward.
Q.6. A 74 year old woman with breast cancer and bone metastasis has her pain relieved with oral morphine 60 mg twice a day. For the past 2 weeks she has needed to use an additional 20 mg of oral morphine every 4 hours. What is the most appropriate regimen of analgesia to prescribe?
Correct Answer : D
It is particularly important to remember how to calculate breakthrough doses in palliative care for pain relief. If someone is taking PRN morphine regularly for a while, they should have their pain relief reassessed and increased. In this stem, we all can agree that the regular oral morphine dose needs to be increased.
Calculation of the dose to give for breakthrough pain is easy once you understand it.
The dose of normal release morphine for breakthrough pain should be 1/6 of the total 24 hour morphine dose.
In this stem, increasing the oral morphine to 120 mg BD means that the total amount of morphine in 24 hours is 240 mg.
Breakthrough pain dose should be 240 mg/6 which is 40 mg.
Hence, 40 mg of oral morphine should be prescribed as 4 hourly PRN in addition to the BD dose of morphine.
INTERESTING FACT: This method of using one sixth of the total 24 hour dose as a breakthrough dose is a traditional method.
Now, with the newer modified-release analgesia, some physicians are choosing to use only 10% of the total daily regular dose as the as-required breakthrough dose as there is a better balance of analgesia with adverse effects.
Q.7. A 60 year old man developed ankle swelling shortly after starting antihypertensive medication. What is the most likely antihypertensive medication which could account for his symptoms?
Correct Answer : B
One of the known side effects of calcium channel blockers is swelling of the ankle. Calcium channel blockers widen the narrow blood vessels (vasodilation), causing redistribution of fluid from the vascular space, and for some people, this can cause more fluid to leak out of the blood into the tissues around the ankle resulting in swelling.
Calcium channel blockers can be divided into two types, dihydropyridines, which are predominantly vasodilators and generally have neutral or increased effects on vascular permeability (Amlodipine and Nifedipine); and
non-dihydropyridines (verapamil and diltiazem) which reduce vascular permeability and affect cardiac contractility and conduction. All of these can cause ankle swelling.
Q.8. A 48 year old man after surgical removal of mandibular cancer presents with perioral paresthesia and severe perioral pain which is not relieved by oral morphne and ibuprofen. The skin is also very tender to touch. What is the most appropriate next step in management to relieve the pain?
Correct Answer : A
The pain is likely due to a nerve injury during the operation. Neuropathic pain follows damage or disruption of the nervous system, and
it is often difficult to treat and responds poorly to standard analgesia.
Gabapentin is licensed for neuropathic pain which is described in this stem. Alternatively, amitriptyline could also be used if it was in the options.
Q.9. A 5 year old boy was rushed to the emergency department unconscious after he had taken methadone belonging to his sister. He was given naloxone and he regained consciousness. After a while he started getting drowsy again. What is the most likely reason for his drop in level of consciousness?
Correct Answer : B
Naloxone has a shorter plasma half-life than all opioid analgesics and so coma and respiratory depression often recur when naloxone wears off. Careful observation of the patient is essential and repeated doses of naloxone may be needed.
Q.10. A 69 year old man presents, has a history of stage 4 prostate cancer. He has been having back pain over the past year which is well controlled with oral morphine. Over the past few weeks, his morphine dose was increased as his back pain was worsening. Since then he has started vomiting and feeling nauseous. The oral morphine was ceased and replaced with a fentanyl patch and he was started on metoclopramide by the palliative team. A few weeks after the change of medications, he develops neck stiffness, high fevers, pallor, excessive sweating and muscle rigidity. What is the most likely cause of these symptoms?
Correct Answer : C
Extrapyramidal side effects are a very common side effect of metoclopramide which is an antidopaminergic drug.
Symptoms include dystonia, akathisia, parkinsonism, bradykinesia, and tremors. The high fever in this stem could represent a syndrome called neuroleptic malignant syndrome (NMS).
Neuroleptic malignant syndrome is a life-threatening reaction that occurs in response to neuroleptic or antipsychotic medications (usually haloperidol). Metoclopramide is one of the medications that may induce neuroleptic malignant syndrome
. Symptoms usually include high fevers, confusion, agitation, muscle rigidity, sweating, and tachycardia. The onset of these symptoms usually occurs after a few weeks of starting the medication but the symptoms can occur at any time.
NEUROLEPTIC MALIGNANT SYNDROME Neuroleptic malignant syndrome is a rare but life-threatening reaction to anti-dopaminergic medications.
Onset is usually within a few weeks of starting the anti-dopaminergic medication but can occur at any time. Features
• High fever
• Rigidity
• Confusion or altered consciousness
• Variable blood pressure
• Tachycardia Management
• Stop offending medication
• Rapid cooling
• Dopaminergic agents such as bromocriptine.
Q.11. A 67 year old man with advanced prostate cancer is on long term treatment with oral tramadol for pain. He was admitted to the hospital for treatment by the medical team because of a 2 week history of productive cough and a high fever. During his admission, he becomes more unwell and is unable to tolerate oral medication. The medical team would like to determine the appropriate dose of intravenous morphine to administer for pain relief in the hospital. He would normally take a total of 600 mg of tramadol hydrochloride a day. What is the MOST appropriate total dose of background intravenous morphine to be administered over 24 hours?
Correct Answer : C
100 mg of tramadol is equivalent to around 5 mg of intravenous morphine. So 600 mg of tramadol would equate to 30 mg of intravenous morphine. OPIOID EQUIVALENT DOSES Below is an approximate guide for converting opioid analgesics Opioid analgesic Route Dose Codeine PO 100 mg Diamorphine IM, IV, SC 3 mg Dihydrocodeine PO 100 mg Morphine PO 10 mg Morphine IM, IV, SC 5 mg Oxycodone PO 6.6 mg Tramadol PO 100 mg
The following are important points of relative potency conversions which is a need to know for the exam:
• Oral morphine has 1/2 the potency of oral oxycodone.
When converting from oral morphine to oxycodone, use 1/2 of the dose
• Oral morphine has 1/2 the potency of injectable morphine. When converting from oral morphine to injectable morphine, use 1/2 the dose
• Oral morphine has 1/3 the potency of injectable diamorphine. When converting from oral morphine to injectable diamorphine, divide the dose by three.
Q.12. A 52 year old man has a history of prostate cancer and bone metastasis. He has been taking regular codeine orally for his back pain for the past year. For the past three months, he finds the back pain worsening. He often wakes up in the middle of the night due to the back pain. What is the most appropriate management?
Correct Answer : D
The question here is written to test your understanding of the pain ladder. As the pain is not well controlled, we should move up on the pain ladder. The pain ladder consists of 3 steps:
1: Simple analgesia like paracetamol. Aspirin, NSAIDs +/- adjuvant therapy
2: Weak opiates: e.g codeine, tramadol, dihydrocodeine +/- adjuvant therapy
3. Strong opiates: morphine, fentanyl patches, diamorphine, oxycodone +/- adjuvant therapy.
If the patient is still in pain, you should never go back a step on the pain ladder, only go forward. Dihydrocodeine is similar to codeine in its analgesic effect and would not benefit the patient.
There is no point in the patient taking 2 different types of opioids. If a patient is started on a strong opioid, the weaker opioids should be stopped. Oral oxycodone is twice the potency of oral morphine. It would not be suitable unless the patient has tried morphine for a few days first and has intolerable side effects like constipation.
Q.13. A 63 year old man presented with sudden onset of severe dyspnoea, orthopnoea, raised jugular venous pressure and bilateral basal crackles three days after an episode of myocardial infarction. A diagnosis of acute congestive cardiac failure was made and intravenous furosemide was started. What is the most likely electrolyte abnormality to be expected?
Correct Answer : B
Furosemide is a loop diuretic Loop diuretics The 3 main points that you need to know about loop diuretics are that it may cause:
1. Hypokalaemia
2. Hyponatraemia
3. Gout
Mnemonic: LOOP – HypOOnatraemia, HypOOkalaemia, GOOut
Q.14. A 65 year old with a diagnosis of terminal prostate cancer with bone metastasis has his pain usually well controlled with a fentanyl patch. He is on the palliative register. For the past several weeks, he has shooting pains radiating down both his arms to his hands. He describes it as a stabbing pain. What is the most appropriate pain relief?
Correct Answer : D
The pain is likely due to nerve-ending damage. Neuropathic pain follows damage or disruption of the nervous system and it is often difficult to treat and responds poorly to standard analgesia.
Gabapentin is licensed for neuropathic pain which is described in this stem.
Alternatively, amitryptiline could also be used if it was in the options as suggested by guidelines however note that although amitryptiline is used frequently for neuropathic pain. Its use is off-label. Bisphosphonates may be used as adjuvants for bone pain and radiotherapy can also be used to improve pain from bony metastases if severe, however, the history provided in this stem is more in line with neuropathic pain.
Q.15. A 34 year old man suffers from depression. He was recently started on sertraline by his doctor. When can a therapeutic effect of sertraline be seen?
Correct Answer : B
The onset of the therapeutic effect of Sertraline may be seen within 7 days. However, longer periods are usually necessary to demonstrate an appropriate therapeutic response. In general, an antidepressant effect is usually seen within 2 weeks of starting treatment. If no effect is seen after 2-4 weeks, adherence should be assessed.
Q.16. A 40 year old woman has repeated retching and intractable vomiting following an elective varicose veins ligation and stripping surgery a few hours ago. Her pain is well controlled but she feels extremely nauseous. What is the most appropriate medication to administer?
Correct Answer : C
Postoperative nausea and vomiting are experienced by about 25% of all patients. Administering more opioid-like substances are likely to worsen the nausea and vomiting. Intractable vomiting usually responds very well to ondansetron which is serotonin (5HT3) antagonist and
it is the most effective agent in these situations.
This is given as 4-8 mg slowly intravenously in adults. Other agents like metoclopramide can also be used. Any oral medication would not be of benefit here as she would just vomit out the medications almost immediately.
Q.17. A 74 year old terminally ill man with brain metastases is on palliative care and is being discharged from the hospital for end-of-life care at home to be looked after by his family. He suffers from multiple seizures and has been prescribed benzodiazepine for his seizures. Which is the best route of benzodiazepine administration for this patient?
Correct Answer : A
The choice of benzodiazepine here is between Buccal Midazolam and Rectal Diazepam. Guidelines do not discriminate between the two. However, Rectal Diazepam is preferred due to its availability and lesser cost as compared to buccal Midazolam.
Q.18. A 45 year old man has his pain controlled on oral morphine 60 mg twice daily following abdominal surgery. He has recently, however, been unable to take oral medication. What is the most appropriate management for this patient?
Correct Answer : A
Since this patient is unable to take oral medications at all, we can immediately eliminate (B), (C), and (D). So, we are now left with B As a guide, halve the 24-hour oral morphine dose to change to subcutaneous morphine. This patient is taking a total of 120 mg of oral morphine per 24 hours.
So the correct dose for subcutaneous morphine should be 60 mg per 24 hours (half the oral dose) by subcutaneous infusion. Please note, use one-third of the 24-hour oral morphine dose over 24 hours for conversion to subcutaneous diamorphine.
Q.19. A 45 year old diabetic man had recently started taking anti-hypertension therapy. 6 months later, his fasting blood glucose is 14 mmol/L. What is the most likely medication that would have caused this?
Correct Answer : B
The potential adverse metabolic effects of thiazide and thiazide-like therapy include elevations in the plasma glucose.
Bendroflumethiazide may lower carbohydrate tolerance and the insulin dosage of some diabetic patients may require adjustment.
Care is required when bendroflumethiazide is administered to patients with a known predisposition to diabetes.
Q.20. A 57 year old man with known squamous cell lung carcinoma has chronic right shoulder pain which had been well controlled with oral morphine in the past. He has now, however, been switched to a fentanyl patch to control his pain due to the nausea and vomiting side effects that he experienced from his morphine treatment. The patient claims that a few hours after he was switched to the fentanyl patch and gibven metoclopramide for his vomiting, his neck became weak and stiff. Other than his chronic pain medication, the patient takes no other medication or over-the-counter drugs. What is the most likely cause of this patient’s neck stiffness?
Correct Answer : C
This patient’s symptoms have everything to do with the fact that he was given metoclopramide for his nausea. It is important to note that neck stiffness can be communicated as being anything from muscle weakness to muscle pain by the patient.
Extrapyramidal symptoms are most commonly caused by antipsychotic drugs such as haloperidol. Other anti-dopaminergic drugs, like the antiemetic metoclopramide, can also result in extrapyramidal side effects.
Acute dystonic reactions can occur as well, and these occur shortly after treatment with metoclopramide.
Q.21. A 33 year old man visits his GP surgery as he has been suffering from depression for the past year. He has attended the GP surgery multiple times and has been referred for group cognitive behaviour therapy and introduced to self help methods which he feels have helped his depression. However, he still feels he needs more help as he has frequent low moods and has very little interest in daily activities. His GP has agreed to start him on a selective receptor reuptake inhibitor (SSRI). Which statement regarding SSRIs is correct?
Correct Answer : A
Antidepressant effect is usually seen within 2 weeks of starting an SSRI. If there is no effect seen after 2 to 4 weeks, it would be advisable to check patient adherence
. If there is no response after 4 weeks and the patient is compliant with his/her medication, consider increasing the dose or switching antidepressants. SSRIs do not cause hypernatraemia.
They do the opposite. They can exacerbate hyponatraemia, especially in the elderly. It is important to inform your patients to continue on the same dose of antidepressants even though they have gone into remission.
They should continue it for at least 6 months to reduce the risk of relapse after which they can reduce the dose slowly over 4 weeks. Note that fluoxetine does not require tapering of the dose over weeks because it has a long half-life.
A single antidepressant usually gives fewer side effects compared to combinations of antidepressants. If one SSRI is not effective, try an alternative SSRI.
Q.22. A 25 year old man has been suffering from breathlessness and wheeze for the last 3 months. He has been prescribed Salbutamol inhaler, to take 2 puffs as required. In the last 2 weks, his symptoms have worsened and he has been using his Salbutamol inhaler five times a week, more frequently during the day. He also complains of difficulty sleeping at night due to excessive coughing and breathlessness. What is the best medication to be added to his usual regime?
Correct Answer : D
According to the British Thoracic Society (BTS) Asthma guideline, the patient is currently on Step 1. As his asthma is not controlled (i.e. he is using his Salbutamol inhaler more than three doses per week), he should be moved up to Step 2 which is a regular low-dose corticosteroid inhaler.
Q.23. A patient has recently been diagnosed with Bipolar Disorder and is to be put on Lithium therapy. Her renal function and liver function tests are normal. What is the other test you need to do before commencing her on Lithium?
Correct Answer : A
Important tests to do before commencing Lithium therapy - Weight, pulse, and blood pressure - Renal function (primary excretion route) - Full blood counts, U&E - Thyroid function tests and calcium -
Baseline ECG - Baseline parathyroid hormone and magnesium As this patient has already had baseline renal function and liver function tests,
the next best test to do would be thyroid function tests (especially measurement of T4).
As Lithium can cause disease of the thyroid, it is important to exclude hypothyroidism or hyperthyroidism in a patient before commencing Lithium therapy.
Q.24. A 22 year old woman comes to see her general practitioner after having uprotected sex 2 days ago. She has been told by her friend about the copper intrauterine device (IUCD). She asks if he could explain the mechanisms of which this will prevent her from becoming pregnant. What is the most appropriate mechanism of action of copper intrauterine device to prevent pregnancy after unprotected sex?
Correct Answer : D
Emergency contraception Copper intrauterine contraceptive device Intrauterine devices work by inhibiting fertilization or implantation.
They should be inserted within 5 days of unprotected sexual intercourse (UPSI). It is the most effective form of emergency contraception with less than 1% pregnancy rates when IUCD is used as an emergency contraception.
Progestogen-only emergency contraception - Levonorgestrel Works by inhibiting ovulation and implantation but the mode of action is not fully understood. It should be taken as soon as possible as the efficacy decreases over time.
Licensed for use within 72 hours of UPSI. Ulipristal Acetate.
The main mechanism of action is by inhibition or delay of ovulation.
It should be taken no later than 120 hours (5 days) after intercourse.
Q.25. A 21 year old man presents with a red, circular shaped rash on his arm. He was prescribed Fucidin cream for 7 days to be applied but the rashes did not improve. He is complaining of itch around the area where the rashes appear. What is the next best choice of medication to be prescribed?

Correct Answer : D
Fucidin cream is an antibacterial cream (fusidic acid). If after a week, this has no response then it is most likely a fungal infection on the skin. The red, circular, and itchy rash is most probably a ringworm infection (dermatophytosis) which should respond to Clotrimazole cream.
Q.26. A 44 year old man weighing 80 kg presented for an operative procedure and was given 20 ml of 1% lidocaine without epinephrine prior to the procedure. If the maximum allowed dose is 4 mg/kg, how much more of 1% lidocaine can be given?
Correct Answer : C
Percentage concentration is based on g/100 ml so a 1% solution would be 1 g/100 ml or 1000 mg/100. This gives you 10 mg/ml This patient has already been given 20 ml of a 1% solution so he has been given 20 ml at 10 mg/ml. He has been given 200 mg of the drug.
The max dose is 4 mg/kg and this patient is 80 kg. So a maximum dose of the drug for him would be 320 mg. This means that he can only be given 120 mg more of the drug.
Since the answer choices are all in ml, we need to convert 120 mg to ml. 10 mg -= 1 ml 120 mg – x ml Cross multiply and solve for x and you will get 12 ml This patient can only be given 12 ml more of lidocaine.
Q.27. A 22 year old woman who is allergic to ciprofloxacin was prescribed 2 days of rifampicin for prophylaxis as her roommate was diagnosed with meningococal meningitis. She has been taking combined oral contraception for the past year and is sexually active. She does not wish to become pregnant. Which is the most appropriate advice to give her?
Correct Answer : A
Combined hormonal contraceptives are less reliable during treatment with rifampicin. Breakthrough bleeding and spotting are common, and pregnancies have occurred.
Barrier methods would be appropriate here as she only requires a short amount of time for extra contraceptive protection. Progesterone implants such as NexplBatman are not recommended with the use of a hepatic enzyme inducer as progesterone released into the bloodstream can be affected by the enzyme-inducing medication.
NexplBatman is also used for 3 years and would be unsuitable for an enzyme inducer which is only prescribed for 2 days. Allergy to ciprofloxacin has no association with an allergic reaction to rifampicin.
It is thrown in here because ciprofloxacin is the preferred choice over rifampicin by most individuals for meningococcal prophylaxis due to drug interactions.
What can be done? Use alternative methods (IUDs, depot or barrier methods), an increased ethinylestradiol dose (at least 50 micrograms during and for 28 days after rifampicin is stopped), an extended or tricycling regimen, or a suitable alternative antibacterial should be given.
Q.28. A 72 year old woman who is taking loop diuretics is suffering from palpitations and muscle weakness. What is the most likely electrolyte imbalance to be found?
Correct Answer : D
Please see Q- 13
Q.29. A 58 year old lady with breast cancer has metastatic spread to her lower vertebrae. Her current medications include morphine sulphate, paracetamol, ibuprofen and senna. She still complains of moderate to severe pain in her back. She is compliant with her medication. What is the best adjuvant to be added to manage her pain?
Correct Answer : A
The treatment of bone pain due to skeletal metastases in advanced breast cancer begins with analgesia according to the WHO’s analgesic ladder. This patient is already on paracetamol, ibuprofen, and opioids which are no longer helpful. The next step is to offer radiotherapy to provide pain relief. Bisphosphonates are an important adjunct to pain relief.
However, they take time to act (as long as six months). They do have a role in the “acute” management of metastatic bone pain, however, the indications of use are where treatment with conventional analgesia, radiotherapy, and surgery are either unsuccessful or inappropriate.
Dexamethasone is useful when there is evidence of cord compression along with radiotherapy. Vertebroplasty is useful in impending spinal fractures or if they have already occurred.
Q.30. A 35 year olf man with a history of alcohol abuse has oedema and ascites demonstrated by shifting dullness. Spider naevi is noted on his trunk. Paracentesis shows clear fluid. He has a temperature of 37.2 C, a pulse of 85 beats/minute, a blood pressure of 119/85 mmHg and a respiratory rate of 20 breaths/minute. What is the most appropriate medication to start?
Correct Answer : B
Oedema and fluid overload in third spaces, such as ascites, are managed with diuretics. The diuretic most useful in cirrhosis is spironolactone.
This is because cirrhotics have intravascular volume depletion, which results in a high aldosterone state. Spironolactone is an aldosterone antagonist.
Common indications of spironolactone - Ascites: patients with cirrhosis develop a secondary hyperaldosteronism. - Hypertension: used as one of the last treatment options (in a 'step 4' treatment) - Heart failure - Nephrotic syndrome.
Q.31. A 30 year old lady comes to the emergency department with palpitations and chest pain. ECG shows sinus tachycardia. Her pulse rate is 110 beats/minute. She has a history of asthma and her GP recently changed her medications. What is the most appropriate management?
Correct Answer : C
She most likely started a beta agonist to treat her asthma which is known to cause tachycardia.
Q.32. A 72 year old man has been on warfarin for atrial fibrillation for the last 2 years. He is not on any other medication. Which symptom would be the most alarming?
Correct Answer : B
A headache that may result from intracranial haemorrhoage due to Warfarin is the most important adverse effect – and patients should be counseled to report any unusual or persistent headache whilst taking Warfarin.
Q.33. A 45 year old man has recently had an anterior resection of the rectum. Postoperatively, he was on oxycodone which controlled the pain. He started vomiting several times on the second day and a mild intestinal obstruction is suspected. What is the most appropriate management for his pain?
Correct Answer : C
Intravenous morphine would be the most suitable as he is not able to tolerate opioids orally due to the vomiting. There is no rationale behind picking a fentanyl patch as an option. Whilst it is true that if the pain is stable and the oral route is no longer appropriate (e.g. vomiting),
fentanyl patches are a good choice however, the pain here is not stable. The pain was well controlled with oral oxycodone which he has now started to vomit out. He will be in pain again.
Fentanyl is a strong opioid. Due to its long half-life, it will take at least 12 to 24 hours to achieve therapeutic drug levels and so is only of benefit in patients with stable pain. If you had given this to the patient, he would be in severe pain for several hours while waiting for the therapeutic drug levels to kick in.
Fentanyl patches are usually used in cancer patients who have stable pain and are not able to tolerate oral medication. It is not reasonable to use constipation as an excuse in this example to avoid the use of intravenous morphine.
The bottom line is constipation can be prevented or greatly reduced with laxatives but postoperative pain cannot be relieved with a slow-releasing transdermal patch.
Q.34. A 78 year old man who was previously on 120 mg slow release oral morphine and paracetamol 1 g QDS had his dose increased to 200 mg slow release oral morphine. He is still in significant pain but complains of drowsiness and constipation. What is the most appropriate step in the management?
Correct Answer : A
In general, oxycodone should be used when patients are still in pain but have side effects of opioids. This is because oxycodone has twice the potency of morphine to manage pain but with fewer side effects compared to morphine. The pain ladder consists of 3 steps:
1: Simple analgesia like paracetamol. Aspirin, NSAIDs +/- adjuvant therapy
2: Weak opiates: e.g codeine, tramadol, dihydrocodeine +/- adjuvant therapy
3. Strong opiates: morphine, fentanyl patches, diamorphine, oxycodone +/- adjuvant therapy.
If the patient is still in pain, you should never go back a step on the pain ladder, only go forward.
Q.35. A 45 year old man with known type 1 diabetes mellitus has an ulcer on his right ankle with agonising burning pain. The pain has been gradually worseing over the past few months. The pain is worse when he walks and during late hours of the night. He has regular inspection of his feet and has normal sensation and palpable pulses. His glucose levels have not been well controlled over the past year, and he is currently undergoing investigations for diabetic retinopathy and diabetic nephropathy. What is the most appropriate management for his pain?
Correct Answer : C
This patient has symptoms of diabetic neuropathy. It is often tricky to diagnose as neuropathic pain may present in different ways such as burning, tingling, numbness, and itching.
This stem includes burning as one of the symptoms. The evidence of diabetic nephropathy and diabetic retinopathy is included here as patients with these complications are more likely to have signs of neuropathy. Amitryptiline works well with neuropathic pain, and so it is the answer here. The other medications that are NICE recommended for the initial treatment of neuropathic pain include duloxetine, gabapentin, or pregabalin however amitryptiline is usually used as first-line as it is cheaper and has a simple once-a-day dosing. Capsaicin cream is licensed for use in diabetic neuropathy but it is not the first line.
They are usually used for patients who are not able to tolerate oral treatments. Nerve blocking agents refer to local anaethetics such as lidocaine. They are usually only given as a form of temporary relief such as a femoral nerve block prior to a knee replacement.
While lidocaine does have a role in diabetic neuropathy, it is mainly used for refractory painful neuropathy. Furthermore, its administration is complex and it is given intravenously with ECG monitoring.
Aside from pharmacological interventions, good glycaemic control is vital in managing diabetic neuropathy.
Q.36. A 74 year old man has been taking Warfarin 7 mg daily for the treatment of left arm DVT with an INR target of 2-3 for the past two years. He also takes Furosemide 40 mg daily, Diprobase cream and Co-dydramol when required for pain relief. He is usually compliant with his medication. What is the most important adverse effect the patient should be careful with?
Correct Answer : A
Headache which may result from intracranial haemorrhage due to Warfarin is the most important adverse effect – and patients should be counselled to report any unusual or persistent headaches whilst taking Warfarin.
Q.37. A 32 year old man on psychiatric medications complains of the inability to ejaculate. What is the most likely medication he is taking?
Correct Answer : B
Sexual dysfunction is a common symptom of depression. However, in addition to this, all antidepressants can cause sexual dysfunction to varying degrees (most commonly serotonin reuptake inhibitors).
Table
1. Sexual adverse effects of antidepressants Drug - Selective serotonin reuptake inhibitors (SSRIs) Prevalence - 60 - 70% Type of the problem experienced -
• All phases of the sexual response
• Paroxetine is associated with more erectile dysfunction and vaginal dryness than other SSRIs Drug - Tricyclic anti-depressants (TCAs) Prevalence - 30% Type of the problem experienced -
• Decreased libido, erectile dysfunction, delayed orgasm, and impaired ejaculation Drug - Venlafaxine Prevalence - 70% Type of the problem experienced -
• Decreased libido, delayed orgasm, and erectile dysfunction. Rarely painful ejaculation and priapism Drug - Mirtazapine Prevalence - 25% Type of the problem encountered -
• Decreased libido, delayed orgasm, erectile dysfunction, absence of orgasm Drug - Reboxetine Prevalence - 5-10% Type of problem experienced -
• Orgasm abnormalities Drug - Duloxetine Prevalence - 46% Type of the problem encountered -
• Delayed orgasm Drug - Irreversible monoamine oxidase inhibitors (MAOIs) Prevalence - 40% Type of the problem experienced -
• Decreased libido, erectile dysfunction, delayed orgasm, and impaired ejaculation • Moclobemide is less likely to cause sexual dysfunction compared with older MAOIs (4% versus 40%).
Q.38. A 48 year old man with renal cell carcinoma had radiotherapy for metastatic spinal cord compression at the 11th thoracic vertebra 4 weeks ago. He has retained sensation of his legs but is unable to stand due to muscle weakness and pain. He has pain around his lower trunk which is relieved by regular oral morphine however he has been increasingly distressed due to his painful muscle spasms on his right leg. What is the most appropriate management to treat his symptoms?
Correct Answer : C
Muscle relaxants such as Baclofen and Diazepam are very good medications to provide relief from muscle spasms. They are often used as adjuvants of pain control in palliative care.
Q.39. A 67 year old man attends the accident and emergency department with a productive cough, temperature and rigors. Chest radiograph demontrates right upper zone consolidation and he is started on clarithromycin antibiotics as he is penicillin allergic. His CURB-65 score on admission is 2. His current medical treatment consists of ramipril 5 mg once a day, metformin 1 g twice a day, simvastatin 40 mg at night. What adjustments to his medications should be made?
Correct Answer : D
Clarithromycin is a macrolide antibiotic and is a potent CYP3A4 inhibitor. Clarithromycin is contraindicated with the use of simvastatin. This is because clarithromycin can alter the metabolism of simvastatin leading to an increase in plasma levels and therefore increasing the risk of myopathy and rhabdomyolysis.
Note the advice regarding atorvastatin is to not exceed 20 mg daily if concomitant use with clarithromycin is required.
There is no indication to reduce his metformin dose. Unless he has developed an acute kidney injury or his blood pressure remains low (both parameters not given), there is no indication to reduce his ACE inhibitor.
The CURB-65 score has also been mentioned in this question.
It is worth knowing that the score is a predictor of 30-day mortality for community-acquired pneumonia and ranges from a score of 0 to 5.
It is made up of Confusion (AMTS < 8/10) Urea (> 7 mmol/L) Respiratory rate (30 bpm or above) BP (< 90/60) Age (65 years or above).
Q.40. A 24 year old woman was prescribed azithromycin for a sexually transmitted infection. She has been using a form of contraception for the past year. Which most likely contraceptive method is likely to be affected by azithromycin?
Correct Answer : D
It was previously thought that hepatic enzyme inhibitor drugs (like azithromycin) may affect COCP but was later discovered that that there were no significant interaction Only drugs like rifampicin have an interaction with COCP. Combined hormonal contraceptives are less reliable during treatment with rifampicin.
Breakthrough bleeding and spotting are common, and pregnancies have occurred when the patient is on rifampicin and COCP.
Q.41. A 24 year old woman was prescribed amoxicillin for an episode of otitis media. She has been using the combined oral contraceptive pill as a form of contraception for the past two years. What is the most appropriate advice to give her with regards to antibiotic use and taking the COCP?
Correct Answer : A
According to latest recommendations, no additional contraceptive precautions are necessary when antibiotics that do not induce liver enzymes are used together with combined oral contraceptives, unles diarrhoea or vomiting occur.
Q.42. A particular drug is undergoing a trial assessing both the oral and intravenous routes of administration. The two graphs below demonstrate the rate of absorption for both routes of administration. What is the most likely reason for this to occur?
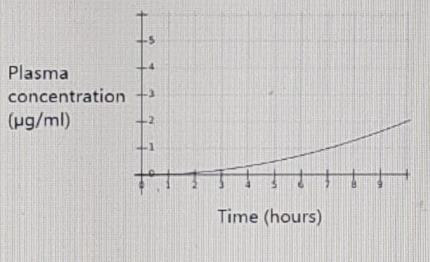
Correct Answer : C
The question is testing your knowledge of pharmacology. The area under the curve is the area underneath the graph where plasma concentration of the drug (y) is plotted against time after drug administration (x) and this is most important when looking at these types of questions.
The first-pass effect is where the concentration of a drug is reduced before it reaches systemic circulation. When a drug is administered orally, it travels through the gut, then through the portal system, and into the liver.
The liver metabolizes most drugs and toxins that enter the body and only allows a certain fraction to enter systemic circulation. This ‘first pass’ through the liver reduces the bioavailability of the drug in question. Drugs that are administered via other routes such as the intramuscular, intravenous, and sublingual route bypass being metabolized by the liver, and so the bioavailability of these drugs is greater.
Simply put, a larger area under the curve means a greater drug bioavailability and vice-versa. It would make sense that a drug administered orally would have lesser bioavailability than a drug administered intravenously, therefore hepatic first-pass elimination is the correct answer. Renal clearance of the drug does not pertain to this question at all therefore an increased renal clearance of the intravenous drug and a reduced renal clearance of the intravenous drug is incorrect.
Bioavailability increases in patients who have liver disease since the liver is unable to metabolize substances with efficacy therefore reduced hepatic absorption is incorrect. Increased bioavailability of the drug is incorrect since the oral route would have a decrease in bioavailability as compared to the intravenous route.
Q.43. A 65 year old man with hypertension develops gingival hyperplasia. What is the most likely medication causing the gingival hyperplasia?
Correct Answer : D
Gingival hyperplasia is a recognized side effect of calcium channel blockers.
Q.44. A 37 year old female patient has been taking doxycycline 100 mg daily for acne for the past two weeks. She complains of feeling nauseous and having frequent diarrhoea since starting the medication. She has no known allergies and occasionally buys paracetamol over the counter. What is the most appropriate advice to be given to this patient?
Correct Answer : B
Side effects known to Doxycycline include headache, nausea, diarrhoea, vomiting, and oesophageal irritation. These side effects can be minimized by advising patients to swallow Doxycycline capsules as a whole, while sitting or standing, with a full glass of water with meals. This reduces the likelihood of feeling nauseous.
In this stem, doxycycline is used however nausea is not specific to doxycycline but to a range of other antibiotics as well. Nausea is one of the most common side effects of any medication.
Virtually all medication has some ability to cause stomach issues. It is important to educate patients on how to reduce the likelihood of nausea to ensure good compliance and the optimum benefit of the medication prescribed.
Antiemetics like promethazine and prochlorperazine are not a good choice in this case.
Firstly, simple advice like taking medication on a full stomach may already do the trick and eliminate the side effects of some medications. Secondly, antiemetics are used for short-term offenders or opioid-induced nausea. This patient is likely to be taking doxycycline for a long period.
Q.45. A 32 year old man has recently been laid off work due to his drinking habits. He drinks half a litre of vodka (ABV 40%) and a pint of beer (3.5%) in a week. How many units of alcohol is he drinking in a week?
Correct Answer : C
One unit equals 10 ml or 8 g of pure alcohol. It is around the amount of alcohol the average adult can process in an hour. In theory, there should be little or no alcohol left in the blood of an adult after one hour of drinking one unit.
Q.46. A 33 year old lady who is an opiate drug addict presents to the local community addiction team for assessment as she wants to quit her drug abuse problem. She is supported well by her friends and family. What is the most appropriate treatment to combat withdrawal symptoms?
Correct Answer : A
Methadone is used to help combat withdrawal effects for opiate misusers. Methadone is an opioid medication and it reduces withdrawal symptoms in people addicted to heroin. It does not cause the “high” associated with drug addiction and thus it is especially helpful for opiate addicts to help them quit the drug addiction problem.
Q.47. A 30 year old man is referred to the local community addiction team for assessment and treatment. He has been taking heroin for a number of years and would like help for his opioid dependence. Which is the most likely medication to be offered to him as first-line for community based detoxification?
Correct Answer : A
NICE has proposed that either methadone or buprenorphine can be offered as a first-line treatment for detoxification. Buprenorphine is not among the options, so methadone is the answer. Methadone is an opioid receptor agonist, so it acts similarly to heroin, and
hence it is used in opioid substitution therapy as part of the detoxification program. Detoxification can last anywhere from up to four weeks in an inpatient/residential setting and up to 12 weeks in the community.
METHADONE is the METHoD number ONE to detoxify Lofexidine can be used for patients who would like a shorter detoxifying period, who have mild or uncertain dependence, and
who have decided not to use methadone or buprenorphine to detoxify. Naloxone is an opioid receptor antagonist (opposite to methadone which is an opioid receptor agonist). Its main use is reversing the effects of opioids in acute opioid overdose. Naltrexone is an opioid antagonist (like naloxone) but with a longer half-life.
It has a role as an adjuvant in preventing relapses in opioid-dependent patients who have remained opioid-free for at least 7-10 days. Codeine is a weak opioid with no role in opioid detoxification.
Q.48. A 64 year old man diagnosed with a nasopharyngeal carcinoma 6 months ago is having recent difficulty swallowing his tablets. He takes regular morphine sulphate 20 mg twice a day for his localised pain as part of his palliative care plan. He has minimal side effects from the use of oral morphine which manages the pain well. His last blood test shows no liver or renal impairment. What is the most appropriate action?
Correct Answer : D
Oral morphine is usually offered to patients with pain from progressive cancer as part of palliative care much like in this stem. If they have difficulty swallowing, oral medications would be inappropriate. Another route to deliver the same equivalent dose of the opioid should be offered.
In the scenario of a palliative patient with “stable” pain, patches would be the most appropriate way as they are easy to use and can be managed at home.
The doses of fentanyl are not likely to be asked at this level but for those who would like to know more, a transdermal fentanyl 12 microgram patch is equivalent to approximately 45 mg oral morphine daily.
Q.49. An 18 year old female is rushed into Accident & Emergency following the ingestion of 33 tablets of paracetamol. Her mother mentions that her daughter was devastated at not getting into the university of her choice. The patient’s parents found her unconscious on her bedroom floor two hours later. Physical examination reveals a Glasgow coma scale (GCS) score of 11/15. Blood sampling was done two hours later and showed a plasma paracetamol level that is above the treatment line. A decision was subsequently made to commence intravenous N-acetylcysteine treatment. Which of the following is the best description for the mechanism of action of N-acetylcysteine?
Correct Answer : B
When faced with a question of this type, choose the answer that makes the most sense in the context of the question. You already know that a paracetamol overdose causes liver damage. This happens because a metabolite of paracetamol decreases stores of the antioxidant glutathione. Decreased stores of glutathione cause liver cells to be damaged by free radicals. When N-acetylcysteine is given,
it is broken down into L-cysteine which then gets converted to glutathione which in turn protects from damage from free radicals.
N-acetylcysteine inhibits cytokine NF-kB and not interferon-alpha. It has a minimal effect on cytochrome P450 enzymes.
N-acetylcysteine causes the breakdown of sulfhydryl bonds.
This additional effect of N-acetylcysteine also makes it useful as a mucolytic treatment in patients with respiratory conditions.
N-acetylcysteine increases glutathione stores.
Q.50. A 34 yer old female presents to Accident & Emergency with the complaint of right calf pain. Further questioning reveals that the patient had been started on the combined oral contraceptive pill (COCP) three weeks ago. She takes no other medications and has no other medical conditions. On examination, the patient’s right leg appears swollen below the knee. She was then given low molecular weight heparin (LMWH) subcutaneously. What is the best description for the mechanism of action of low molecular weight heparin?
Correct Answer : A
Heparin works by binding to antithrombin (AT) III, resulting in its activation. The activated antithrombin (AT) III then inactivates thrombin via the inhibition of prothrombin (coagulation factor II), factor Xa, and other proteases of the coagulation cascade.
Regardless of whether heparin is administered at a high dose or a low dose or whether it is delivered as low molecular weight heparin (LMWH) or unfractionated heparin (UFH), the initial mechanism of action is the same (the activation of antithrombin) although later interactions might differ.
During the normal coagulation cascade, thrombin is converted to fibrinogen which is, in turn, converted into strands of fibrin.
Even though heparin does decrease the conversion of fibrinogen to fibrin by inhibiting thrombin, this is indirectly done and the single best description of how heparin works is the inhibition of prothrombin to thrombin.
Q.51. A 76-year-old is treated for HTN (hypertension). He suffers from pain and redness at the MTP joint of his right big toe. Which of the following anti-HTN cause this symptoms?
Correct Answer : B
Ans. The key is B. Bendroflumethiazide [ Thiazide diuretics may cause hyperuricemia and thus cause or precipitate gout].
Q.52. A 4-year-old boy with a febrile convulsion lasting eight minutes has been given IV lorazepam to control them. What is the most likely serious side effect?
Correct Answer : C
Ans. The key is C. Apnoea. [Respiratory depression may occur following lorazepam administration].
Q.53. A 71-year-old man presents with coarse tremor. He is on some medication. Which one can be the reason for the tremor?
Correct Answer : A
Ans. The key is A. Lithium. [Lithium overdose can cause coarse tremor].
Q.54. A 40-year-old manic depressive is noted to have high serum levels of lithium and profound hypokalemia. His GP had started him on anti-hypertensive. Choose the most likely cause?
Correct Answer : D
Ans. The key is D. Thiazide. [Thiazide was prescribed for hypertension and when lithium was prescribed its level increased due to thiazide (Thiazide diuretics have a significant potential to increase serum lithium concentrations.
These diuretics induce a natriuresis that leads to a compensatory increase in the reabsorption of sodium (and lithium) in the proximal tubule) and thiazide also caused hypokalemia resulting in the given picture].
Q.55. All the following drugs do not cause bronchoconstriction except?
Correct Answer : A
The key is A. Atenolol
Q.56. A 32-year-old man on psychiatric medications complains of inability to ejaculate. Which drug is most likely to cause these symptoms?
Correct Answer : D
Ans. The key is D. Fluoxetine. [SSRIs are frequently associated with delayed ejaculation].
Q.57. A 34-year-old diabetic patient is undergoing contrast radiography. What measure should be taken to prevent renal damage with contrast dye?
Correct Answer : B
The key is B. Plenty of fluids
Q.58. A 35-year-old IVDA (Intra Venous Drug Abuser) on penicillin and flucloxacillin for cellulitis now presents with jaundice, pale stools and dark urine. What is the most likely diagnosis?
Correct Answer : B
Ans. The key is B. Cholestatic jaundice. [Flucloxacillin can cause cholestasis and hence cholestatic jaundice].
Q.59. A 72-year-old man has been on warfarin for 2 years because of past TIAs and strokes. What is the most important complication the patient should be careful with?
Correct Answer : A
Ans. The key is A. Headache. [Headache from intracranial hemorrhage is more important complication about which patient should be careful with (it is more important than osteoporosis)].
Q.60. A patient on antihypertensive drugs develops hyperkalemia. Which anti-hypertensive is likely to cause it?
Correct Answer : A
Ans. The key is A. Ramipril. [Both ramipril and losartan can cause hyperkalemia]
Q.61. A boy was rushed to the ED unconscious after he had taken methadone belonging to the sister. He was given naloxone and he regained consciousness. After a while he started getting drowsy again. What is responsible for his present drop in level of consciousness?
Correct Answer : D
The key is D. Naloxone is eliminated faster than methadone
Q.62. A lady with depression has a bag full of medicine. She now presents with coarse tremors. Which drug caused her symptoms?
Correct Answer : D
Ans. The key is D. Sodium valproate. [As the bag is not empty but full of medicine this is not a case of over-dose. The side effect of lithium in the therapeutic range is fine tremor. Sodium valproate (a well-known mood stabilizer) can cause coarse tremors in the therapeutic range].
Q.63. A patient taking doxycycline complains of nausea, indigestion, abdominal pain and vomiting. What will you advise?
Correct Answer : A
The key is A. Take it after a meal
Q.64. A 72-year-old lady is drowsy and her relatives want to take her home. She has been prescribed diazepam 2.5mg. What is the best delivery route?
Correct Answer : D
The key is D. Per rectal
Q.65. A man presents with inoperable carcinoma and back pain. His pain has been well controlled with morphine but he develops vomiting. Morphine was stopped and he was started on metoclopramide and fentanyl patches. He then develops neck stiffness and fever. What is the cause of these symptoms?
Correct Answer : A
Ans. The key is A. Metoclopramide. [Extrapyramidal effects like neck stiffness are common side effects of metoclopramide and also there is a rise in temperature].
Q.66. What are the side effects of thiazide diuretics?
Correct Answer : B
Ans. The key is B. Hyponatremia. [Thiazide causes hypercalcemia, hypokalemia and hyponatremia].
Q.67. A 4-year-old boy ingested his grandmother’s medicine and has developed dilated pupil. What is the cause?
Correct Answer : A
The key is A. Amitryptiline
Q.68. A patient is on loop diuretics. What effect do loop diuretics produce?
Correct Answer : A
Ans. The key is A. Low Na+, Low K+. [Loop diuretics causes hyponatremia and hypokalemia].
Q.69. A patient being sedated with fentanyl develops severe respiratory depression. This is best reversed using which drug?
Correct Answer : B
The key is B. Naloxone. [Opioid Antagonist, reverses the effects of fentanyl, though it has to be administered for a longer period due long half-/life of fentanyl]
Choose a Question
×Choose a Question
×
Trial Access Limit Reached
You’ve reached the limit of free content. Subscribe to continue learning without restrictions.