

Hello,
Dr. Batman
Hello Doctor, Welcome!
Profile

Name: Batman
Email: batman@gotham.com
RESPIRATORY MEDICINE
(Total Questions - 163)Q.1. A 32 year old female smoker has a history of wheeze, shortness of breath and fever. Her past medical history includes eczema. FEV1/forced vital capacity (FVC) was measured and was found to be low. This was improved after taking bronchodilators. What is the most likely diagnosis?
Correct Answer : B
Asthma is characterized by paroxysmal and reversible obstruction of the airways. It is a clinical diagnosis based on : A history of recurrent episodes of wheezing, chest tightness, breathlessness, and/or cough, particularly at night- Evidence of generalized and variable airflow obstruction, which may be detected as intermittent wheeze on examination or via tests such as peak expiratory flow (PEF) measurement.
Acute asthma involves:
- Bronchospasm (smooth muscle spasm narrowing airways)
- Excessive production of secretions (plugging airways)
Risk factors :
- Asthma is due to a combination of genetic and environmental factors
- Personal history of atopy
- Family history of asthma or atopy
- Inner city environment; socio-economic deprivation
- Prematurity and low birth weight
- Viral infections in early childhood
- Smoking
- Maternal smoking.
Presentation :
- Cough
- SOB
- Wheeze
- Chest tightness
Classically, these are variable, intermittent, worse at night and in early morning, and are associated with specific triggers.
Triggers include : Pollens, cat and dog, cold air, perfumes.
Note: Symptoms may present after taking aspirin or beta-blockers.
Examination:
- May be entirely normal.
- In a mild attack : Slight tachypnoea, and tachycardia
- Classically, an expiratory wheeze is heard (widespread wheeze)
In severe life-threatening attacks :
- Use of accessory muscles for respiration
- Diminished breath sounds, loud wheezing, and hyper-resonance (increased vocal fremitus) and intercostal retraction
- The chest may appear hyperinflated
- Sometimes, in severe life-threatening asthma, there may be no wheeze at all a silent chest.
- In long-standing/poorly controlled asthma :
- Chest deformity/hyperinflation may be seen.
Diagnosis: This is often a clinical diagnosis but should be supported by objective measurements.
The diagnosis is based on the presence of :
- Symptoms (cough, wheeze, breathlessness)
- PFTs show an obstructive pattern that typically reverses with bronchodilation
- Otherwise unexplained peripheral blood eosinophilia.
Where the diagnosis is uncertain (intermediate probability) but with a demonstration of airway obstruction (FEV1/forced vital capacity (FVC) <0.7), reversibility testing and/or atrial treatment are suggested.
Chest x-ray findings are nonspecific in an asthmatic attack. It should not be used routinely in the assessment of asthma but consider CXR in any patient presenting with an atypical history or with atypical findings on examination. CXR if atypical symptoms, may show hyperinflation. The chest x-ray may help rule out acute infection as the cause of an acute attack.
One differential diagnosis that is worth mentioning is COPD.
- Reversibility distinguishes asthma from COPD
- COPD is rarely totally refractory to medication.
- Almost all patients with COPD do smoke or have smoked in the past.
- Asthmatics can also develop COPD.
Q.2. A 6 year old girl has had 2 short episodes of cough and wheeze over the last 12 months. These 2 acute episodes responded quickly to bronchodilator. She has no symptoms or abnormal physical signs at the moment. She has slight eczema and her mother has a history of asthma when she was young. What is the most appropriate investigation?
Correct Answer : D
Spirometry is now preferred over peak flow masurement for initial confirmation of obstrucion of airways in the diagnosis of asthma, as it is felt to offer clearer identification of airway obstruction, to be less effort-dependent and more repeatable.
Q.3. A 68 year old woman presents to the emergency department from her nursing home complaining of shortness of breath. She has a temperature of 38.7 C and productive cough. Her sputum is noted to be a rusty colour. On auscultation, crackles are heard over the right lung base. A chest X-ray was done and shows right lower lobe consolidation. She has a blood pressure of 100/65 mmHg and a pulse rate of 102 beats/minute. A urinalysis shows 1+ leukocytes with no nitrates or protein. What is the most likely organism causing her symptoms?
Correct Answer : A
This is a typical presentation of streptococcus pneumoniae infection. Streptococcus pneumonia (pneumococcus) is the most common cause of community-acquired pneumonia.
The urinalysis does not correlate with the pneumonia. It is important to remember that urinary tract infections are a common cause of sepsis in the elderly, but in this case, it is not a UTI as the findings are associated with pneumonia.
Q.4. A 48 year old man with a 30 pack year smoking history is found to have an incidental finding of a chest X-ray showing a 2 cm hilar mass and was referred to the respiratory team for a biopsy. The histology report has returned with findings of large polygonal cells containing keratin pearls and intercellular bridges. What is the most likely type of lung cancer?
Correct Answer : B
Histopathologically, squamous cell carcinomas can be divided into keratinizing and nonkeratinizing types. Keratinizing carcinomas are defined as tumours in which malignant cells produce extracellular keratin, most frequently in the form of keratin pearls. This question tests your histopathology knowledge.
Knowing that squamous cell carcinoma cell histology can be described as islands of large polygonal malignant cells containing keratin pearls and intercellular bridges is the only step to getting this answer correct.
Other hints to help you with this question:
• Squamous cell carcinoma has a strong smoking history link whereas adenocarcinomas are the most common type of lung cancer in NON-smokers.
Note: Although adenocarcinoma is the most common type of cancer in non-smokers, the majority of patients who develop adenocarcinoma are indeed smokers.
• Squamous cell carcinomas usually present centrally whereas adenocarcinoma and large cell lung carcinoma present peripherally.
Mnemonic: Squamous cell carcinoma and Small cell lung cancer present Sentrally (central lesions).
Q.5. A 27 year old female attends outpatient department with a fever and dry cough. She has had a headache, muscle pain and joint pain for more than one week. She has a temperature of 37.5 C, a pulse of 100 beats/minute, a blood pressure of 110/70 mmHg and a respiratory rate of 20 breaths/minute. A Chest X-ray report shows bilateral patchy consolidation. What is the most likely causative organism?
Correct Answer : A
Mycoplasma pneumoniae is a cause of atypical pneumonia which often affects young adults.
Features - the disease typically has a prolonged and gradual onset - flu-like symptoms classically precede a dry cough - bilateral consolidation on x-ray.
Note: Occasionally, exam may also give a presentation of erythema multiforme along with the atypical pneumonia symptoms. Erythema multiforme is one of the features of infection with mycoplasma pneumoniae.
Q.6. A 67 year old smoker presents with cough, breathlessness and wheeze. 24% oxygen by Venturi face mask was initiated and nebulized salbutamol and hydrocortisone were administered. As his dyspnoea did not improve, intravenous aminophyllin was administered and an arterial blood gas was sent. He has a respiratory rate of 32 breaths/minute. His arterial blood gas results show: pH 7.32 pCO2 7.7 kPa pO2 10.1 kPa. What is the most appropriate next step in management?
Correct Answer : A
This question is testing your knowledge of the management of acute exacerbation of COPD. The reason that this is likely COPD instead of asthma is because of his age, the fact that he is a smoker, and the choice of administering 24% oxygen rather than 100% oxygen.
24% of oxygen gives a clue that he is on controlled O2 therapy with an attempt to maintain saturations between 88% and 92% to balance hypoxia, hypercapnia, and pH which is seen as part of the management for COPD.
Non-invasive ventilation would be the next step in management as it is particularly effective in supporting patients during an exacerbation especially when maximal medical treatment has not been effective like in this case. Its use is appropriate for conscious patients with ongoing respiratory acidosis (< pH 7.35).
Oral antibiotics should ONLY be given if there is purulent sputum or clinical signs of pneumonia. While it is common practice for all patients with an exacerbation of COPD to receive antibiotics in the hospital, it is not according to guidelines, and for this exam, antibiotics should not be administered to manage acute exacerbation of COPD unless we suspect pneumonia.
The reason why invasive mechanical ventilation is an inappropriate answer is that it has its complications such as pneumonia, barotrauma, and failure to wean to spontaneous ventilation. Thus, it should not be used unless non-invasive ventilation fails or is contraindicated such as in scenarios like respiratory arrest, high aspiration risk, or impaired mental status.
Doxapram is also an incorrect answer. Doxapram is a respiratory stimulant. It is given intravenously and can be used to drive respiratory rate if the respiratory rate is less than 20 breaths/minute. In this case, the respiratory rate is 32 breaths/minute hence there is no problem with the respiratory drive.
Management of acute exacerbation of COPD :
- Antibiotics if sputum is purulent or clinical signs of pneumonia
- Prednisolone 30mg/day for 7-14 days
- Inhaled or nebulized bronchodilators
- Controlled O2 therapy 24% via Venturi face mask, with oximetry.
- Maintain saturations between 88% and 92%
- IV aminophylline. Beneficial if the patient is wheezy and has not improved with nebulizers alone
- Non-invasive ventilation. Effective in supporting patients during an exacerbation when maximal medical treatment is not effective.
Q.7. A 27 year old man presents with chest pain and respiratory distress following a road traffic accident. On examination, his neck veins are noted to be distended and trachea is deviated to right. Breath sounds are absent on the left and diminished on the right lung field. He has a blood pressure of 80/40 mmHg and a heart rate of 120 beats/minute. What is the most appropriate next action?
Correct Answer : B
The features described are diagnostic of left-sided tension pneumothorax.
Presentation :
- Acute respiratory distress
- Hypotension
- Raised jugular venous pressure
- Tracheal deviation away from the pneumothorax side
- Reduced air entry on the affected side
Management of a tension pneumothorax -
- If strong clinical suspicion, give high-flow oxygen and insert a large bore cannula into second intercostal space in the midclavicular line on the side of the pneumothorax.
- Do not wait for a chest X-ray if the patient is seriously compromised or has a cardiac arrest has occurred or if the diagnosis is clinically certain
- Hiss of escaping air confirms the diagnosis
- Air should be aspirated until the patient is less distressed. Then insert a chest drain in the mid-axillary line, leaving the cannula in place until you have finished and the underwater seal is bubbling satisfactorily.
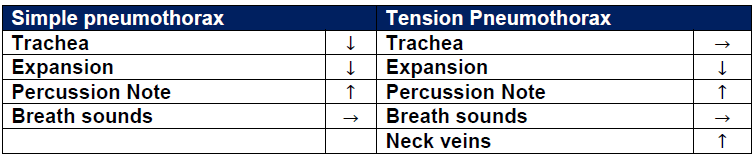
PNEUMOTHORAX TYPES -
Primary spontaneous pneumothorax : Occurs without an apparent cause
Secondary spontaneous pneumothorax : Occurs in the presence of existing lung pathology e.g. COPD
Simple pneumothorax : Non-expanding collection of air around the lung
Tension pneumothorax : Expanding the collection of air around the lung.
Think of tension pneumothorax as a “one-way valve” where air is allowed to enter around the lung but cannot escape it. Although this is not entirely true because air can still escape a little, hopefully, this analogy gives you the idea of a tension pneumothorax.
Q.8. A 20 year old man suddenly develops shortness of breath over the last day. It started when he was playing football. The shortness of breath was associated with right sided pleuritic chest pain. On examination, reduced air entry with hyper-resonance was noted over the right lung field. His oxygen saturation was 91% on room air. What is the most likely diagnosis?
Correct Answer : C
Dyspnoea and chest pain in a young man are features of primary spontaneous pneumothorax. This occurs when a subpleural bullous ruptures.
One of the major differences between spontaneous pneumothorax from tension pneumothorax is that the patient does not have a deviated trachea away from the affected side.
Primary spontaneous pneumothorax occur most commonly in tall thin men aged between 20 and 40. They usually occur in the healthy. Cigarette is a major risk factor for pneumothorax.
The mechanism is unclear; a smoking-induced influx of inflammatory cells may both break down elastic lung fibers (causing formation) and cause small airway obstruction (increasing alveolar pressure and the likelihood of interstitial air leak)
- More common on the right side
- Less than 10% of cases are bilateral
- Usually caused by rupture of small subpleural blebs (collections of air < 2cm)
Presentation :
- Dyspnoea, chest pain, cough, tachypnoea
- Ipsilateral decreased chest wall movement, hyper resonant hemithorax to percussion.
Q.9. A 33 year old man is brought into the emergency department following a road traffic accident. He is seen to be very short of breath. He has no breath sounds over the right side of his chest. On percussion, the right chest is noted to be hyper-resonant. On examination, his trachea is deviated to the left. His heart rate is 120 beats/minute. His blood pressure is 90/65 mmHg, and has an oxygen saturation of 85% on 15 L of oxygen. What is the most appropriate course of action?
Correct Answer : C
This man has rapidly developed the signs of a pneumothorax. Needle decompression needs to be immediately done using a large bore cannula into the second intercostal space at the midclavicular line just above the third rib to avoid the neurovascular bundle. As the needle is withdrawn, a hiss will be heard as the lung decompresses. Air should be removed until the patient is no longer compromised. This is usually followed by an axillary drain.
The other less appropriate answers: Investigations like ABG and chest X-ray - should be deferred as this is a serious situation that would lead to cardiorespiratory arrest unless addressed. Insertion of a chest drain will be needed but not until the air has been removed and the lung decompressed.
Insertion of a cannula into the left second intercostal space. A wrong answer as the trachea is deviated towards the left. This means that the tension pneumothorax is on the right.
Q.10. A 50 year old woman returned by air to Dubai from UK. 3 days later, she presents with a sharp chest pain and breathlessness. Her chest X-ray and ECG are normal. What is the most appropriate investigation?
Correct Answer : D
A prolonged plane journey is a recognized risk factor for thromboembolism and hence pulmonary embolism as well. Sharp chest pain and breathlessness after 3 days of plane journey are highly suggestive of pulmonary embolism. CTPA is the answer here as it is the best test among the other options that provide a definitive diagnosis of pulmonary embolism.
Q.11. A 49 year old man was admitted 5 days ago with fever, poor oral intake, cough and shortness of breath. His medical history includes a recent renal transplant which he has been on immunosuppressants. A chest X-ray during admission demonstrates streaky and fibrotic lesions in both lungs. As his symptoms worsened, the respiratory team performed a diagnostic bronchoscopy with bronchoalveolar lavage which results demonstrate pneumocystis jiroveci cysts. What is the most appropriate antibiotic to prescribe?
Correct Answer : A
The first line treatment for pneumocystis jiroveci is co-trimoxazole (trimethoprim/sulfamethoxazole). This can be given by mouth or intravenously. Atovaquone is a second-line agent, although it is used only for mild-to-moderate pneumocystis jiroveci.
PNEUMOCYSTIS CARINII PNEUMONIA (PCP) (PNEUMOCYSTIS JIROVECI PNEUMONIA) :
Whilst the organism Pneumocystis carinii is now referred to as Pneumocystis jiroveci, the term Pneumocystis carinii pneumonia (PCP) is still in common use. Pneumocystis pneumonia (PCP) is a major cause of morbidity and mortality among immunocompromised people.
It remains a leading AIDS-defining opportunistic infection in HIV-infected individuals. HIV infection is a particularly important risk factor especially if the CD4 count is < 200/mm³ thus all patients with a CD4 count < 200 should receive PCP prophylaxis.
Features :
- Exertional dyspnoea
- Gradual onset of dry cough
- Fever
- Tachypnoea
- Chest pain or retrosternal tightness
- May be signs of AIDS e.g. Thrush
- Chest examination is typically normal
Think of flu-like symptoms in an immunocompromised patient. Desaturation on exercise may suggest the diagnosis in individuals at risk of PCP with normal saturations at rest. This is pathognomonic for PCP so in the outpatient setting, it is good practice to monitor oxygenation by pulse oximetry after walking in patients you suspect having PCP.
Remember, there are so many causes of pneumonia. The question writers would have to give you some sort of clue if they would want you to pick PCP. The two major clues that they can give are an HIV patient and desaturation on exercise.
Investigation - Sputum often fails to show PCP, bronchoalveolar lavage may be needed to demonstrate PCP.
Bronchoscopy with bronchoalveolar lavage is the diagnostic investigation of choice in non-HIV-infected patients and in patients with HIV in whom induced sputum analysis is non-diagnostic.
Management - Co-trimoxazole (trimethoprim-sulfa) remains the first-line treatment.
Q.12. A 56 year old lady with lung cancer presents with urinary retention, postural hypotension, diminished reflexes and sluggish pupillary reaction. What is the most likely explanation for her symptoms?
Correct Answer : C
These features are well-known features of autonomic neuropathy which can be a result of paraneoplastic syndrome. Paraneoplastic syndromes are rare and believed to occur when cancer-fighting antibodies (white blood cells) mistakenly attack normal cells in the nervous system.
When one of these syndromes is associated with lung cancer, it is often with small cell lung cancer or because the cancer has metastasized to a particular part of the body.
Autoimmune paraneoplastic autonomic neuropathy is a rare paraneoplastic syndrome (PNS), which manifests as a disturbance in sympathetic and/or parasympathetic nervous system function.
Q.13. A 45 year old chronic smoker attends the outpatient department with complaints of persistent cough and copious amount of purulent sputum. He had history of measles in the past. On examination, finger clubbing is noted and inspiratory crepitations on auscultation is heard. A chest X-ray shows tram track opacies. What is the most likely diagnosis?
Correct Answer : B
The history of smoking here is irrelevant as smoking does not appear to be an independent risk factor but smoking cessation is important as part of the management if the patient does smoke. The persistent cough and copious amount of purulent sputum are symptoms of bronchiectasis.
Measles is a childhood viral infection that is one of the aetiologies of bronchiectasis. Finger clubbing is not a specific sign but has been seen in bronchiectasis although not very frequently. Inspiratory crepitations and a chest-x ray that shows tram lines give a more specific picture pointing towards bronchiectasis.
Although these are not diagnostic, the most probable diagnosis among the others is bronchiectasis. Only a high-resolution computed tomography (HRCT) chest would give you the diagnosis of bronchiectasis. Bronchiectasis Is the irreversible abnormal dilatation of small and medium-sized bronchi, with chronic airway inflammation.
It is associated with chronic sputum production, chronic cough, recurrent acute chest infections, and airflow obstruction.
. Bronchiectasis may progress to respiratory failure and corpulmonale;
- Coarse crackles are the most common finding, heard in early inspiration and often in the lower zones
- Large airway rhonchi (low-pitched snore-like sounds)
Wheeze may be present - Clubbing is found infrequently
Diagnosis :
- Usually made clinically, with high-resolution computed tomography (HRCT) chest for confirmation.
- A baseline chest x-ray should be done in all patients. Early chest X-ray findings may be normal in patients with bronchiectasis.
Chest X-rays in advanced cases may show 1 to 2-cm cysts, crowding of the bronchi (tramlines), or ring opacities.
The main value of a CXR excludes other causes of symptoms.
Treatment - Damaged lungs cannot be repaired so the basis of management is to prevent or at least slow down further deterioration.
- Bronchodilators, chest physical therapy, and postural drainage are used to control and improve drainage of bronchial secretions
- If the patient smokes this must be stopped
- Immunisation against influenza and pneumococcus
- Long-term oral antibiotics for patients having three or more exacerbations per year requiring antibiotic therapy or patients with fewer exacerbations that are causing significant morbidity should be considered for long-term antibiotics.
- Choice will be dictated by sensitivities and local microbiology advice from sputum test results.
Q.14. A 48 year old presents with increasing shortness of breath over the last few months and a dry cough. He has worked in coal mines for 18 years. Chest x-ray and CT scan of the chest demonstrate characteristic upper zone mass-like scarring with calcification and volume loss. The lung opacifications are seen to be associated with radiating strands. What is the most likely diagnosis?
Correct Answer : D
The first step to recognition of the answer is to understand that with a history of working in coal mines, this is likely a Coal worker’s pneumoconiosis.
Progressive massive fibrosis refers to the formation of large conglomerate masses of dense fibrosis, predominantly in the upper pulmonary lobes. These classically develop in the context of certain pneumoconioses (especially Coal worker's pneumoconiosis and silicosis).
Q.15. A 10 year old girl with diagnosed asthma is having frequent coughs and wheezing that wakes her up at night. She is compliant with her asthma medications which consist of a short-acting B2 agonist inhaler as required, inhaled corticosteroid 400 mcg/day and a long-acting B2 agonist inhaler. Her inhaler technique is good. What is the most appropriate next step in management?
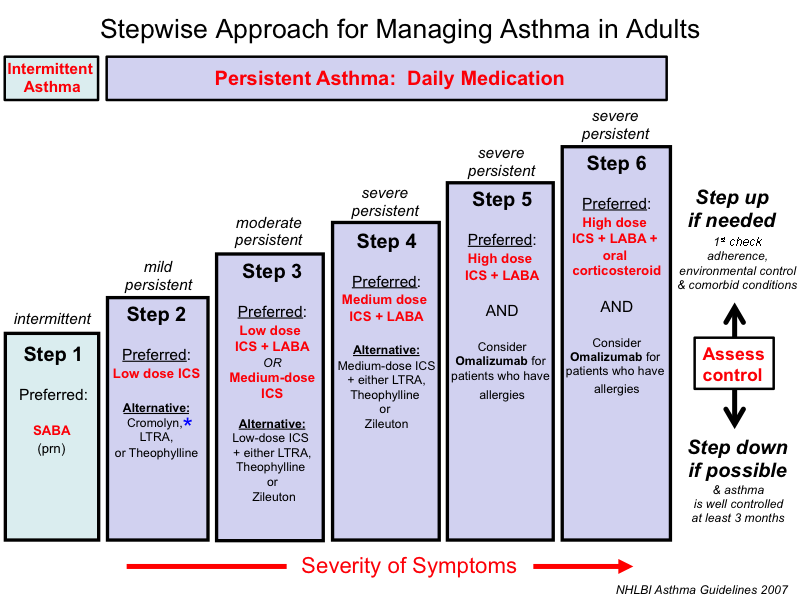
Correct Answer : A
The answer here is to increase the dose of ICS. The patient is considered to be at step 4 of the BTS guideline which recommends increasing the ICS dose to 800 mcg/day or considering a trial of Theophylline. Be mindful that children and adult recommendations are different.
Asthma is characterized by paroxysmal and reversible obstruction of the airways.
Stepwise approach if asthma remains : AGE - 5 To 16
Step 1 - Inhaled short-acting B2 agonist (SABA)as required.
Step 2 - Add pediatric low-dose inhaled corticosteroid (ICS) up to 200 mcg/day.
Step 3 - Add leukotriene receptor antagonist (LTRA), Review response in 4-8 weeks.
Step 4 - Stop LTRA and start inhaled long-acting B2 agonist (LABA) in combination with paediatric low-dose inhaled corticosteroid.
Step 5 - Stop LABA and ICS and start the MART* regimen with a paediatric low-dose ICS.
Step 6 - Increase to paediatric moderate maintenance dose ICS (either continuing MART or changing to fixed-dose ICS + LABA and SABA as a reliever)
Step 7 - Refer to a respiratory physician for further escalation.
Q.16. A 27 year old male is admitted with acute exacerbation of asthma. He is treated intiated with 100% oxygen and salbutamol nebulizers. Intravenos hydrocortisone was prescribed but it was not available in the department. He has a respiratory rate of 21 breaths/minute, a heart rate of 90 beats/minute and an oxygen saturation of 92%. What is the most appropriate next step in management?
Correct Answer : A
Oral prednisolone and intravenous hydrocortisone have been shown to have similar efficacy. The only benefit of intravenous hydrocortisone compared to oral prednisolone for asthma is for those patients who are vomiting or having severe dyspnoea where they cannot consume oral medication.
ASTHMA – MANAGEMENT OF ACUTE EXACERBATION IN ADULTS
Immediate treatment:
• Start O2 if saturations < 92%, aim sats 94-98%
• Salbutamol 5 mg (or terbutaline 10 mg) nebulized with O2
• Hydrocortisone 100 mg IV or prednisolone 40-50 mg PO
If life-threatening features are present:
• Give salbutamol nebulizers every 15 minutes, or 10 mg continuously
• Add ipratropium 0.5 mg to nebulizers
• Give a single dose of magnesium sulphate (MgSO4) 1.2-2 g IV over 20 minutes If improving within 15-30 minutes
• Nebulized salbutamol every 4 hours
• Prednisolone 40-50 mg PO OD for 5-7 days.
Q.17. A 50 year old chronic smoker attended the outpatient department with complaints of chronic productive cough, dyspnoea and wheeze. A chest X-ray was ordered and reported as hyperinflated lung with flattened hemidiaphragm and a small cardiac silhouette. Full blood count shows an increase in haematocrit. What is the most likely diagnosis?
Correct Answer : C
The findings are in going with COPD. Haematocit can be raised in COPD. Chest X-ray is not required for diagnosis of COPD, and repeated CXR is unnecessary, unless other diagnosis are being considered (most importantly, lung cancer or bronchiectasis).
If a chest X-ray is ordered, these are the findings:
- Hyperinflated lung fields
- > 7 posterior ribs seen
- Flattened diaphragms
- Small heart
- May see bullae
Q.18. A 29 year old woman has been short of breath for the last 15 hours and is feeling unwell. An arterial blood gas is taken: PaO2 8.8 kPa PaCO2 3.2 kPa pH 7.50 Bicarbonate (HCO3-) 20 mmol/L Normal Values: PaO2 > 10 kPa PaCO2 4.7-6 kPa pH 7.35 – 7.45 Bicarbonate (HCO3-) 22-26 mmol/L. What is the most likely diagnosis?
Correct Answer : D
This woman has become acutely breathless from a pulmonary emboli. She is hypoxic and, as a reflex to this, is hyperventilating (as evidenced by the low PaCO2). As a result, she has developed an alkalosis. The other options are much less likely to be the answer:
Diabetic ketoacidosis and methanol overdose - both cause acidosis. The scenario that was given is alkalosis.
Panic attacks - This does cause acute alkalosis via hyperventilation but tends to happen in the absence of hypoxia rather than as a response to it (as in pulmonary embolism).
Severe vomiting - Causes a metabolic alkalosis (i.e. a high pH with a high HCO3–), PaO2 is not likely to decrease.
METABOLIC ACIDOSIS:
• Excess production of Organic Acids
• Ketoacidosis
• Alcoholic
• Violent convulsions
• Excessive ingestion of Toxins
• Aspirin
• Methanol Alcohol
• Excess loss of HCO3
• Diarrhoea
• Addison’s disease
• Retention of Organic Acids
• Renal insufficiency of Any Cause
METABOLIC ALKALOSIS:
• HCl loss
• Vomiting
• Excessive Administration of HCO3
• Hypokalaemia
• Hypovolaemia
• Increased Renal Excretion of Acid
• Diuretic therapy
• Secondary Hypoparathyroidism.
RESPIRATORY ACIDOSIS:
• Airway obstruction
• Aspiration
• COPD
• Respiratory center depression
• Circulatory collapse
• Cardiac arrest
• Pulmonary oedema
• Neurogenic causes
• Cervical spine injury
• Drugs (paralytic agents, organophosphates)
• Multiple sclerosis
• Restrictive effects
• Haemothorax
ALKALOSIS: (Any event causing hyperventilation)
• Lung disease
• Pulmonary embolism
• CNS-Respiratory stimulation
• Cerebral Vascular Accident (Stroke)
• Anxiety - Hyperventilation syndrome
• Salicylate Intoxication
• Congestive cardiac failure
• Mechanical ventilation
Q.19. A 79 year old man with longstanding chronic obstructive pulmonary disease has become progressively breathless over the last 2 years. His medications for his COPD include salbutamol and salmeterol inhalers, inhaled corticosteroids and theophylline. His forced expiratory volume in one-second (FEV1) is less than 30%. His oxygen saturations are 89% onroom air. What is the next appropriate management?
Correct Answer : D
COPD is the disease for which long-term oxygen therapy (LTOT) is most commonly prescribed. There is strong evidence of the survival benefit of long-term oxygen therapy (LTOT) in patients with COPD and severe chronic hypoxaemia when used for at least 15 hours daily. Once LTOT is started, it is likely to be lifelong.
Q.20. A 25 year old tall man presents to A&E with increasing dyspnoea and right sided chest pain. He has been a heavy smoker for the past 4 years. He has not past medical history. What is the most likey diagnosis?
Correct Answer : B
Dyspnoea and chest pain in a young tall man with no past medical history could only be primary spontaneous pneumothorax. The giveaway here is the word “tall”.
Primary spontaneous pneumothorax occur most commonly in tall thin men aged between 20 and 40. They usually occur in the healthy. Cigarette is a major risk factor for pneumothorax.
Presentation :
- Dyspnoea, chest pain, cough, tachypnoea
- Ipsilateral decreased chest wall movement, hyperresonant hemithorax to percussion
Diagnosis : Chest X-ray is the diagnostic test in most cases, revealing a visible lung edge and absent lung markings peripherally.
Q.21. A 34 year old HIV positive man presents to the outpatient clinic with fever, dry cough and shortness of breath. He is tachypnoeic but his chest is clear. Oxygen saturation is normal at rest but drops on walking. What is the most likely diagnosis?
Correct Answer : C
There are so many cases of pneumonia so the stem would have to give you some sort of clue to pick pneumocystis carinii pneumonia (PCP). The two major clues that are seen here are an HIV patient and desaturation on exercise which is pathognomic for PCP.
Q.22. A 10 year old girl is brought to the emergency department by her dad after having fallen in the park. Her elbows are full of cuts and she has not stopped crying since the injury. Her medical history includes asthma. What is the most appropriate analgesia to administer?
Correct Answer : D
Symptoms of asthma may present after taking aspirin, NSAIDs, or beta-blockers. Thus, NSAIDs like ibuprofen and diclofenac should not be used here. The association between non-steroidal anti-inflammatory drugs (NSAIDs), including aspirin, and the precipitation of asthma is well documented but, in reality, it is not often seen.
So in clinical practice, one may use NSAIDs even if the patient has asthma, but for exam, never give NSAIDs if the patient has asthma.
Codeine should only be used to relieve acute moderate pain in children older than 12 years and only if it cannot be relieved by other painkillers such as paracetamol or ibuprofen alone. Since the child here is under 12, co-codamol should not be used.
Paracetamol is the only available choice.
Q.23. A 68 year old smoker has left sided chest pain which worsens when taking deep breaths. His medical history includes diabetes mellitus and hypertension. On examination, he has a miotic left eye and partial ptosis on the left. There is also wasting of small muscles of the left hand. What is the most likely diagnosis?
Correct Answer : B
The likely diagnosis here is a pancoast tumour which is a type of lung cancer defined primarily by its location situated at the top end of the right or left lung. In this case, it would be the left lung. This would explain the chest pain firstly and also the miosis and ptosis which are part of Horner’s syndrome.
Pancoast tumour :
- A tumour of the pulmonary apex
- It is a type of lung cancer defined primarily by its location situated at the top end of either the right or left lung
Presentation :
- Ipsilateral invasion of the cervical sympathetic plexus leads to Horner's syndrome (ptosis, anhidrosis, miosis)
- Brachial plexus invasion can lead to wasting of the intrinsic hand muscles and paraesthesia in the medial side of the arm along with shoulder and arm pain
Mnemonic for Horner’s syndrome :
P *Ptosis (drooping of the eyelid)
A *Anhidrosis (lack of sweating)
M *Miosis (constriction of the pupils)
E *Enophthalmos (sunken eyeball).
Q.24. A 35 year old lady had an emergency C-section following an ultrasound labour. Three days post-operation she develops a sudden onset of left sided chest pain associated with breathlessness. Her heart rate is 105 beats/minute. Her left leg is swollen and has pain on palpation. What is the best investigation to provide a definitive diagnosis?
Correct Answer : A
CTPA is the answer here as it is the best test among the other options that provide a definitive diagnosis of pulmonary embolism.
Q.25. A 23 year old woman who is on several medications and inhalers for her asthma presents to the hospital with palpitations. Her heart rate is 110 beats/minute. Her peak expiratory flow rate is 400 L/minute. What is the most appropriate management?
Correct Answer : B
One of the common side effects of beta-agonists is palpitations and tachycardia. Both of which are seen here. Reviewing the medications would be appropriate.
Q.26. A 21 year old lady who smokes has a history of wheezing, chest tightness and coughing at night. She also notices these symptomsoccur when she goes out in the cold and breathes cold air. What is the most likely diagnosis?
Correct Answer : A
Please see Q-1
Q.27. A 45 year old man has been having a productive cough for the past 3 weeks. He has been having a fever since then. He has not gone to work for the past 2 weeks as he feels too unwell. He presents to the hospital with chest pain and shortness of breath. On auscultation, there is decreased breath sounds on the right upper lobe with crackles. Percussion is dull in the same area. He has a temperature of 39 C, a respiratory rate of 28 breaths/minute and a pulse rate of 110 beats/minute. His blood results are as follows: Haemoglobin 129 g/L White cell count 15 x 109/L Platelets 450 x 109/L CRP 110 mg/L. What is the most likely diagnosis?
Correct Answer : C
The blood results are consistent with an infection. Lobar pneumonia is more common than pleural empyema although pneumonia may later develop into a pleural empyema.
Empyema describes pus in a cavity. Pleural empyema describes pus in the pleural space. It starts with pneumonia that is complicated by an inflammatory response leading to parapneumonic effusion. When secondary infection of this effusion occurs, it produces an empyema.
Pneumonia and empyema share similar clinical features however symptoms of empyema usually include swinging fevers, night sweats, weight loss, and chest pain. One should suspect pleural empyema if pneumonia does not improve with antibiotics.
Dullness to percussion, crackles on auscultation, and decreased breath sounds are features of lung consolidation from pneumonia and can also be seen once an empyema develops so they are not a useful discriminating physical finding.
Q.28. A 35 year olf man presented to the Accident and Emergency department with a productive cough and fever. A chest X-ray demonstrated right lower zone pneumonia. His CURB-65 score was 1 and he discharged with oral antibiotics. 5 days later he presents with ongoing fever (38.9 C) and pleuritic chest pain. On examination there is reduced breath sounds at the right base with crepitations. A repeat chest x-raydemonstrates a new right sided pleural effusion. What is the most important investigations to perform?
Correct Answer : B
Pleural aspiration is required to rule out an empyema – a collection of pus within the pleural cavity. It is a complication of pneumonia, as well as invasive procedures of the thorax. If an empyema is confirmed (pH of the pleural aspirate < 7.2) or the effusion is causing respiratory compromise then a chest drain should be inserted. The aspirate should be sent for microscopy and culture Blood and sputum cultures should also be repeated, however, these are not the most important investigations.
The patient will be managed as an inpatient and treated with intravenous antibiotics. Note an HIV test should be requested. The CURB-65 score has also been mentioned in this question.
It is worth knowing that the score is a predictor of 30-day mortality for community-acquired pneumonia and ranges from a score of 0 to 5.
CURB 65 :
C onfusion
U rea (> 7 mmol/L)
R espiratory rate (30 bpm)
B lood Pressure ( SBP < 90mm Hg, DBP < 60 mm Hg)
> 65 years.
Scores of 0-2 can be managed as an outpatient if the patient is well.
Q.29. A 56 year old man who has a history of hypertension and asthma recently had a change of medication which was prescribed by his GP. 2 days after starting the new medication, he develops wheezing and shortness of breath. What is the most likely medication that would have caused this?
Correct Answer : D
Symptoms of asthma may present after taking aspirin, NSAIDs, or beta-blockers.
Q.30. A 29 year old HIV positive man attends the outpatient department with complaints of persistent cough and copious amount of purulent sputum. He also has dyspnoea and chest pain. On auscultation, inspiratory crepitations are heard at the base of the lung. A chest X-ray shows tram track opacities. What is the most likely diagnosis?
Correct Answer : B
The persistent cough and copious amount of purulent sputum are symptoms of bronchiectasis. HIV is one of the aetiologies of bronchiectasis. Inspiratory crepitations and a chest-x ray that shows tramlines give a more specific picture pointing towards bronchiectasis. Although these are not diagnostic, the most probable diagnosis among the others is bronchiectasis.
Only a high-resolution computed tomography (HRCT) chest would give you the diagnosis of bronchiectasis.
Q.31. A 62 year old man has been smoking 15 cigarettes a day for the past 40 years. He is a retired builder and has been working since he was 24 years old. He presents with chest pain, shortness of breath, and has lost significant weight over the last couple of years. Chest X-ray shows bilateral fibrosis and left sided pleural effusion. What is the best investigations that will lead to diagnosis?
Correct Answer : C
Histology is the most appropriate way to diagnose mesothelioma. The history of working as a builder is the question writer's way of hinting at asbestos exposure. The association with smoking greatly increases the possibility of developing mesothelioma. The best investigation is a pleural biopsy.
Malignant mesothelioma is a tumour of mesothelial cells that usually occurs in the pleura, and rarely in the peritoneum or other organs. It is associated with occupational exposure to asbestos.
Q.32. A 68 year old man has malaise and cough for 5 days. He has a temperature of 38.5 C. There is dullness on percussion of the left lung base. What is the most appropriate investigation?
Correct Answer : C
The given presentation is suggestive of pneumonia for which the most appropriate investigation is a Chest X-ray.
Q.33. A 62 year old man who used to work in the shipyard industry presented to the hospital with gradual increase in shortness of breath, chest pain and weight loss. He has been feeling fatigued and having a mild fever for the past few weeks. On examination, finger clubbing and a palpable chest wall mass was noted. A computed tomography was performed which showed patchy infiltrates, pleural thickening and pleural effusion. He died 7 days later. What is the most appropriate management to deal with this patient’s death certificate?
Correct Answer : C
This patient had probably died from mesothelioma. Mesothelioma is classed as an industrial disease. All deaths from mesothelioma must be referred to the local coroner’s office.
The coroner will then decide if a post-mortem examination is required and will hold an inquest. An inquest is a legal investigation to establish the circumstances surrounding a person’s occupational disease and one needs to determine whether the death was due to mesothelioma or some other cause.
The coroner will give the final verdict and issue the final death certificate.
Remember: If someone has died of a disease that might be related to asbestosis this could be an ‘unnatural death’ so an investigation or ‘inquest’ will be needed.
Q.34. A 33 year old chronic smoker attends the outpatient department with complaints of persistent cough, copious amount of purulent sputum and dyspnoea. He has a history of recurent chest infections in the past. Coarse crackles are found at the base of his lung on auscultation. Bronchiectasis is suspected. What is the most definitive test to diagnose bronchiectasis?
Correct Answer : D
The gold standard for diagnosis is HRCT of the chest.
HRCT has a very high sensitivity and specificity for diagnosis and has now replaced bronchography.
In adults, bronchoscopy and bronchoscopic sampling of the lower respiratory tract do not have a place in the routine investigation of patients with bronchiectasis.
Bronchoscopy is used for patients in whom serial testing of sputum does not yield microbiological information and who are not responding well to treatment or if HRCT suggests atypical mycobacterial infection and sputum culture is negative.
Q.35. A 65 year old retired builder complains of persistent dull chest pain and shortness of breath. He is a smoker and started smoking since a young age. He looks thin and his clothes are oversized. Finger clubbing is noted on examination. What is the most likely diagnosis?
Correct Answer : D
The history that he is a builder is the question writer's way to hint that this patient had asbestos exposure in the past. Asbestos exposure is a well-established cause of mesothelioma, with occupational exposure being documented in 70-80% of those affected.
Finger clubbing is usually caused by underlying asbestosis. Although finger clubbing is commonly seen in questions with mesothelioma, it is very rare in clinical practice. Finger clubbing is seen in less than 1% of patients with mesothelioma.
Q.36. A 38 year old woman is brought to the A&E after falling down the stairs and injuring her rib. She complains of shortness of breath. A chest X-ray was perforemd to rule out a rib fracture. Bilateral hilar lymphadenopathy was seen on the chest X-ray. On auscultation, there are vesicular breath sounds. On examination, there are red lesions on both her shins which are tender. What is the most likely diagnosis?
Correct Answer : A
In exam, whenever you see the term “bilateral hilar lymphadenopathy” with a lesion on the shin, you should be thinking of Sarcoidosis. The lesion on the shin is erythema nodosum which are blue or red lesions and are seen in people suffering from sarcoidosis.
The syndrome here is Lofgren syndrome which includes erythema nodosum, arthritis, and hilar adenopathy.
Lofgren is a distinct sarcoid syndrome.
SARCOIDOSIS :
Sarcoidosis is a systemic disease of unknown cause, characterized histologically by the presence of nonspecific noncaseating granulomas in the lung and other organs.
Presentation :
- Up to 50% are asymptomatic (Chest X-ray for another indication reveals the diagnosis from hilar lymphadenopathy)
- Involves almost any organ system, but pulmonary involvement is most common (around 90% of symptomatic patients)
- Fatigue
- Erythema nodosum
- Bilateral hilar Lymphadenopathy
- Polyarthralgia
- Uveitis
- Renal Stones
• Lofgren syndrome includes : Erythema nodosum, Arthritis, Hilar adenopathy
Investigations :
• Chest X-ray shows bilateral hilar adenopathy
• Elevation in angiotensin-converting enzyme (ACE) can be seen in 60% of patients with sarcoidosis.
• Definitive diagnosis is by biopsy of suspected tissue which shows noncaseating granulomas. This can be from the skin, lymph nodes, conjunctiva, or lung.
Treatment : Generally in the setting of organ impairment, a trial of steroids may be used.
Q.37. A 17 year old boy with a history of asthma suddenly develops chest pain and increasing breathlessness during a game of football. He has reduced breath sounds on the right side. His oxygen saturation is 94% on air. What is the most appropriate investigation?
Correct Answer : A
Do not forget that acute severe asthma may have an underlying pneumothorax. Dyspnoea and chest pain in a young man are features of primary spontaneous pneumothorax. A standard erect CXRs in inspiration are recommended for the initial diagnosis of pneumothorax.
Q.38. A 74 year old man who has been a smoker since he was 20 has recently been diagnosed with small cell lung cancer. What is the most likely serum electrolyte picture that confirms the presence of syndrome of inappropriate antidiuretic hormone secretion (SIADH)?
Correct Answer : B
SIADH :
The diagnosis requires concentrated urine (Na+ > 20mmol/L and osmolality > 100mosmol/kg) in the presence of hyponatraemia (plasma Na+ < 125mmol/L) and low plasma osmolality (< 260mosmol/kg), in the absence of hypovolaemia, oedema, or diuretics.
One of the causes is small-cell lung cancer.
Treatment : Treat the cause and restrict fluid. Consider salt ± loop diuretic if severe.
Vasopressin receptor antagonists (‘vaptans’) are an emerging class of drugs used in SIADH and other types of hyponatraemia.
Q.39. A 24 year old male is admitted with acute exacerbation of asthma. He is treated intiated with 100% oxygen. He continues to deteriorate. What is the most appropriate next step in management?
Correct Answer : D
The next step is to give salbutamol nebulizers. Magnesium sulphate is also used in the management of acute exacerbation but it is used further down the line.
Q.40. A 50 year old woman presents to Accident & Emergency with the complaint of shortness of breath and a dry cough which started a day ago. This was preceded by four days of experiencing flu-like symptoms. Further questioning reveals that she recently attended a conference in the United States for five days where she stayed in the hotel that was provided for attendees. A chest X-ray was done which shows pulmonary infiltrates. The patient’s vitals are noted as follows: Temperature 39.1 C Respiratory rate 21 breaths per minute Blood pressure 100/57 mmHg Heart rate 90 beats/minute Blood tests were done and the results are as follows: Haemoglobin 139 g/L (130-180 g/L) White cell count 2.34 x 109/L (4-11 x 109/L) Sodium 126 mmol/L (135-145 mmol/L) Potassium 4.1 mmol/L (3.5-5.0 mmol/L) Urea 3.9 mmol/L (2.5-6.7 mmol/L). What is the best treatment option for this patient?
Correct Answer : D
This patient’s history of staying in a hotel is very suggestive of a legionella infection. Other clues towards legionella seen here are hyponatraemia and lymphocytopenia.
It is worth remembering that Legionella infections have specific blood results:
• Hyponatraemia
• Lymphocytopenia
• Hypoalbuminaemia
• Elevated liver enzymes
Treatment of legionella : Erythromycin or azithromycin are usually the choice.
Q.41. A 54 year old patient 7 days after a total hip replacement presents with acute onset breathlessness, and chest pain. On examination, an elevated jugular venous pressure was observed. Her right calf looks swollen. Her pulse rate is 95 bpm and respiratory rate is 24/min. Which investigations will be most helpful in leading to a diagnosis?
Correct Answer : B
Please see Q-10
Q.42. A 65 year old known case of hepatocellular carcinoma with lung and bone metastasis presents with shortness of breath, gastric reflux and bloatedness. The symptoms have been on going for the past week. He is on the palliative care register and takes regular morphine for the pain. A recent DEXA scan shows his bones to be osteoporotic. On examination, there are crackles in the base of the left lung. He has a temperature of 38.1 C. A chest X-ray was performed which shows basal consolidations on the left lung. What is the most appropriate medication to administer?
Correct Answer : B
In reality, he would be started on all of them. But for the purpose of exam, if you were to choose among the answers provided, IV antibiotics would be the most important one to start as this patient has pneumonia and this should be treated first.
Q.43. A 19 year old man has a history of exercise induced asthma which has previously been controlled using a salbutamol inhaler as required. He is taking beclomethasone inhaler regularly but he now gets asthma attacks with exercise. What is the most appropriate action?
Correct Answer : D
Sodium cromoglycate can be added for exercise-induced asthma.
Exercise-induced asthma although following the stepwise approach has a slight difference in management. For most patients, exercise-induced asthma is an illustration of poorly controlled asthma, and regular treatment including inhaled corticosteroids should therefore be reviewed.
If exercise is a specific problem in patients already taking inhaled corticosteroids who are otherwise well-controlled, consider adding either:
- leukotriene receptor antagonist
- a long-acting beta 2 agonist
- an oral beta 2 agonist
- theophylline
An inhaled short-acting beta 2 agonist used immediately before exercise is the drug of choice.
Q.44. A 33 year old man has a temperature of 38.5 C, productive cough and chest pain on the right side on inspiration. He has a blood pressure of 100/60 mmHg and a pulse rate of 108 beats/minute. He appears slightly short of breath and has an oxygen saturation of 94% on room air. What is the most likely organism causing the patient’s symptoms?
Correct Answer : A
Streptococci pneumoniae (pneumococcus) is the most common cause of community-acquired pneumonia. It is a gram +ve cocci.
Q.45. A 48 year old farmer presents with malaise, dry cough, chest tightness and shortness of breath. The shortness of breath and cough started only a few hours ago. On auscultation, a wheeze is heard throughout the chest. He has a temperature of 39.2 C, a pulse of 96 beats/minute, a blood pressure oef 110/70 mmHg and a respiratory rate of 29 breaths/minute. His chest X-ray shows diffuse micronodular interstitial shadowing. What is the most appropriate diagnosis?
Correct Answer : D
The signs and symptoms fit extrinsic allergic alveolitis. The occupation as a farmer is also another hint.
Chest X-ray: in the acute form may be normal in some or show diffuse micronodular interstitial shadowing like in this case.
In extrinsic allergic alveolitis, there is diffuse, granulomatous inflammation of the lung parenchyma and airways in people who have been sensitized by repeated inhalation of organic antigens in the dust (eg, from dairy or grain products, animal dander, and protein and water reservoir vaporizers).
One of the specific risk factors is occupations including farmers, cattle workers, ventilation system workers, vets, people working with grain and flour, those whose job involves working with chemicals.
There are 3 forms of extrinsic allergic alveolitis:
1. Acute
2. Subacute
3. Chronic
Q.46. A 26 year old smoker has a history of wheezing, chest tightness and breathlessness at night and early morning. Her past medical history includes eczema. What is the most likely diagnosis?
Correct Answer : C
Please see Q-1
Q.47. A 22 year old man presents with episodes of dyspnoea, starting suddenly. This usually occurs when he is in a crowded area like a lift. When he is breathless, he also notices tingling around his mouth and he feels light-headed. These episodes usually go away after a while. An arterial sample was taken for blood gases during one of the episodes. What is the most likely result of the arterial blood gas (ABG)? Normal Values: Pa02 > 10 kPa PaCO2 4.7–6 kPa pH 7.35 - 7.45 Bicarbonate (HCO3-) 22-26 mmol/L
Correct Answer : B
To understand this question, we have to go back to basics.
First, is the patient hypoxic? - the Pa02 >10 kPa is normal
Second, is the patient acidaemic (pH <7.35) or alkalaemic (pH >7.45)
Third, PaCO2 > 6.0 kPa suggests a respiratory acidosis & PaCO2 < 4.7 kPa suggests a respiratory alkalosis.
If your answer was A or D, you need to remember that panic attacks usually result in hyperventilation thus PaO2 is usually normal (Pa02 > 10 kPa). If your answer was C, you need to remember that hyperventilation which is seen in panic attacks usually results in respiratory alkalosis (pH >7.45).
If your answer was B, you need to remember that there would be no metabolic compensation as panic attacks resolve rapidly.
Q.48. A 33 year old man is referred for an X-ray as he complains of a persistent cough, chest pain and excessive purulent sputum. He has a history of recurrent chest infections. On examination, drumstick-shaped fingers were noted. What is the most likely diagnosis?
Correct Answer : D
The persistent cough and excessive purulent sputum are symptoms of bronchiectasis. Finger clubbing is not a specific sign but has been seen in bronchiectasis although not very frequently.
The most probable diagnosis among the others is bronchiectasis. Occasionally, the question would include chest-x ray findings that show tramlines. This would give a more specific picture pointing towards bronchiectasis.
Only a high-resolution computed tomography (HRCT) chest would give you the diagnosis of bronchiectasis.
Q.49. A 63 year old man has advanced COPD. He is currently unable to mobilise the way he used to a few months ago. He is on relaxation therapy for his panic and anxiety and is on chronic oxygen therapy for his breathlessness however, he still complains of being unable to breathe. What is the most appropriate agent to assist with his breathlessness?
Correct Answer : B
Regular nebulized normal saline has been shown to help loosen tenacious secretions which may reduce breathlessness.
This is a very important stem to remember and possibly can be written in many different ways with different answers. If the options included “Prednisolone” then that would be preferred over nebulized normal saline as it is frequently prescribed as part of the management for patients with acute COPD.
Q.50. A 2 year old girl presents with a 4 day history of fever which started with a cough. She has a respiratory rate of 45 breaths/minute, oxygen saturation of 94% and a temperature of 38.9 C. There are crepitations at the left base on auscultation of the lung fields. Urine dipstick was found to be negative. What is the investigation most likely to lead to diagnosis?
Correct Answer : B
This is an extremely straightforward question. The features are consistent with respiratory rate infection (possibly pneumonia) for which a chest X-ray is the investigation of choice.
Q.51. A 60 year old lady is on treatment for ischaemic heart disease, hypertension and hyperlipidaemia. During the night, she complains of wheezing and shortness of breath. What is the most likely medication that is responsible for her symptoms?
Correct Answer : C
Symptoms of asthma may present after taking aspirin, NSAIDs, or beta-blockers. Atenolol is the only beta blocker on the list.
Q.52. A 22 year old, tall thin man comes to the Emergency Department with difficulty breathing and chest pain. It developed 2 hours ago while he was driving. The onset was sudden and without any history of trauma. He has no cardiac or pulmonary problems in the past. His oxygen saturation is 92% on air and his respiratory rate is 26 breaths/minute. What is the most appropriate investigation?
Correct Answer : C
Tall thin young men are particularly prone to develop pneumothorax. Sudden pain and breathlessness in this young man are highly suggestive for pneumothorax. A standard erect CXR in inspiration is recommended for the initial diagnosis of pneumothorax.
Q.53. A morbidly obese 60 year old man has a right hemicolectomy for a tumour of the caecum 4 days ago. He suddenly becomes breathless, dizzy and describes chest discomfort. The chest discomfort worsens when he takes a deep breath. On examination, he has good air entry on both lungs. His oxygen saturation is 90% on room air and he has a pulse rate of 110 beats/minute. A chest X-ray was performed and was reported as normal. An ECG shows sinus tachycardia. What is the most likely diagnosis?
Correct Answer : A
The diagnosis here is pulmonary embolism. Although hypoxia and chest discomfort are word used to describe a pulmonary embolism, chest infection, or pneumothorax, the findings of worsening pain when taking a deep breath (pleuritic pain) and a normal chest X-ray point towards a diagnosis of pulmonary embolism. Examination of the chest may be normal in patients with pulmonary embolism.
ECG changes such as SQ3T3 pattern are uncommon in pulmonary embolism (often they may show sinus tachycardia or right heart strain).
A CT pulmonary angiogram (CTPA) would confirm the diagnosis. Other risk factors in this stem that should point you toward the diagnosis of pulmonary embolism are:
• He has likely bedridden for the past few days since the major surgery
• He has a high BMI.
Q.54. A 34 year old woman with a smoking history has had an uneventful laparascopic cholecystectomy 18 hours ago. She is now complaining of shortness of breath. She has a pulse rate of 108 bpm and a temperature of 37.8 C. There are signs of reduced air entry at the right base. Chest X-ray shows no obvious abnormality. What is the most appropriate next step?
Correct Answer : D
The four most likely common causes of post-operative breathlessness are:
- Infection/ Atelectasis
- Pulmonary embolism
- Left ventricular failure (fluid overload)
- Exacerbation of underlying lung disease such as COPD
The time of the surgery in this question helps us with the diagnosis. As this is an early complication (hours rather than days), it is likely to be either atelectasis or pulmonary embolism.
However, since no other factors are pointing towards a pulmonary embolism and there is a smoking history, the more likely diagnosis here would be atelectasis.
Atelectasis is the collapse or closure of a lung resulting in reduced or absent gas exchange.
Management of atelectasis :
Adequate analgesia to encourage expectoration, nebulized saline, chest physiotherapy, deep breathing and coughing, postural drainage, and incentive spirometry.
If the lung does not re-inflate, consider bronchoscopy to suction out secretions.
Pneumonia may happen in about 3 days if atelectasis is not resolved. If this happens, fever will persist and Chest x-ray will show infiltrates.
Q.55. A 39 year old chronic smoker attends the outpatient department with complaints of persistent cough and copious amount of purulent sputum. He has recurrent chronic chest infections in the past. Finger clubbing is noted in examination and inspiratory crackles are heard on auscultation. A chest X-ray was done and results were normal. What is the most likely diagnosis?
Correct Answer : A
The history of smoking here is irrelevant as smoking does not appear to be an independent risk factor but smoking cessation is important as part of the management if the patient does smoke.
The persistent cough and copious amount of purulent sputum are symptoms of bronchiectasis. Measles is a childhood viral infection that is one of the aetiologies of bronchiectasis. Finger clubbing is not a specific sign but has been seen in bronchiectasis although not very frequently.
Inspiratory crepitations and a chest-x ray that shows tramlines give a more specific picture pointing towards bronchiectasis. Although these are not diagnostic, the most probable diagnosis among the others is bronchiectasis. Only a high-resolution computed tomography (HRCT) chest would give you the diagnosis of bronchiectasis.
Q.56. An 8 year old boy diagnosed with asthma is on salbutamol inhaler and beclomethasone inhaler. He takes his beclomethasone inhaler everyday as prescribed and does not miss any doses. However, he wakes up at night with wheezing and having shortness of breath. He uses around 6 times of his salbutamol inhaler a week. He occasionally finds exercise difficult because he becomes very short of breath. What is the most appropriate management?
Correct Answer : C
The third step management for asthma differs between several guidelines. In general, we can add on LABA or Montelukast. As Montelukast is not available here, LABA would be the most suitable option.
Q.57. A 10 year old boy who takes regular dose inhaled steroids for his long standing asthma has been advised to use bronchodilators to control his acute attacks. His parents are unsure when he should use his bronchodilator. What is the most appropriate investigation to perform?
Correct Answer : D
The peak flow rate diary for asthmatics would usually show diurnal variation. This is because symptoms of asthma often worsen at night. This peak flow diary shows when the bronchoconstriction remains worse and with the results, we can guide the patient on the the best times to use bronchodilators which is usually prior to those times.
Q.58. A 21 year old man has exercise induced asthma and is using a salbutamol inhaler as required and beclomethasone inhaler 400 mcg/day. He complains of wheeze and shortness of breath during exercise despite using salbutamol inhaler just before exercise. What is the most appropriate action?
Correct Answer : D
Sodium cromoglycate can be added for exercise-induced asthma.
Q.59. A 28 year old female who has returned from the US to the UAE presents to Accident & Emergency with shortness of breath and a cough beginning 3 days after her return to the United Kingdom. Her cough initially contained blood but is now dry. Her only significant history is that she is on the combined oral contraceptive pill. What is the most likely diagnosis for this woman’s symptoms?
Correct Answer : C
In exam, when the examiners want you to choose pulmonary embolism, they will mention:
1. History of prolonged immobility (such as airplane travel)
2. Risk factors for PE (COCP, surgery, obesity, etc.)
3. Patient experiencing shortness of breath
PULMONARY EMBOLISM :
Risk factors
- Surgery
- Pregnancy (including the postnatal period)
- Lower limb injury
- Malignancy
- Reduced mobility
- Previous VTE (venous thromboembolism)
Signs and symptoms:
Remember that these are non-specific
Symptoms include:
- Dyspnoea
- Pleuritic chest pain or retrosternal chest pain
- Cough and hemoptysis
Signs include:
- Tachypnoea and tachycardia.
- Hypoxia, which may cause anxiety, restlessness, agitation, and impaired consciousness.
- Pyrexia
- Elevated jugular venous pressure.
- Gallop heart rhythm, a wide split-second heart sound, tricuspid regurgitant murmur.
- Pleural rub
- Systemic hypotension and cardiogenic shock.
All you need to remember in terms of diagnosis and management for the exam is that CTPA is the gold standard for diagnosis of pulmonary embolism and that immediate administration of LMWH (low molecular weight heparin) or fondaparinux must be given once the PE is suspected (even prior to CTPA).
Q.60. A 55 year old woman with a persistent cough and history of smoking develops left sided chest pain exacerbated by deep breathing. She has a temperature of 38.2 C and basal crackles are heard on auscultation. What is the most likely diagnosis?
Correct Answer : A
These are typical signs and symptoms of pneumonia. Pleuritic pain can occur with pneumonia. Crackles can be heard in patients with pneumonia.
Symptoms of cough, purulent sputum which may be blood-stained or rust-coloured, breathlessness, fever, and malaise are usually how pneumonia presents.
Q.61. A 32 year old previously healthy woman has developed pain and swelling on both knees and ankles with a nodular rash over her shins. She describes feeling more fatigue over the past few weeks with a mild grade fever. As part of the investigation a chest X-ray was performed. What is the most likely appearance on the chest x-ray?
Correct Answer : D
A very commonly asked topic on exams.
The questions would usually provide 2 out of the 3 important clinical features of Lofgren syndrome and ask for the third feature.
Lofgren syndrome includes :
1. Erythema nodosum
2. Arthritis
3. Bilateral hilar lymphadenopathy.
Thus if you see any 2 of the 3 features stated above, the first thought should be Lofgren (a distinct sarcoid syndrome).
The fatigue and fever will distract you from the answer. However, it is worth remembering that sarcoidosis also presents with fatigue and fever.
Q.62. A 15 year old boy presents to the Emergency Department with a sudden onset of chest pain and increasing shortness of breath during a beach volleyball game. He has a medical history of asthma and is on a beta-2 agonist inhaler. On examination, there is no cyanosis but there are reduced breath sounds on the left side. Which of the following is the most appropriate investigation?
Correct Answer : A
This is a diagnosis of spontaneous pneumothorax.
Key clues for the exam: A young male playing a sport develops sudden shortness of breath. There usually would be clues of “decreased breath sounds on one side”. Sometimes they may say a “tall” man or an “athlete”, as these would be the common presenters of spontaneous pneumothorax.
Primary spontaneous pneumothorax occur most commonly in tall thin men aged between 20 and 40. Cigarette is a major risk factor for pneumothorax.
Q.63. A 24 year old male is admitted with acute severe asthma. He is treated initiated with 100% oxygen, nebulized salbutamol, and IV hydrocortisone. Ipratropium bromide was added to nebulizers. Despite the initial treatment there has been no improvement. What is the most appropriate next step in management?
Correct Answer : B
Next step would be IV magnesium sulphate.
Q.64. A 64 year old man who was previously exposed to asbestos for 35 years while working as a builder has chest pain and shortness of breath. The diagnosis of mesothelioma has been made. His shortness of breath has been worsening over the last couple of days. A recent chest x-ray shows bilateral pleural effusion. What is the most appropriate management?
Correct Answer : C
This patient's symptoms are due to the pleural effusion secondary to mesothelioma. A long-term indwelling pleural drainage may be useful in this scenario where he has a malignant effusion. Chemotherapy, radiotherapy, and surgery are used in the management of mesothelioma but this patient's major problem is his current shortness of breath which needs to be treated.
Palliative radiotherapy provides pain relief in some patients with chest wall pain but is less useful in the treatment of breathlessness. Radiotherapy and surgery can be quite controversial and is unlikely to be the answer in an exam as it requires a great depth of knowledge.
Q.65. A 59 year old smoker presents to his GP clinic with the complaint of breathlessness. His wife, who has accompaneid him today, reports that the patient had been having difficulty with breathing especially for the past week. His oxygen saturation was 81% on air, his pulse was 90 beats/minute and his blood pressure was recorded at 110/75 mmHg. He was given nebulised salbutamol and thereafter, his oxygen saturation and symptoms improved. Chronic obstructive pulmonary disease (COPD) was suspected and he was asked to come back another time to perform a spirometry. The spirometry performed on this patient showed a decreased FEV1. What other finding can also be observed in a patient with COPD on spirometry?
Correct Answer : D
The guidelines state that the criteria for diagnosing COPD on spirometry are as follows: FEV1 (Forced Expiratory Volume in 1 second) less than 80% of predicted AND a FEV1/FVC (Forced Vital Capacity) less than 70%. It is important to note that in obstructive lung diseases such as COPD and asthma, volumes are essentially normal but flow rates are impeded.
Note: The reason that this patient was asked to come back another time to perform spirometry is it should only be tested when the patient’s condition is stable which is ideally six weeks after the last exacerbation.
Q.66. A 28 year old male is admitted with acute exacerbation of asthma. He has a temperature of 38.1 C and a productive cough. He is treated initiated with 100% oxygen and salbutamol nebulizers. Despite treatment, his oxygen saturation is 88% and respiratory rate is 34 breaths/minute. What is the most appropriate next step in management?
Correct Answer : C
Hydrocortisone should be given first as this is an acute exacerbation of asthma. The aetiology is probably due to a chest infection which initiated the exacerbation for which we will prescribe antibiotics. But, we need to sort out his shortness of breath first and aim for a saturation of 94-98%.
Q.67. A 33 year old man has mild headache and myalgia for 2 days followed by high fever, chills, rigors and a cough. His cough was initially dry but progressed to be productive. He has just returned from a conference in Greece where he mentions that he swam and used the hot tubs in the hotel. He has a temperature oef 38.1 C and is seen to be dyspnoeic. Chest X-ray shows patchy alveolar infiltrates. What is the most likely organism which would have caused his symptoms?
Correct Answer : A
Legionella pneumophila is the causative organism that causes Legionnaires' disease which is a severe, potentially fatal acute pneumonia acquired by droplet inhalation of water contaminated. L. pneumophila is found in natural water supplies and soil.
It is also found in many recirculation and water supply systems. For the purpose of this exam, look out for hints like traveling, hotel stays, whirlpool spas, and hot tubs as often they would put one of these hints in the question if the examiners would like you to select Legionella pneumophila as the answer.
Q.68. A 68 year old male presents to Accident & Emergency with the complaint of a cough. He said that he first noticed the cough two days ago. He is coughing up about a tablespoon full of purulent sputum a day. He has no other complaints. His past medical history is significant for hypercholesterolaemia for which he takes atorvastatin. He is also on bisoprolol, aspirin, diclofenac, lansoprazole as well as a regular salbutamol inhaler for asthma. He had a severe allergic reaction to amoxicillin a year ago which he was hospitalized for. Upon examination, he appears to be unwell. He is short of breath with a respiratory rate of 22 breaths per minute and his oxygen saturation on room air is 97%. A chest X-ray was done which showed right middle zone consolidation. What is the most appropriate antibiotic for this patient?
Correct Answer : A
The best antibiotic to give this specific patient is doxycycline. Doxycycline can be used in lower respiratory tract infections for patients in whom penicillin is contraindicated.
Q.69. A 59 year old man with a medical history of chronic obstructive pulmonary disease presents to the Emergency Department with breathlessness. He finds it extremely difficult to breathe while in the supine position and has to sit up in bed or in a chair at night due to his severe dysponoea. His respiratory rate is 30 breaths/minute and his heart rate is 110 beats/minute. His oxygen saturation on presentation was 89%. An arterial blood gas test was done for him and he was commenced on 100% oxygen however, he is still dyspnoeic. The results of his arterial blood gas are as follows: pH 7.20 PaO2 11.6 kPa PaCO2 9.8 kPa. What is the most appropriate initial action?
Correct Answer : C
This patient is experiencing an exacerbation of COPD. Giving oxygen would be the first action. The history of COPD alone should prompt you to pick 24% oxygen instead of 100% oxygen. This is because 100% oxygen will abolish the hypoxic drive and worsen hypercapnia.
Remember, for COPD patients, you should be aiming for an SaO2 of 88-92%, (compared with 94-98% for most acutely ill patients NOT at risk of hypercapnic respiratory failure)
Q.70. A 68 year old man presented to his GP with the complaint of a persistent cough. He says that he had been suffering with the cough for about two months. Further questioning reveals 4.5 kilograms of unintentional weight loss. The patient denies a fever, dyspnoea, sore throat, rhinorrhoea or chest pain but admits that he did cough up a few droplets of blood a few times. His past medical history is significant for chronic obstructive pulmonary disease (COPD). The patient has smoked a pack of cigarettes daily for thirty years but quit five years ago. On general inspection, the patient is noted to be thin with distinct pallor. Examination of the chest reveals no focal wheezes or crackles. There was no lymphadenopathy to be found. His vitals are as follows: Blood pressure 140/82 mmHg Heart rte 80 beats/minute Respiratory rate 17 breaths/minute Oxygen saturation on room air 98% A chest X-ray was done and showed a right perihilar mass. What is the most approprite investigation in this scenario to confirm the diagnosis?
Correct Answer : B
This patient’s history is very suggestive of lung carcinoma. The single most appropriate investigation to consider at this stage would be a bronchoscopy. A bronchoscopy is suitable for central tumours and would be able to provide histological and cytological specimens.
A thorascopy is mainly used for biopsies of pleural lesions and drainage of pleural effusions which is of no use here. While a sputum cytology can be done, it is not the correct option because it is not routinely used.
In the context of possible lung carcinoma, sputum cytology should only be performed in patients who are unfit for bronchoscopy or biopsy. The specificity is high but the sensitivity is low. A bone scan should be ordered when a patient with established cancer presents with recent and new onset bone pain, pathological fractures, or if alkaline phosphatase or serum calcium is seen to be elevated.
Repeating the chest X-ray would yield no further diagnostic information. It would only be useful in patients with suspected pneumonia where we would like to ensure that the initial consolidation seen is no longer present at 6 weeks.
Q.71. A 54 year old male chronic smoker presents with progressive dyspnoea. He complains of cough, wheeze and about a tablespoon full of mucopurulent sputum which he has been coughing out daily for the past 15 months. Spirometry was performed which showed an FEV1/FVC of 2.4/3.7. He was given inhaled salbutamol and spirometry was repeated. His FEV1/FVC after inhaled salbutamol was 2.5/3.8. What is the most likely diagnosis?
Correct Answer : D
He has clear signs of chronic bronchitis. The spirometry is important to perform as it shows that there is irreversible airflow obstruction on spirometry.
Chronic bronchitis - Defined as a productive cough that lasts for three months or more per year for at least two years.
Note that COPD is now the preferred term for patients with airflow obstruction who were previously diagnosed as having chronic bronchitis or emphysema
Presentation :
- Cough accompanied by sputum production
- Dyspnoea
- Low-grade fever (but patients are most commonly afebrile)
- Wheezing
- Smoking
Investigations :
- Pulmonary function test
- Chest X-ray is not required for diagnosis but is important to rule out other diagnoses that are being considered e.g. lung cancer, bronchiectasis.
- Hyperinflated lung fields.
- Attenuation of the peripheral vasculature & Flattened diaphragms.
Remember diagnosis of COPD is based on a history of smoking and progressive dyspnoea, with evidence of irreversible airflow obstruction on spirometry.
Q.72. A 16 year old boy who attends boarding school feels unwell. He developed a dry cough for the last few days. On examination, there are target lesions seen on the back of his hands. A chest X-ray was performed and it shows bilateral consolidations. What is the most likely causative organism?
Correct Answer : C
The diagnosis here is atypical pneumonia.
Mycoplasma pneumoniae is one of those that cause atypical pneumonia that presents with a dry cough. The target lesions are known as erythema multiforme. Mycoplasma pneumoniae is a cause of atypical pneumonia which often affects young adults.
Features - The disease typically has a prolonged and gradual onset - flu-like symptoms classically precede a dry cough - bilateral consolidation on x-ray.
Note: Occasionally, exam may also give a presentation of erythema multiforme along with the atypical pneumonia symptoms. Erythema multiforme is one of the features of infection with mycoplasma pneumoniae.
Q.73. A 58 year old man who used to work in the shipyard industry was having chronic cough and shortness of breath for several months. He was given salbutamol inhalers and intravenous antibiotics and admitted to the ward. A computed tomography was performed which showed patchy infiltrates, pleural thickening and pleural effusion. He died 3 days later after which this case was referred to the coroner. What is the most likely reason for the referral to the coroner?
Correct Answer : C
This patient's symptoms were due to the pleural effusion secondary to mesothelioma. Mesothelioma is classed as an industrial disease.
The coroner will then decide if a post-mortem examination is required and will hold an inquest. An inquest is a legal investigation to establish the circumstances surrounding a person’s death. An inquest is needed because mesothelioma is an occupational disease and one needs to determine whether the death was due to mesothelioma or some other cause.
Q.74. A 68 year old man with advanced non-small cell lung carcinoma diagnosed nine months ago on biopsy presents with the complaints of dyspnoea and sub-sternal chest pain. An X-ray was done and showed a large left hilar mass. He is currently undergoing radiotherapy for his condition and he was relatively well for about two months until he developed thoracic back pain radiating around both sides of his chest. Additional scans showed metastases to T5, T6 and T7 with a mass compressing his spinal cord. The patient is currently on 260 mg of sustained release morphine every 12 hours and he describes his pain control as adequate. Some other symptoms that he suffers from include anorexia, weight loss of about 15 kilograms over the past five months and generalised weakness. He is unable to carry out his daily activities and finds it difficult to do household chores. His wife died five years ago and he has one son who currently lives overseas. Upon further questioning, the patient has no written advanced directive but on several occasions, he has told his general practitioner that he wants nothing more done as far as his treatment is concerned. The patient is a devout Catholic and has expressed concerns over receiving his proper last rites. What is the next best step in the management of this patient?
Correct Answer : A
This question is testing your understanding of end-of-life care.
End-of-life care is support for patients who are in the last stages of their life due to a terminal illness. In this scenario, it is obvious that this patient has terminal cancer. While a written advance directive is important and he should be counseled on this, it is not the next best step in this scenario.
You do not need a referral to a psychiatrist for an advanced directive – any healthcare professional can counsel a patient on advanced directives and not attempt resuscitation (DNR) orders.
The patient is experiencing weight loss and tiredness and while diet is an important part of end-of-life care, referring him to a dietitian would not be the next best step in this case either. While there is a role for spiritual support and social care under end-of-life care, the most important team that needs to manage him is a palliative care team that will provide relief from pain and offer support until death. The palliative care nurses are very well trained to oversee the care of patients at the end of life. Some of them would even do home visits to ensure that patient care is at an optimal level.
Q.75. A 70 year old man admits to asbestos exposure 20 years ago. He was a heavy smoker but quit smoking 3 years ago. He has noted weight loss and hoarseness of voice. Which is the most likely type of cancer associated with the risk factors and symptoms present?
Correct Answer : C
Approximately 95% of all primary lung tumours are bronchial carcinomas. Primary bronchial cancers are classified as follows:
- Small-cell lung cancers (SCLCs)
- Non-small-cell lung cancers (NSCLCs) : Adenocarcinoma accounts for 39% of NSCLCs and is the most common bronchial carcinoma associated with asbestos and is more common in non-smokers, compared with other cell types.
It is also important to note that hoarseness can also be a feature of lung cancer.
Q.76. A 14 year old girl with asthma is having frequent night coughs and mild exercise-induced wheezing. She is compliant with her asthma medication of inhaled corticosteroid and short-acting bronchodilator as required. Her inhaler technique is good. What is the most appropriate next step in management?
Correct Answer : A
The third step management for asthma differs between several guidelines. In general, we can add on LABA or leukotriene receptor antagonist (montelukast). As LABA is not available as an option and the patient is above 12, it would be appropriate to add a leukotriene receptor antagonist as per guidelines.
Q.77. A 61 year old man has suddenly become very short of breath. In the last hour, he has had a CT-guided biopsy of a mass in the right lung. His temperture is 36.5 C, heart rate is 120 bpm, BP 90/60 mmHg, and SaO2 78% on 15 L oxygen. He looks cyanosed, his trachea is deviated towards the left, and breath sounds are much louder over the left hemi-thorax. Which is the most appropriate course of action?
Correct Answer : C
This man has rapidly developed the signs of a pneumothorax. Having just had a needle inserted into his chest, this is almost certainly an iatrogenic pneumothorax.
The deviation of the trachea suggests that it is under tension and so needs urgent reversal. This is done by introducing a cannula into the pleural space, usually in the second anterior intercostal space mid-clavicular line.
Air should be removed until the patient is no longer compromised and then an intercostal tube can be inserted into the pleural space.
The other less appropriate answers are investigations like ABG and chest X-rays. should be deferred as this is a serious situation that would lead to cardiorespiratory arrest unless addressed.
Insertion of a chest drain. will be needed but not until the air has been removed. Insertion of a cannula into the left second intercostal space. Clearly a wrong answer as the trachea is deviated towards the left. This means that the tension pneumothorax is on the right.
Q.78. A 56 year old man complains of increased volume of sputum with specks of blood and chest pain. He has a history of recurrent chronic chest infections and deep vein thrombosis which happened 3 years ago. Finger clubbing was noted on examination. A chest X-ray shows tramlines but is otherwise normal. What is the most likely diagnosis?
Correct Answer : C
The increased volume of sputum with specks of blood and chest pain are symptoms of bronchiectasis. Finger clubbing is not a specific sign but has been seen in bronchiectasis although not very frequently. A chest x-ray that shows tramlines give a more specific picture pointing towards bronchiectasis. Although these are not diagnostic, the most probable diagnosis among the others is bronchiectasis.
Only a high-resolution computed tomography (HRCT) chest would give you the diagnosis of bronchiectasis. It is very rare that the question writers would attempt to trick you. But this is one of the questions that may be misleading as they give a history of DVT which is irrelevant for bronchiectasis.
Q.79. A 50 year old man has had hoarseness of voice and a left drooping eyelid for the past 2 months. He also has diminished sweating on same side of face. Finger clubbing is noted on examination. He smokes 20 cigarettes a day for the last 30 years. What is the most likely diagnosis?
Correct Answer : C
A Pancoast tumour is a tumour of the pulmonary apex. The hoarseness of the voice is due to compression of the recurrent laryngeal nerve. An ipsilateral invasion of the cervical sympathetic plexus leads to Horner's syndrome (miosis, enophthalmos, ptosis).
The history of smoking and finger clubbing gives a clue towards a bronchogenic neoplasm.
Pancoast's Syndrome classically caused by an apical (superior pulmonary sulcus) malignant neoplasm of the lung. The neoplasm is usually bronchogenic in origin (most commonly squamous cell carcinoma, sometimes adenocarcinoma and large-cell carcinoma).
Presentation : This syndrome results from the invasion of several structures and tissues around the thoracic inlet and may be characterized by:
- An ipsilateral invasion of the cervical sympathetic plexus leading to Horner's syndrome (miosis, enophthalmos, ptosis)
- Ipsilateral reflex sympathetic dystrophy may occur.
- Shoulder and arm pain (brachial plexus invasion C8-T2) leading to wasting of the intrinsic hand muscles and paraesthesiae in the medial side of the arm.
- Less commonly, unilateral recurrent laryngeal nerve palsy produces unilateral vocal cord paralysis (hoarse voice ± bovine cough)
- There may be arm oedema secondary to the compression of blood vessels.
Q.80. A 24 year old man presents with acute respiratory distress after being stabbed in the back. The trachea is not deviated, but he has engorged neck veins and reduced air entry on his right chest. He has a blood pressure of 80/50 mmHg, a pulse of 135 beats/minute, and a respiratory rate of 35 breaths/minute. What is the most likely diagnosis?
Correct Answer : A
The patient has signs of a tension pneumothorax and requires urgent needle compression. Some might argue here this is a haemothorax. The stem states that the neck veins are engorged. In haemothorax, there is no distension of neck veins or raised jugular venous pressure due to the hypovolaemic state.
Engorged neck veins indicate that the pressure within the right ventricle is high. This is seen in both cardiac tamponade and tension pneumothorax. It is not seen in simple pneumothorax, pleural effusion, and haemothorax.
Another reason against haemothorax is that it would be very unlikely that a stab wound in the back would involve the heart (which is in the anterior mediastinum) AND the right lung. The decision between cardiac tamponade and tension pneumothorax is a difficult one.
Do not be confused by the trachea’s lack of deviation – in real life, this is not a very sensitive sign! The patient is hypotensive, tachycardic, tachypnoeic, and very unwell. Reduced entry on his right chest indicates that this is the side of the tension pneumothorax (presuming he was stabbed on the right side) It is important to remember Beck’s triad for cardiac tamponade.
The patient has both hypotension and engorged neck veins, but the heart sounds have not been commented on (which are usually muffled).
Q.81. A 35 year old man presents with progressive breathlessness and a non-productive cough. He has been more lethargic over the past few months. He has a history of polyarthralgia with painful red lumps appearing on his shins. They are cherry sized and are about 20 or more in number. His chest X-ray shows bilateral hilar lymphadenopathy. What is the most likely diagnosis?
Correct Answer : B
Please see Q-36
Q.82. A 79 year old lady is brought in by ambulance to the Emergency Department with shortness of breath that worsened dramatically overnight. She has been feeling unwell for the past two weeks with a cough and slight shortness of breath of which her general practitioner has prescribed her amoxicillin seven days ago. The ambulance crew tells you that she initially had saturations of 70% before being started on oxygen. She is not known to have COPD but has been a heavy smoker for the past 50 years of her life. On examination, she is seen to be struggling to breathe. Her respiratory rate is 26 breaths/minute, heart rate is 105 beats/minute and blood pressure is 110/70 mmHg. A chest X-ray was performed which is shown below. What is the most likely diagnosis?
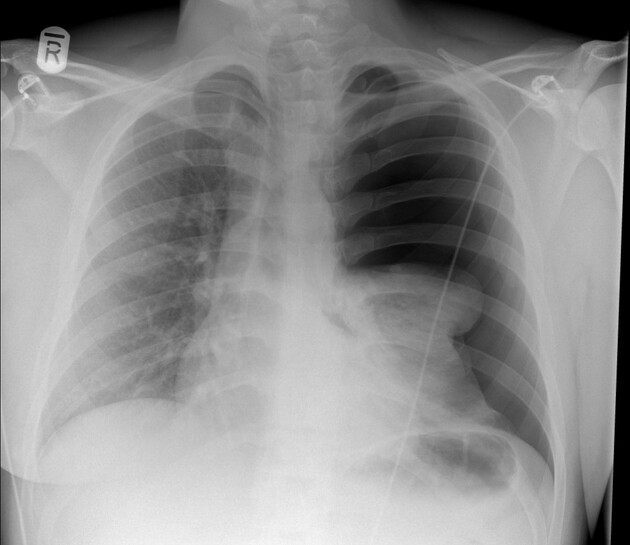
Correct Answer : D
The chest X-ray clearly shows a left pneumothorax with right lung collapse and mediastinal shift. The right lung is completely compressed and the trachea is pushed to the left. It is obvious that there are no lung markings on the right field.
You will not be asked for complicated X-rays in the exam, but life-threatening X-rays like this which it is easy to spot should not be missed in the exam and also in practice. An urgent chest drain would be required to alleviate her symptoms and prevent the worsening of the mediastinal shift.
Although she is likely to be an undiagnosed COPD patient given the history of her smoking, the more important diagnosis at the moment is the left pneumothorax.
The undiagnosed COPD that this patient has is likely the cause of her secondary spontaneous pneumothorax. Remember, if it is clinically clear that you have a patient with tension pneumothorax, do not request an X-ray just yet, treat the patient!
Q.83. A 25 year old tall rugby player comes to the Emergency Department complaining of chest pain and shortness of breath that developed earlier in the day. He was hit in the chest by a player of the opponent team during a rugby match. He has no significant medical history. The triage nurse takes his observations and notices that his oxygen saturations are 89% on air, respiratory rate is 26 breaths/minute, heart rate is 100 beats/minute. You have been called to look at him. What is the most appropriate initial action?
Correct Answer : A
The patient is likely having difficulty breathing from a pneumothorax. Administration of oxygen would always be your first step in a desaturating patient.
Q.84. A 55 year old man presents with increasing breathlessness, noisy breathing and a history of hoarseness of voice. He has a chronic cough that is productive. He has noticed his symptoms worsening over the past 3 weeks . He smokes 15 cigarettes a day for the past 25 years. His spirometry results show the following: • FEV1 60% predicted • FEV1/FVC ratio 0.67 post bronchodilation. What is the most likely diagnosis?
Correct Answer : D
Remember that diagnosis of COPD is based on the history of smoking and progressive dyspnoea, with evidence of irreversible airflow obstruction on spirometry which this patient ticks all of them. Tracheal compression is not correct. Tracheal compression refers to any pressure on the trachea sufficient to cause displacement.
This is usually in the context of an enlarging thyroid mass. The reason many people mistakenly pick tracheal compression is because they assume compression of the recurrent laryngeal nerve could explain the hoarseness of voice however, it fits one symptom but not the remaining ones. COPD is a much better fit in this scenario. The spirometry findings for the diagnosis of COPD are very important and worth remembering.
The presence of airflow obstruction should be confirmed by performing post-bronchodilator spirometry.
Airflow obstruction is defined as :
• FEV1 < 80% predicted and FEV1/FVC < 0.7.
Q.85. A 60 year olf man presents to his general practitioner with the primary complaint of shortness of breath. He complains that he has been having increasing shortness of breath for the past seven months and that his symptoms have escalated to such a stage that he is now unable to walk the length of his hallway at home without becoming breathless. Further questioning reveals that the patient is also suffering frm a dry cough that has been present for the past five months. His past medical history is significant for hypertension, diagnosed when he was 55 years of age, which he takes ramipril for. The patient says that he is compliant with his medication. The patient says that he has worked in a warehouse for the past 30 years and specifically mentions that he has not been exposed to asbestos. Upon examination, the patient appears unwell and gaunt. Finger clubbing is noted and fine inspiratory crackles can be appreciated bilaterally upon auscultation of his lungs. His vitals are as follows: Blood pressure 145/86 mmHg Temperature 36.8 C Respiratory rate 89% on room air A lung function test was subsequently carried out and the results are as follows: FEV1 60% of predicted FVC 40% of predicted FEV1/FVC ratio 0.8. What is the most likely diagnosis for the patient?
Correct Answer : C
This is a very straightforward question but it does test your knowledge of lung function testing thoroughly.
The pulmonary indices indicate a restrictive lung disease. The only choice that is a restrictive lung disease is pulmonary fibrosis. Asthma, bronchiectasis, pulmonary oedema, and chronic obstructive pulmonary disease are all obstructive lung diseases.
Q.86. A 55 year old man attends the Accidents & Emergency with complaints of a productive cough for the past 14 days. He feels unwell and complains of mild shortness of breath. His observations show that he has a temperature of 38.9 C, a respiratory rate of 25 breaths/minute, heart rate of 90 beats/minute, and a blood pressure of 110/80 mmHg. A chest X-ray shows right lower lung consolidation. His blood results are unremarkable. The triage note states that he has a severe allergic reaction involving anaphylaxis to penicillin in the past. What is the most appropriate management?
Correct Answer : D
Amoxicillin and co-amoxiclav are a class of penicillins and should not be given to penicillin-allergic patients. Cefuroxime (and all cephalosporins) has a cross-reactivity of around 10% to penicillins. This means 1 in 10 patients with a penicillin allergy, would develop the allergy if taking a cephalosporin. These options can be crossed out almost immediately with a history of a severe penicillin allergy.
The next step is to calculate the CURB-65 score to assess the need for hospital admission.
The CURB-65 is a clinical prediction rule that helps predict mortality in patients with community-acquired pneumonia.
It consists of 5 risk factors – each scoring one point:
• Confusion of new onset (AMTS of 8 or less)
• Blood urea nitrogen (BUN) > 19 mg/dL (> 7 mmol/L)
• Respiratory rate - 4- breaths/minute
• Systolic BP < 90 mmHg or Diastolic BP - 60 mmHg
• Age - 65
The choice of antibiotic to prescribe depends on the severity of the illness. The patient scores 0 on his CURB-65 score and thus can be managed at home.
If CURB-65 score = 0
• Prescribe amoxicillin
• If penicillin allergy, prescribe doxycycline or clarithromycin (other macrolides like erythromycin can also be used)
If CURB-65 score = 1 or 2
• Dual therapy with amoxicillin and clarithromycin or monotherapy with doxycycline
• Hospital admission can also be considered for patients who score 2 on their CURB-65 score
If CURB-65 score = 3
• Arrange hospital admission usually for IV antibiotics.
Q.87. A 37 year old woman presents to the Emergency Department with shortness of breath and coughing with blood stained sputum. She flew from Thailand to United Kingdom 3 days ago. She denies any fever. Her oxygen saturation is 92% on room air. She has a heart rate of 105 beats/minute, respiratory rate of 25 breaths/minute and a blood pressure of 120/90 mmHg. What is the most appropriate investigation?
Correct Answer : B
CTPA is the answer here as it is the best test among the other options that provide a definitive diagnosis of pulmonary embolism.
Q.88. A 48 year old man was admitted with cough and dyspnoea. He has a long history of smoking. He has noticed some recent weight loss. A chest X-ray was performed and showed consolidation on the lower left lobe. He was started on antibiotics and is due for discharge. What is the most appropriate follw up investigations to perform after discharge?
Correct Answer : A
A chest X-ray should be performed after he recovers. As he is a smoker and has lost significant weight, lung malignancy should be part of the differential. The first chest X-ray shows consolidation of the left lower lobe which is consistent with pneumonia. A repeat chest X-ray would be required to assess malignancy as the consolidation of the left lower lobe could have hindered a proper assessment of lung carcinoma.
Q.89. A 27 year old man who is a known asthmatic presents to the Emergency Department with shortness of breath. He has a respiratory rate of 25 breath/minute and a heart rate of 110 beats/minute. He has bilateral wheeze heard on auscultation. He looks drowsy, agitated and has poor respiratory effort. Which of the following is a criteria for life threatening asthma?
Correct Answer : A
Life-threatening asthma has the following features • PEF < 33% best or predicted • SpO2 < 92% • PaO2 < 8 kPa
• Normal PaCO2 (4.6-6.0 kPa)
• Silent chest
• Cyanosis
• Poor respiratory effort
• Arrhythmia
• Exhaustion
• Altered conscious level
• Hypotension
Q.90. A 28 year old male is admitted with acute exacerbation of asthma. He is treated initated with 100% oxygen, salbutamol nebulizers and hydrocortisone 100 mg IV. Despite treatment, his oxygen saturation is 89% and respiratory rate is 30 breaths/minute. What is the most appropriate next step in management?
Correct Answer : B
Salbutamol and hydrocortisone have been given rightly so since it is an acute exacerbation of asthma. Ipratropium nebulizers should be added next as they will improve symptoms. The aetiology is probably due to a chest infection which initiated the exacerbation for which we will prescribe antibiotics. But, we need to sort out his shortness of breath first and for a saturation of 94-98%.
Q.91. A 74-year-old smoker presented to his GP with cough and shortness of breath. Exam revealed pigmentation of the oral mucosa and also over the palms and soles. Tests show that he is diabetic and hypokalemic. What is the most probable diagnosis?
Correct Answer : C
The patient probably developed small cell lung cancer which is working as a tumour producing ectopic ACTH.
Hyperpigmentation is caused by high levels of circulating ACTH that bind to the melanocortin 1 receptor on the surface of dermal melanocytes. Ectopic ACTH-induced raised cortisol is leading to diabetes and hypokalemia. A variant of Cushing's disease can be caused by ectopic ACTH production from small-cell lung cancer.
Q.92. A 26-year-old man presents to emergency department with increasing shortness of breath on left side and chest pain. He has been a heavy smoker for the past 4 years. He doesn’t have any past medical history. What is the likely diagnosis?
Correct Answer : D
A pneumothorax occurs when air leaks into the space between the parietal and visceral pleura.
This air pushes on the outside of the lung and makes it collapse. It may be a complete collapse or partial. A pneumothorax can be idiopathic or caused by a blunt or penetrating chest injury, certain medical procedures, or damage from underlying lung disease and rupture of subpleural blebs. The main symptoms of a pneumothorax are sudden chest pain and shortness of breath.
Pneumothorax may be
i. Spontaneous pneumothorax
ii. Iatrogenic pneumothorax and
iii. Tension pneumothorax.
History and physical examination remain the keys to making the diagnosis of pneumothorax.
Chest X-ray is most commonly used. In the given case increased shortness of breath and chest pain with no past medical history favours the diagnosis of pneumothorax. Heavy smoking or tobacco is a risk factor for spontaneous pneumothorax.
Q.93. A 35-year-old man presents with progressive breathlessness. He gave a history of polyarthralgia with painful lesions on the shin. CXR: bilateral hilar lymphadenopathy. What’s the most likely diagnosis?
Correct Answer : C
Sarcoidosis is a granulomatous inflammatory disease that affects multiple organs in the body, but mostly the lungs, skin, and lymph glands. The given case is termed Lofgren’s syndrome. Lofgren's syndrome is an acute form of sarcoidosis characterized by erythema nodosum, bilateral hilar lymphadenopathy, and polyarthralgia or polyarthritis.
Q.94. A 10-year-old girl presents with hoarseness of the voice. She is a known case of bronchial asthma and has been on oral steroids for a while. What is the most likely cause of hoarseness?
Correct Answer : A
Here laryngeal candidiasis is due to steroid. Steroids predisposes to fungal infection.
Q.95. A 20-year-old student attends the OPD with complaint of breathlessness on and off, cough and sputum. His sleep is disturbed and skin is very dry in flexural areas of the body. Examination: tachypnea, hyperresonant percussion and wheezing on auscultation. What is the most likely diagnosis?
Correct Answer : B
Diagnostic criteria of asthma :
i) Airway hyper-responsiveness to certain stimuli
ii) Recurrent variable airflow limitation usually reversible
iii) presents as wheezing, breathlessness, chest tightness, and cough.
Asthma is often associated with eczema which may be present as dryness and itching of flexures.
Q.96. An old alcoholic presents with cough, fever, bilateral cavitating consolidation. What is the most probable cause?
Correct Answer : B
The picture is of pneumonia and bilateral cavitating consolidation favours staphylococcus as the causative agent.
Q.97. A 20-year-old man has a head on collision in a car. On presentation he is breathless, has chest pain and fracture of 5-7th rib. CXR confirms this. What is the most appropriate initial action in this patient?
Correct Answer : C
O2 by mask.
Q.98. A 50-year-old chronic smoker came to OPD with complaint of chronic productive cough, SOB (shortness of breath) and wheeze. Laboratory investigations: CBC=increase in PCV. CXR >6ribs seen above the diaphragm in midclavicular line. ABG=pO2 decreased. What is the most likely diagnosis?
Correct Answer : D
Points in favour of COPD :
i) Age 50 yrs
ii) Chronic smoker
iii) Chronic productive cough, SOB, and wheeze
iv) Raised PCV secondary to chronic hypoxaemia
v) Low set diaphragm and widened horizontal ribs
vi) Hypoxaemia on ABG
Q.99. A 32-year-old previously healthy woman has developed pain and swelling of both knees and ankles with nodular rash over her shins. As part of the investigation a chest X-ray has been performed. What is the most likely chest X-ray appearance?
Correct Answer : B
Diagnosis is sarcoidosis, more specifically Lofgren’s syndrome.
It is the triad of -
i) Erythema nodosum
ii) Bilateral hilar lymphadenopathy
iii) Arthralgia
Q.100. A patient complains of SOB (shortness of breath), wheeze, cough and nocturnal waking. He has dry scaly shin with rashes that are itchy. What is the most likely diagnosis?
Correct Answer : B
Eczema (Asthma may be associated with atopy).
Q.101. A child suffering from asthma presents with Temp 39 C, drooling saliva on to the mother’s lap, and taking oxygen by mask. What sign will indicate that he is deteriorating?
Correct Answer : C
Intercostal recession is a sign of severe asthma but it can be seen at a lesser degree as well. So drowsiness is more appropriate answer.
Q.102. A 48-year-old farmer presented with fever, malaise, cough and SOB. Examination: tachypnea, coarse end-inspiratory crackles and wheeze throughout, cyanosis. Also complaint severe weight loss. His CXR shows fluffy nodular shadowing and there is PMN (polymorphonuclear) leukocytosis. What is the most appropriate diagnosis?
Correct Answer : D
Hypersensitivity pneumonitis (also known as extrinsic allergic alveolitis) refers to a group of lung diseases in which the lungs become inflamed as an allergic reaction resulting from exposure to dust of animal and vegetable origin.
It starts with fever, muscular aches, and a general, unwell feeling or malaise. These symptoms are accompanied by tightness in the chest, a dry cough, and shortness of breath.
Symptoms may develop between 4 and 8 hours after exposure.
Chest X-ray shows fluffy nodular shadowing and there is polymorphonuclear leukocytosis.
Treatment of extrinsic allergic alveolitis initially depends on the identification of the cause of the allergic reaction.
If possible, the patient should avoid exposure to the allergen. In an occupational setting, mild cases may be alleviated by improved ventilation or the use of air-filtering masks.
Q.103. A 30-year-old female attends OPD with a fever and dry cough. She says that she had headache, myalgia and joint pain like one week ago. Examination: pulse 100 bpm, temperature 37.5C. CXR: bilateral patchy consolidation. What is the most likely causative organism?
Correct Answer : C
Myalgia, joint pain, headache, bilateral patchy consolidation points towards mycoplasma pneumonia.
Q.104. A 45-year-old IV drug abuser is brought into the emergency department with complaint of fever, shivering, malaise, SOB and productive cough. Examination: temperature 39C, pulse 110bpm, BP 100/70mmHg. Investigation: CXR bilateral cavitating bronchopneumonia. What is the most likely causative organism?
Correct Answer : B
Among the given causes Staphylococcus and PCP are recognized cause of cavitating pneumonia. This case is with productive cough which goes more with staphylococcus as PCP is not productive but rather associated with dry cough. Drug abuse can support both staphylococcus and PCP.
Q.105. A 45-year-old chronic smoker attends the OPD with complaints of persistent cough and copious amount of purulent sputum. He had history of measles in the past. Examination: finger clubbing and inspiratory crepitations on auscultation. What is the most likely diagnosis?
Correct Answer : B
Persistent cough with copious purulent sputum and finger clubbing points towards the diagnosis of bronchiectasis. Severe lung infections such as tuberculosis (TB), whooping cough, pneumonia, or measles can damage the airways at the time of infection. Bronchiectasis may then develop later on.
Q.106. A 68-year-old man has had malaise for 5 days and fever for 2 days. He has cough and there is dullness to percussion at the left lung base. What is the most appropriate investigation?
Correct Answer : B
Given presentation is suggestive of pneumonia for which investigation of choice is CXR.
Q.107. A tall thin young man has sudden pain in the chest and becomes breathless while crying. What is the most appropriate investigation?
Correct Answer : B
Tall thin young men are particularly prone to develop pneumothorax. Sudden pain and breathlessness in this young man are highly suggestive of pneumothorax. So investigation of choice is CXR.
Q.108. A 55-year-old woman with a persistent cough and history of smoking develops left sided chest pain exacerbated by deep breathing with fever and localized crackles. What is the most appropriate diagnosis?
Correct Answer : C
Chest pain exacerbated with deep breathing, fever and localized crackles are highly suggestive of pneumonia.
Q.109. A 14-year-old boy with asthma suddenly developed chest pain and increasing breathlessness during a game of football. When seen in the emergency department he was not cyanosed. He has reduced breath sounds on the right side. His oxygen saturation is 94% on air. What is the most appropriate investigation?
Correct Answer : B
Asthma is a predisposing factor for spontaneous pneumothorax. The the presentation indicates pneumothorax for which the most appropriate investigation is CXR.
Q.110. A 39-year-old man presents to the emergency department with persistent cough, sputum and dyspnea. He gave a history of smoking 20 cigarettes/day for the last 10 years. Patient was given oxygen in ambulance but he is not improving. What is the next step?
Correct Answer : C
The patient has COPD and as no improvement with oxygen, next the step is to check ABG to give guidance for the next treatment plan (need for assisted ventilation).
Q.111. A 35-year-old man has a temperature of 39 C, cough with purulent sputum and right sided chest pain on inspiration. He has herpes labialis. What is the most likely causative organism?
Correct Answer : C
High temperature, cough with purulent sputum, pleuritic chest pain, and herpes labialis are recognized features of pneumococcal pneumonia. This pneumococcus is Gram +ve diplococci.
Q.112. A 16-year-old girl has been unwell for 5 days with malaise, headache and dry cough. She has a few crackles in her chest. Her CXR shows patchy consolidation in the lower lobes. What is the most likely causative organism?
Correct Answer : A
Mycoplasma pneumonia, a form of atypical bacterial pneumonia related to cold agglutinin disease.
Q.113. A 56-year-old man complains of increased volume of sputum with specks of blood and chest pain. He has a history of DVT. Examination: clubbing. What is the cause of blood in his sputum?
Correct Answer : C
Increased volume of sputum with specks of blood and clubbing points towards bronchiectasis.
Q.114. A 32-year-old female has a history of SOB (shortness of breath) and fever. Prebroncho- dilation test was done and it was 2/3.5 and post-bronchodilator was 3/3.7. The patient has history of eczema and past TB. What is the possible diagnosis?
Correct Answer : B
Airway reversibility and presence of atopy (eczema) favours the diagnosis of asthma.
Q.115. A 53-year-old man with previous history of COPD presents with breathlessness and purulent sputum. O2 staturation 85% on air. ABG: PaO2-7.6, PaCO2-7. What is the appropriate management for his condition?
Correct Answer : A
Patient has hypoxemia and hypercapnea (type 2 respiratory failure). Hence he should be put on 24% oxygen. 100% oxygen will abolish hypoxic drive and worsen hypercapnea.
Q.116. A 60-year-old is on treatment for IHD (ischemic heart disease), HTN (hypertension) and hyperlipidemia. During the night he complains of wheeze and SOB (shortness of breath). Which of the following medicine is responsible for that?
Correct Answer : B
Asthma can be precipitated by beta blockers; in practice it is seen that even cardioselective beta blockers can precipitate or aggravate asthma.
Q.117. A patient presents with progressive dyspnea. He complains of cough, wheeze and a table spoonful of mucopurulent sputum for the last 18m. Spirometry has been done. FEV1/FVC 2.3/3.6. After taking salbutamol, the ratio is 2.4/3.7. What is the most likely diagnosis?
Correct Answer : A
Progressive dyspnoea, wheeze productive cough, and the result of spirometry, prebronchodilator FEV1/FVC ratio of 64% and postbronchodilator FEV1/FVC ratio of 65% points towards the diagnosis of chronic bronchitis. Some may think of bronchiectasis! But in bronchiectasis there is copious purulent sputum (as a cup full of sputum , not table spoon full!)
Q.118. A 62-year-old man presents with cough, breathlessness and wheeze. 24% O2, salbutamol and hydrocortisone were given. The symptoms haven’t improved and so nebulized bronchodilator was repeated and IV aminophylline was given. ABG: pH 7.31, RR 32. What is the next appropriate management?
Correct Answer : A
[Here given case is COPD has the following indications of Nasal IPPV :
i) Tachypnea (>24 breaths/min)
ii) Hypercapnic respiratory acidosis (pH range 7.10-7.35).
Q.119. A 19-year-old man has exercised induced asthma and is using a salbutamol inhaler as required and beclamethasone 400ug BD. He complains that he has to wake up at night for his inhaler. What is the most appropriate tretment?
Correct Answer : D
Leukotriene receptor antagonist
Q.120. A 27-year-old man presents with chest pain and respiratory distress. Examination: tachycardia, hypotension and neck vein distension. Trachea is deviated to the left side, breath sounds on right side are absent and diminished on left side. What is the next appropriate management?
Correct Answer : B
Diagnosis is right-sided massive pneumothorax.
Q.121. An 83-year-old man with longstanding COPD has become progressively breathless over the last 2 years. He is on salbutamol, ipratropium, salmeterol, beclomethasone and theophylline. His FEV1<30%. What is the next appropriate management?
Correct Answer : D
Patient is progressively breathless with present FEV1 of <30%. So his respiratory deterioration indicates progressive respiratory failure for which he should be assessed for long-term O2 therapy.
Long-term oxygen therapy (LTOT) for more than 15 h/day improved mortality and morbidity in a well-defined group of patients with chronic obstructive pulmonary disease. Requirement of condition to proceed to LTOT is patient should be stable and on appropriate optimum therapy (as in the given case) and has stopped smoking tobacco.
FEV1 should be less than 1.5 liters, and there should be a less than 15% improvement in FEV1 after bronchodilators. Patients with a PaO2 between 7.3 and 8 kPa who have polycythemia, right heart failure, or pulmonary hypertension may gain benefit from LTOT.
Q.122. A 33-year-old man has a temperature of 38.5 C, cough and chest pain on the right side on inspiration. He also has purulent sputum. What is the most likely organism to cause pneumonia in this patient?
Correct Answer : A
It is a case of community-acquired pneumonia caused by streptococcus pneumoniae.
Q.123. During a basketball match, one of the players suddenly collapsed to the ground with coughing and SOB (shortness of breath). What is the investigation of choice?
Correct Answer : A
The likely diagnosis is pneumothorax. So investigation of choice is CXR.
Q.124. A tall rugby player was hit in the chest by a player of the opponent team. He developed breathlessness and his face went blue and purple. You have been called to look at him, how will you manage him?
Correct Answer : D
The patient went blue and purple!! It is due to catch up of breath and it is not cyanosis of pneumothorax as cyanosis of pneumothorax takes time to develop and is considered a late feature. Immediate features are chest pain, tachycardia, tachypnea etc.
Q.125. A 64-year-old man complains of increasing SOB (shortness of breath)and cough for the past 18 months. He coughs up a table spoonful of mucopurulent sputum with occasional specks of blood. What is the most likely underlying cause?
Correct Answer : C
There may be specks of blood in sputum in both bronchiectasis and acute and chronic bronchitis. The duration of the disease is 18 months, so it is not acute bronchitis. Again only one tablespoonful of sputum does not justify the term copious sputum of bronhiectasis in which sputum will be much more like cup-full in amount. So it is chronic bronchitis.
Q.126. A 75-year-old man presents with Bell’s palsy. His past medical history is significant for late onset asthma and heart failure. He also reports to have consulted his GP for generalized rash previously. CXR shows multiple soft shadows and CBC eosinophilia. What is the most likely positive antibody?
Correct Answer : A
The diagnosis is Charg Strauss Syndrome (CSS).
There are six criteria for diagnosis of CSS:
Asthma (wheezing, expiratory rhonchi).
Eosinophilia of more than 10% in peripheral blood.
Paranasal sinusitis.
Pulmonary infiltrates (may be transient).
Histological confirmation of vasculitis with extravascular eosinophils.
Mononeuritis multiplex or polyneuropathy.
The presence of four out of six of these features has a high specificity and sensitivity for the diagnosis of CSS.
In the given case there are :
1. Bell’s palsy (mononeuritis multiplex)
2. Asthma
3. Multiple soft shadows on CXR (pulmonary infiltrates)
4. Eosinophilia
The presence of these 4 features is diagnostic of CSS. In CSS 70% of patients are p-ANCA positive!
Q.127. A 68-year-old woman presents to the emergency department with confusion. Temperature 39.3 C and productive cough. Sputum is rusty coloured after 2 days. CXR shows right lower lobe consolidation. What is the most likely organism?
Correct Answer : A
Streptococcus pneumonia
Q.128. A nonsmoker who has worked in coal mines for 20 years presents with gradually increasing SOB (shortness of breath), limited exercise tolerance and a dry cough. His CXR shows round fibrotic tissue demonstrating a mixed restrictive and obstructive ventilator defect with irreversible airflow limitation and reduced gas transfer. What is the most appropriate diagnosis?
Correct Answer : D
Progressive massive fibrosis.
Coal miners pneumoconiosis.
Coal worker's pneumoconiosis (CWP) can be defined as the accumulation of coal dust in the lungs and the tissue's reaction to its presence. Simple coal worker’s pneumoconiosis is usually asymptomatic. Progressive massive fibrosis produces cough, dyspnea, and lung function impairment.
Q.129. A 25-year-old man has been suffering from breathlessness and wheeze for 3 months. He has been taking salbutamol 2puffs as required. In the last 2 weeks his symptoms have worsened and he has to take salbutamol more frequently during the day time. He also complains of excessive dyspnea at night. What drugs or regimen would you like to add?
Correct Answer : C
Beclomethasone inhaled.
Patient was in step 1. As not controlled next step is addition of inhaled corticosteroid.
Q.130. A 12-year-old presents with chest pain. Examination: tachycardia, hypotension, dilated neck veins and the trachea is not centrally placed. What is the next appropriate management?
Correct Answer : B
Needle thoracentesis (A case of tension pneumothorax).
Q.131. A 55-year-old male presents to the emergency department after an RTA (road traffic accident) with breathlessness, engorged neck veins and a dull percussion note on the right side of his chest. Examination: pulse 140 bpm, BP 80/50 mmHg. What is the most likely diagnosis?
Correct Answer : B
Hemopneumothorax.
Dull percussion note indicates the presence of blood. Also, low BP and shock favours more towards hemopneumothorax. Please note in pure hemothorax there is volume depletion so that neck veins do not rise.
Q.132. A 30-year-old woman is taking treatment for asthma. She has a heart rate 130 bpm and peak expiratory flow rate 400. What is the most appropriate management?
Correct Answer : C
Oral beta agonist frequently causes tachycardia and palpitations.
Q.133. A 16-year-old boy came home from boarding school with a cough. His CXR showed bilateral consolidations. What is the most likely organism which would have caused his symptoms?
Correct Answer : B
Mycoplasma pneumonia. Mycoplasma is common in military barracks, prison or boarding dwellers.
Q.134. A young man returns to his hostel and gets headache and lethargy. Now presents with fever. There are crepitations on the auscultation of lung. What is the most likely organism which would have caused his symptoms?
Correct Answer : A
Legionella is common in hostels, hotels, hospitals, and nursing homes where it spreads through their water system, air condition, etc.
Q.135. A 24-year-old male is admitted with acute severe asthma. Treatment is initiated with 100% oxygen, nebulized salbutamol and ipratropium bromide nebulizers and IV hydrocortisone. Despite initial treatment there is no improvement. Which is the next step in management?
Correct Answer : B
If the patient not improving after 15-30 minutes above treatment:
Continue oxygen and steroids.
Use continuous nebulization of salbutamol at 5-10mg/hour if a specialist nebulizer is available. Otherwise, give nebulized salbutamol 5mg every 15–30 minutes. Continue ipratropium 0.5mg 4–6 hourly until the end is improving.
IF PATIENT IS STILL NOT IMPROVING: Consider IV magnesium sulfate 1.2–2g over 20 minutes.
Q.136. A house-bound 78-year-old man with severe COPD has had a gradual deterioration over recent months and is now breathless at rest. He is on maximal inhaled medical therapy. Result: pH 7.36, PaCO2 5.9kPa, PaO2 6.9kPa. What is the most appropriate additional treatment?
Correct Answer : D
In patients with chronic hypoxemia, LTOT should usually be prescribed after appropriate assessment, when the PaO2 is consistently at or below 7.3 kPa (55 mm Hg) when breathing air during a period of clinical stability.
Clinical stability is defined as the absence of exacerbation of chronic lung disease for the previous five weeks. The level of PaCO2(which may be normal or elevated) does not influence the need for LTOT prescription.
Q.137. A 16-year-old boy in boarding school feels unwell. He developed cough and rash. His CXR showed bilateral consolidations. What is the cause of his symptoms?
Correct Answer : C
Rash, bilateral consolidation favours mycoplasma pneumonia. Mycoplasma is common in military barracks, prisons, or boarding dwellers.
Q.138. A man suffering from Influenza A since 5 days ago. CXR: pneumonia. What organism is responsible for pneumonia in this patient?
Correct Answer : C
Post flu pneumonia is usually caused by staphylococcus aureus.
Q.139. A 35-year-old man has been diagnosed as allergic rhinitis and asthma. Examination: peripheral neuropathy with tingling and numbness in a ‘glove and stocking’ distribution. Skin lesions are present in the form of tender subcutaneous nodules. The patient is responding well to corticosteroids. What is the most appropriate diagnosis?
Correct Answer : B
Churg-Strauss syndrome.
The American College of Rheumatology has identified six criteria for the diagnosis of CSS :
• Asthma (wheezing, expiratory rhonchi)
.• Eosinophilia of more than 10% in peripheral blood.
• Paranasal sinusitis
• Pulmonary infiltrates (may be transient)
• Histological confirmation of vasculitis with extravascular eosinophils
• Mononeuritis multiplex or polyneuropathy
The presence of four out of six of these features has a high specificity and sensitivity for the diagnosis of CSS.
Q.140. A 49-year-old man comes with history of cough and SOB. His CD4 count is measured as 350. CXR shows lobar consolidation. What is the most appropriate option?
Correct Answer : C
Though CD4 count indicates immunodeficiency syndrome features are consistent with lobar pneumonia.
Q.141. A 40-year-old patient came to OPD with complaint of fever, pleuritic chest pain, productive cough and painful vesicles around the lips. Exam: temp 38C. He has a history of splenectomy last year. What is the most likely causative organism?
Correct Answer : A
Pneumococcal pneumonia is the most common pneumonia in splenectomized patients. Painful vesicles around the lips are a well-known association of pneumococcal pneumonia. Also, pleuritic chest pain and productive cough are present in pneumococcal pneumonia.
Q.142. A 37-year-old male patient who recently returned back to UK from UAE attends the OPD with complaint of dry cough, breathlessness and anorexia. According to him he had flu like symptoms a week ago. He is slightly confused. Investigations: lymphopenia & decreased Na+. CXR: bi-basal consolidation. What is the most likely causative organism?
Correct Answer : A
H/O travel (staying in AC and water-system of hotel), lymphopenia, decreased Na+ and confusion are well-known features of legionnaires disease.
Q.143. A 20-year-old student came to the OPD with complains of headache, malaise, dry cough, joint pain and vomiting. Examination: temperature 39C. CXR: patchy consolidation. What is the most likely causative organism?
Correct Answer : B
Headache, dry cough, joint pain these are more pronouncedly commoner in mycoplasma pneumonia.
Q.144. A man with chronic cough presents with copious purulent sputum. What is the most likely diagnosis?
Correct Answer : B
Chronic cough with copious purulent sputum is suggestive of bronchiectasis.
Q.145. A 25-year-old patient came to the OPD with complaint of fever, malaise, breathlessness, cough and anorexia. His girl friend has got similar symptoms. He had history of sore throat and ear discharge a month ago. What is the most likely causative organism?
Correct Answer : C
Please note sore throat is a clue for chlamydia as well as about 4 weeks prior exposure history is also a pointer.
Q.146. A 50-year-old DM patient came to the OPD with complaint of fever, muscle ache, dry cough and anorexia. Investigation: CXR shows upper lobe cavitation. What is the most likely causative organism?
Correct Answer : D
Upper lobe cavitation favours Klebsiella pneumonia. Also, it is well known that klebsiella pneumonia is more common in DM than in normal persons.
Q.147. 29-year-old woman who returned from Egypt 2 weeks ago now presents with difficulty in breathing, chest pain, cough and purulent sputum with an episode of blood staining. She is on COCPs. What is the most likely diagnosis?
Correct Answer : B
Purulent sputum is the clincher to differentiate pneumonia from pulmonary embolism here.
Q.148. An 83-year-old elderly woman presented in the emergency department with cough, fever and sneezing. Treatment was given but she became confused and again presented with above said symptoms. What is the cause of her condition?
Correct Answer : A
Aspiration pneumonia is a common disease that frequently occurs in elderly patients. Most patients with aspiration pneumonia have a swallowing disability which worsens in patients with confusion.
Q.149. A 37-year-old man presents with some raised lesions on the shin. He came with cough and also complains of arthralgia. Examination: bilateral hilar lymphadenopathy and erythema nodosum is present. What is the most likely cause?
Correct Answer : C
Cough, arthralgia, bilateral hilar lymphadenopathy, and erythema nodosum are suggestive of sarcoidosis.
Q.150. A patient who works in a pet shop has temperature of 37.5C, dyspnea, chest pain and cough. CXR: patchy consolidation. What is the most suitable treatment?
Correct Answer : D
Clarithromycin.
Q.151. An 83-year-old woman admitted with a chest infection becomes confused with impaired attention and poor concentration. She is restless and frightened. She is verbally abusive and has perceptual abnormalities. There is no significant previous psychiatric history. What is the most likely diagnosis?
Correct Answer : A
Delirium or Acute Confusional State happens in the elderly in response to stressors like acute infections and this is most likely brought on by the chest infection that has developed.
Q.152. A 20-year-old previously healthy woman presents with general malaise, severe cough and breathlessness which has not improved with a seven day course of amoxycillin. There is nothing significant to find on examination. The x-ray shows patchy shadowing throughout the lung fields. The blood film shows clumping of red cells with suggestion of cold agglutinins. What is the most likely diagnosis?
Correct Answer : B
Inability to respond to a seven-day course of amoxicillin suggests atypical pneumonia, patchy shadows throughout lung fields, and cold agglutination points towards mycoplasma.
Q.153. A patient with chronic neutropenia develops a chronic cough. A CXR reveals a cavitating intrapulmonary lesion containing a movable rounded ball lesion. What is the likely diagnosis?
Correct Answer : A
Mostly affects people with reduced immunity, reduced neutrophil count is also a predilection for aspergillosis.
Q.154. A 29-year-old Afro-Caribbean man presents with a non-productive cough mild aches in the ankles. The symptoms have been present for 2 months. His ESR is elevated. Ca: 2.69 mmol/l; PO4 -: 1.20 mmol/l; ALP: 80 iu/L. Serum 25(OH) D: 180 nmol/l Normal values for Calcium: 2.12-2.65mmol/l; Phosphate: 0.8-1.45mmol/l; ALP 30- 300iu/L; Serum 25(OH) D: 20-105nmol/l; Urea: 2.5-6.7mmol/l; Creatinine: 70- 120mmol/l. What is the diagnosis?
Correct Answer : C
Sarcoidosis.
Q.155. A 7-year-old boy with frequent episodic asthma is on treatment with sodium cromoglycate. His physician wants to add a non-steroid preventer. The mother of the boy, a teacher, has just read about a nonsteroidal medication which acts on the mast cells, stopping them from releasing harmful chemicals. Her physician agrees to add this medication to the boy's drug regimen. Which medication is the physician most likely to add to the boy's treatment?
Correct Answer : C
Nedocromil sodium
Q.156. A 70-year-old woman presents with confusion and productive cough. CXR shows right lower lobe consolidation. What is the most likely causative organism?
Correct Answer : C
We know aspiration pneumonia in the elderly may be community-acquired. Streptococcus pneumoniae predominates in community-acquired cases, (those who are not hospitalized- as for presenting case), and Staphylococcus aureus and Gram-negative organisms predominate in hospital-acquired cases.
Q.157. A pet shop owner presents with high swinging fever, cough and malaise. He has scanty rose spots over his abdomen. CXR reveals diffuse pneumonia, What is the most likely causative organism?
Correct Answer : A
Chlamydia psittaci
Q.158. A 70-year-old alcoholic man presents with sudden onset of purulent productive cough. CXR shows consolidations left upper lobe. What is the most likely causative organism?
Correct Answer : D
Klebsiella pneumoniae is the prevalent organism in alcoholics (but recent studies have shown that Streptococcus pnemoniae is the leading cause)
Q.159. A 10-year-old boy with cystic fibrosis presents with pneumonia. What is the most likely causative organism?
Correct Answer : A
In infancy Staphylococcus aureus is the predominant organism and later Pseudomonas aeruginosa becomes the predominant one in children with the disease cystic fibrosis.
Q.160. A 30-year-old man with AIDS presents with fever, dry cough and dyspnoea, CXR shows diffuse bilateral alveolar and interstitial shadowing beginning in the perihilar regions and spreading outward, What is the most likely causative organism?
Correct Answer : B
Pneumocystis carinii also known as Pneumocystis jirovecii is a yeast-like fungus. Pneumocystis specimens are commonly found in the lungs of healthy people although it is usually not a cause for disease.
However, they are a source of opportunistic infection and can cause lung infections in people with a weak immune system or other predisposing health conditions.
PCP is seen in people with HIV/AIDS, those using medications that suppress the immune system, and people with cancer, autoimmune or inflammatory conditions, and chronic lung disease.
Q.161. A 26-year-old man presents to the A & E department with shortness of breath of 3 days duration. He has been coughing during the night and using his salbutamol inhaler more frequently. What is the most appropriate investigation?
Correct Answer : A
Arterial blood gases are valuable for assessing the severity of exacerbations and following response to treatment. It is useful to differentiate between type 1 and type 2 respiratory failure.
Q.162. A 22-year-old man presents to the A & E with sudden onset of sharp right-sided chest pain and shortness of breath. There is reduced air entry in the right side of the chest. What is the most appropriate investigation?
Correct Answer : D
Features (sudden chest pain with shortness of breath, reduced air entry) are consistent with pneumothorax for which Chest X-ray is the investigation of choice.
Q.163. A 78-year-old woman is brought by her family to the A & E department with shortness of breath and occasional cough over the previous 72 hours. There is a coarse crepitation present at the right lung base. What is the most appropriate investigation?
Correct Answer : B
Probable pneumonia. Chest X-ray should be done.
Choose a Question
×Choose a Question
×
Trial Access Limit Reached
You’ve reached the limit of free content. Subscribe to continue learning without restrictions.