

Hello,
Dr. Batman
Hello Doctor, Welcome!
Profile

Name: Batman
Email: batman@gotham.com
VASCULAR SURGERY
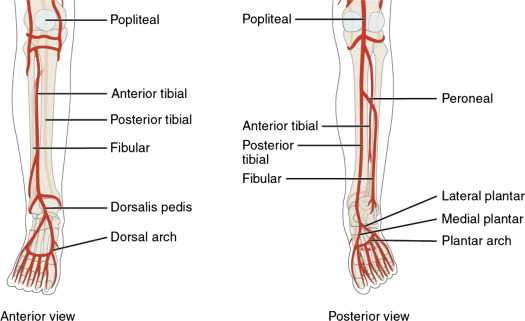
(Total Questions - 21)Q.1. A 55 year old smoker presents to the emergency department with complaint of severe left leg and foot pain that began earlier in the day. The pain spreads to the level just above the inguinal ligament. His past medical history includes hypertension. On examination, he has atrophic skin changes in his left leg and his left limb is cold to touch. He has no palpable pulses in the left lower extremity. Gross motor and sensory functions were intact in the symptomatic leg and foot. What is the most likely occluded artery?
Correct Answer : B
The answer here is the left common iliac artery. The femoral artery and deep femoral artery are less likely as the pain would start below the inguinal ligament. The external iliac artery becomes the femoral artery after it passes under the inguinal ligament.
Hence the occlusion would be above the inguinal ligament.If it was a femoro-popliteal artery occlusion, the pain would be described below the knee.The option of aortoiliac artery occlusion is not specific as it does not state if it is right or left.
It would also have symptoms of claudication and pain in the buttocks and thighs. Symptoms of erectile dysfunction can also be seen in aortoiliac artery occlusion.
The ideal answer would be an external iliac artery occlusion as there are no symptoms of gluteal pain in the stem. The common iliac bifurcates into internal and external iliac arteries and since there is no mention of symptoms of internal iliac artery obstruction in the stem, an external iliac artery occlusion would be the best option if it was given in the exam.
However, since it is not an option given, common iliac artery occlusion falls into the first place as the answer.
Remember, symptoms of occlusion have to occur distal to the level of the occlusion.
Q.2. A 76 year old man suddenly collapsed and died. At postmortem exam, a retroperitoneal haematoma was found due to ruptured abdominal aortic aneurysm. What is the most likely underlying aetiology of the aortic aneurysm?
Correct Answer : A
There are many causes of aortic aneurysm but the most typical cause of an aortic aneurysm is atheroma.
Abdominal Aortic Aneurysms :
Risk factors -
• Severe atherosclerotic damage of the aortic wall
• Family history
• Male sex
• Increasing age
• Hypertension, smoking
• Syphilis
• Ehlers Danlos
• Marfan’s syndrome
Q.3. A 28 year old construction worker was admitted for pain in his right calf while at work which has been increasing over the last 3 months. There is no history of hypertension or diabetes, but he is a smoker. On examination, loss of posterior tibial and dorsalis pedis pulsation was noticed along with a non-healing ulcer at the base of the right 1st metatarsophalangeal joint. What is the most probable diagnosis?
Correct Answer : A
The diagnosis here is thromboangitis obliterans (Buerger’s disease). It usually presents in young men around 40 years old with a strong smoking history.
This particular question might be a little confusing and some might argue that an embolus could have caused an acute limb ischaemia causing admission.
But given his young age, smoking history, chronic pain that was increasing over a long period, and a nonhealing ulcer, Buerger’s disease fits better.
Thromboangitis obliterans (Buerger’s disease) : Involves small vessels of the lower limbs and occurs in young men who smoke. It is thought by some workers to be indistinguishable from atheromatous disease.
However, pathologically there is inflammation of the arteries and sometimes veins that may indicate a separate disease entity.
Clinically, it presents with severe claudication and rest pain. Treatment is for all peripheral vascular diseases, but patients must stop smoking.
Q.4. A 62 year old man has a painless swelling on his groin. On examination, the mass lies below the midpoint of the right inguinal ligament and is pulsatile. What is the most likely diagnosis?
Correct Answer : D
The two top differentials here are the femoral artery aneurysm and femoral hernia. As the mass is pulsatile, it can only be a femoral artery aneurysm. A femoral hernia appears below and lateral to the pubic tubercle, medial to femoral pulse and it is not pulsatile.
Femoral artery aneurysm :
• A less common type of aneurysm
• Rarely symptomatic
• Usually discovered on routine examination by a physician
• May experience a pulsating lump or swelling on the thigh or radiating pain
• Rarely causes numbness in legs due to nerve compression
Q.5. A 60 year old man has sudden severe chest pain radiating to both shoulders and accompanied by shortness of breath. There was no history of trauma. His medical history includes hypertension. Examination shows cold peripheries and paraplegia. What is the most appropriate diagnosis?
Correct Answer : B
This is a typical case. A man in his 60s with hypertension and sudden onset of chest pain. The majority of patients with aortic dissection, present with a sudden severe pain in the chest or back, classically described as 'ripping'. The cold peripheries are due to reduced blood flow to the distal parts of dissection.
Paraplegia is due to the involvement of the spinal arteries. Sometimes questions would also give a difference in blood pressure in limbs on the right and left side of the body.
Thoracic Aortic Dissection - Dissecting aneurysm of the thoracic aorta : Occurs in the poorly controlled hypertensive. The episode resembles an Ml, with a sudden onset of extremely severe, tearing chest pain that radiates to the back and migrates down shortly after its onset. There may be unequal pulses in the upper extremities, and X-rays show a wide mediastinum.
ECG and cardiac enzymes rule out Ml.
MRI angiogram and transesophageal echocardiogram have been used, but the best option is probably a spiral CT scan. As a rule (riddled with exceptions), dissections of the ascending aorta are treated surgically, whereas those in the descending are managed medically with the control of hypertension in the ICU.
Stanford classification -
Type A :
• Ascending aorta, 2/3 of cases
• Surgical management, but blood pressure should be controlled to a target systolic of 100-120 mmHg whilst awaiting intervention
Type B :
• Descending aorta, distal to left subclavian origin, 1/3 of cases
• Conservative management
• Bed rest
• Reduce blood pressure IV labetalol's to prevent progression
Risk factors -
• Approximately 50-75% of patients with dissection will have evidence of hypertension or a previous diagnosis.
• Other risk factors include smoking and raised cholesterol.
The most common risk factor is hypertension.
• Inherited risks include Marfan's syndrome, Ehlers-Danlos syndrome, and familial thoracic aortic aneurysm
Remember: The most common risk factor is hypertension.
Q.6. A 27 year old man attends the GP surgery with complaints of headaches, nose bleeds and pain in the lower limbs on exertion. A radio-femoral delay was noted on examination. His legs are cold and his femoral pulse is difficult to feel. Auscultation reveals a systolic murmur heard in the left infraclavicular area. What is the most likely diagnosis?
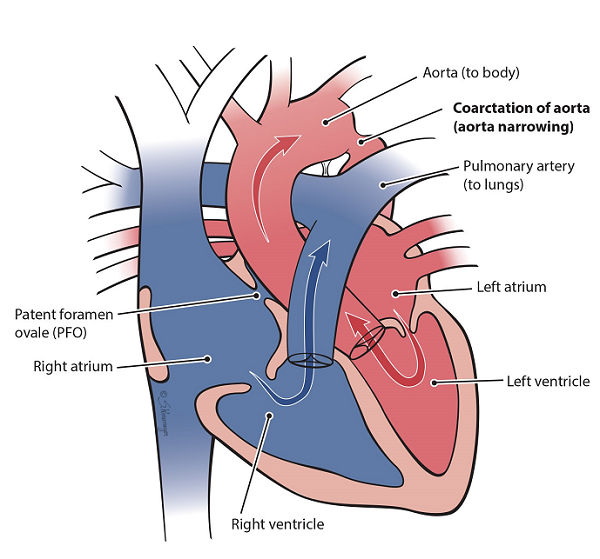
Correct Answer : C
This stem shows a late presentation of coarctation of the aorta suspected when patients have refractory hypertension. In this stem, the blood pressure was not mentioned but he has all the other symptoms one can expect for coarctation of the aorta.
Q.7. A 45 year old man presents to the Emergency Department with sudden excruciating pain in the right leg. On examination, his right lower limb is pale and cold. The dorsalis pedis and posterior tibial pulses are absent in the right foot. He has a pulse of 95 beats/minute with an irregular rhythm. What is the most likely reason for his pain?
Correct Answer : D
This irregular pulse indicates a likely atrial fibrillation which has led to a thrombus forming and dislodging into the arteries that supply the right leg. Acute limb ischaemia • Is a surgical emergency requiring revascularization within 4 to 8 hours to save the limb. It is usually due to thrombosis in situ, emboli, or graft occlusion. • Emboli commonly arise from the heart (Atrial fibrillation; mural thrombus) or aneurysms.
Symptoms and signs: The 6 ‘P’S of acute ischaemia: pale, pulseless, painful, paralyzed, paraesthetic, and perishingly cold’.
In patients with known peripheral arterial disease (PAD), sudden deterioration of symptoms with deep duskiness of the limb may indicate acute arterial occlusion. Management: This is an emergency and may require urgent open surgery or angioplasty.
Q.8. A 60 year old presents with non-healing ulcers on his calves and a cramp-like pain in the calves relieved by rest. His past medical history includes hypertension, diabetes, and hypercholesterolaemia. He also smokes 15 cigarettes a day. Physical examination shows cold extremities, absent distal pulses. Which advice is unlikely to prevent disease progression?
Correct Answer : D
The diagnosis here is clear – Peripheral arterial disease. The history of intermittent claudications and non-healing ulcers are key features of it. Quit smoking is vital. Treat hypertension and high cholesterol and encourage patients to exercise to the point of maximal pain.
PERIPHERAL ARTERIAL DISEASE (PAD) Peripheral arterial disease (PAD) occurs due to atherosclerosis causing stenosis of arteries. This leads to intermittent claudication. Pain comes on walking and after a short rest, it goes away.
Symptoms– Depend on the severity • Intermittent claudication which is cramping pain felt in the calf, thigh, or buttock after walking a distance and relieved by rest. • Rest pain – For more severe cases • Ulceration and gangrene – If continues to progress Signs • Absent femoral, popliteal, or foot pulses.
Risk factors: • Hypertension • Diabetes Mellitus • Smoking • High cholesterol Investigations • Doppler ultrasound – 1st line. Used to measure the pressure at which detectable flow ceases using a compression cuff to determine the ankle-brachial index (ABPI) • Colour flow duplex ultrasound. Assesses stenosis of the vessel • MR/CT angiography. Used only if considering intervention. Used to assess the extent and location of stenoses and quality of distal vessels. o MRI/CT angiography has largely replaced digital subtraction angiography.
Management:
• Address risk factors for cardiovascular disease o Quit smoking (vital). Treat hypertension and high cholesterol. Prescribe an antiplatelet agent to prevent progression and reduce cardiovascular risk. (Clopidogrel is recommended as 1st-line)
• Encourage patients to walk beyond the distance at which pain occurs
• Naftidrofuryl oxalate - Only if the patient does not want revascularization and if exercise fails to improve symptoms If severely affecting the patient's life and disease limited to a single arterial segment.
Percutaneous transluminal angioplasty (PTA) (a balloon is inflated in the narrowed segment). If severely affecting the patient's life and atheromatous disease is extensive distal run-off is good (i.e. distal arteries filled by collateral vessels). Surgical reconstruction: consider arterial reconstruction with a bypass graft One of the important differential diagnoses is thromboangiitis obliterans (Buerger's disease). usually in young men around 40 years old with a strong smoking history.
Thromboangiitis obliterans (Buerger's disease): Involves small vessels of the lower limbs and occurs in young men who smoke.
• It is thought by some workers to be indistinguishable from atheromatous disease. However, pathologically there is inflammation of the arteries and sometimes veins that may indicate a separate disease entity.
Clinically, it presents with severe claudication and rest pain. Treatment is for all peripheral vascular diseases, but patients must stop smoking.
Q.9. A 78 year old man has a painless sudden collapse. His pulse is 120 beats/minute, blood pressure of 70/40 mmHg. Examination reveals a mottled skin of the lower body and a pulsatile abdominal mass. What is the most likely diagnosis?
Correct Answer : A
A “pulsatile abdominal mass” is the key phrase for abdominal aortic aneurysm. One should be able to answer this in less than 3 seconds.
Q.10. A 31 year old woman with confirmed disseminated renal carcinoma presents with bilateral, pitting, non-tender leg swelling up to the groin. She was also found to have dilated lower abdominal veins. What is the most likely cause for her symptoms?
Correct Answer : B
Inferior vena cava syndrome varies in its clinical presentation however, a well-established cause for inferior vena cava syndrome is renal cell carcinoma. When the tumor obstructs the inferior vena cava, it results in marked fluid retention below the obstruction and pitting edema of the lower extremities.
While it is also true that right-sided heart failure can cause these symptoms, no other clue as to the diagnosis of right heart failure exists besides the edema and dilated abdominal veins.
Indeed, the examiners were probably trying to trick you into choosing the right heart failure by putting in dilated lower abdominal veins. Dilated lower abdominal veins can also exist as a result of inferior vena cava syndrome.
Inferior vena cava syndrome presents with a wide variety of signs and symptoms, making it difficult to diagnose clinically but edema of the lower extremities and tachycardia are frequently seen. There are no additional caveats in the stem that point toward any of the other answers.
INFERIOR VENA CAVA SYNDROME Inferior vena cava syndrome are symptom resulting from an obstruction of the inferior vena cava. This can be caused by
• Physical invasion (tumors most commonly renal cell carcinoma)
• Compression (seen in a pregnant woman who lies in a supine position)
• Thrombosis (within the vein itself) Symptoms
• Oedema in the lower extremities
• Tachycardia.
Q.11. A 68 year old lady is brought to the emergency department complaining of severe substernal pain which started suddenly. She is known to suffer from hypertension and diabetes. On examination, her pulse is 120 beats/minute and her blood pressure is 90/30 mmHg. Breath sounds are normal on both sides. Her pain is not responding to oral nitrates. What is the most likely diagnosis?
Correct Answer : A
The two top differentials in this case are acute aortic dissection and acute myocardial infarction. The presence of hypotension in combination with the absence of any response to oral nitrates points towards a likely diagnosis of aortic dissection.
Q.12. A 40 year old heavy smoker presents with pain in the calves relieved by rest. These symptoms have been worsening over the last few months. He has a history of hypertension which is well controlled with medication. His distal pulses are difficult to palpate. What is the most likely diagnosis?
Correct Answer : D
The diagnosis here is thromboangitis obliterans (Buerger’s disease). It usually presents in young men around 40 years old with a strong smoking history.
Q.13. A 55 year old man comes to the emergency department with severe abdominal pain and lower back pain. He has a history of a pulsatile swelling in the abdomen. He has a pulse rate of 125 beats/minute and a blood pressure of 70/40 mmHg. What is the most appropriate initial management?
Correct Answer : C
This scenario describes a ruptured aortic aneurysm. Immediate intravenous normal saline to raise the blood pressure to 90 mmHg to keep the vital organs perfused till definitive measures are taken. The idea here is to treat major hypovolaemia but accept moderate degrees of hypotension which is a systolic BP > 90 mmHg.
In such a given case, assume that the problem is a ruptured abdominal aortic aneurysm and commence resuscitative measures, whilst appropriate experts are summoned and relevant emergency confirmatory investigations like an ultrasound or CT scans are performed.
Q.14. A 44 year old man has sudden severe crushing chest pain radiating to both shoulders and his back. The pain is accompanied by shortness of breath. He is sweating profusely. There was no history of trauma. Examination shows cold peripheries. He is noted to have disproportionately long, slender limbs and long fingers and toes. What is the most appropriate diagnosis?
Correct Answer : B
The signs and symptoms in this stem point towards an aortic dissection. The majority of patients with aortic dissection present with a sudden severe pain in the chest or back, classically described as ‘ripping’. The cold peripheries are due to reduced blood flow to the distal parts of dissection.
Disproportionately long, slender limbs and having long fingers and toes given in this stem is a hint that he probably has Marfan syndrome which is an added risk factor towards aortic dissection.
Sometimes EXAM questions would also give a difference in blood pressure in limbs on the right and left side of the body.
Q.15. A 60 year old diabetic presents with non-healing ulcers on his calves and a cramp-like pain in the calves relieved by rest. He does not smoke, but has a history of hypertension which is well controlled with medication. Physical examination shows cold extremities with lack of heair around the ankles and absent distal pulses. What is the most likely diagnosis?
Correct Answer : B
The diagnosis is Peripheral arterial disease. The history of intermittent claudication and non-healing ulcers are key features of it.
The other options are quite unlikely: Acute limb ischaemia is acute! The 6 ‘P’S of acute ischaemia: pale, pulseless, painful, paralyzed, paraesthetic, and ‘perishingly cold’. Buerger’s disease.
Needs a history of smoking, usually in a younger aged patient with Deep vein thrombosis. Pain or tenderness is constant and not of an intermittent claudication pattern.
Also does not present with non-healing ulcers or Varicose veins. Do not have an intermittent claudication pattern pain. They usually come in saying “My legs are ugly”
Q.16. A 49 year old man presents with a BP of 160/95 mmHg. He is otherwise asymptomatic. His renal function declined severely after starting ACE inhibitors. What is the most likely cause of his hypertension?
Correct Answer : D
When someone is started on ACE inhibitors, urea and electrolytes are usually checked 7 to 10 days after starting treatment, and at least annually. Should a patient’s renal function deteriorate after initiation, the diagnosis of renal artery stenosis should be considered. Renovascular disease: Renovascular disease is defined as stenosis of the renal artery or one of its branches. The two main causes are atherosclerosis and fibromuscular dysplasia.
Signs: BP resistant to treatment; worsening renal function after ACE-i/ARB in bilateral renal artery stenosis Tests:
• USS: renal size asymmetry (affected side is smaller), disturbance in renal blood flow on Doppler US.
• CT/MR angiography is more sensitive.
• Renal angiography is the ‘gold standard’,
but do after CT/MR as it is invasive Treatment:
• Comprehensive antihypertensive regimens, transluminal angioplasty ± stent placement, or revascularization surgery.
Note: Severe decline in renal function may be observed in patients with bilateral renal artery stenosis after initiation of ACE inhibitors.
Q.17. A 68 year old man gets repeated attacks of loss of consciousness and transient ischaemic attacks (TIA). What is the most likely cause for his symptoms?
Correct Answer : D
Carotid artery stenosis would fit this picture perfectly. The plaque can be stable. As the vessel gets smaller, they can lodge in the vessel wall and restrict blood flow to parts of the brain which that vessel supplies. This ischaemia can either be temporary, yielding a transient ischaemic attack, or permanent resulting in a thromboembolic stroke. In this case, it caused a TIA and loss of consciousness.
Q.18. A 38 year old woman presents with a blood pressure of 160/90 mmHg. She is otherwise asymptomatic. Ultrasound scan of kidneys reveal kidneys of equally reduced size with smooth borders and normal pelvicaliceal system. What is the most likely cause of her hypertension?
Correct Answer : B
The likely diagnosis here is fibromuscular dysplasia which is a form of renovascular disease. Often fibromuscular dysplasia involves both renal arteries and usually presents with a high blood pressure resistant to treatment.
The patients are otherwise asymptomatic. Atrophic kidneys or discrepancies in kidney sizes are clues that give off the diagnosis of renal artery stenosis. No mention was given regarding the discrepancy in kidney size in this stem, likely because both renal arteries are stenosed rather than just one.
Q.19. A 70 year old smoker presents with an acutely painful, pale paralysed and pulseless left leg. He is noted to have an atrial fibrillation that was diagnosed recently. He has a pulse rate of 105 beats/minute. What is the most likely diagnosis?
Correct Answer : D
Please see Q-7
Q.20. A 62 year old male presented to Accident & Emergency with the complaint of sudden, severe back pain. His medical history includes hypertension and type 2 diabetes mellitus. He was found to be hypotensive with the presence of a pusatile abdominal mass. The patient was subsequently determined to have an expanding abdominal aortic aneurysm and the decision was taken to immediately rush him for emergency surgery. Unfortunately, he died on his way to theatre due to a ruptured aneurysm. What is the most likely underlying cause for his aneurysm?
Correct Answer : D
The underlying cause for true aneurysms most often is atherosclerosis-related. Atherosclerosis reduces the elastic recoil in the aortic wall as well as causes degenerative ischaemic changes, which predisposes to aneurysms. Aneurysms may be associated with infective causes such as mycotic aneurysms while other aneurysms may be due to collagen and elastin abnormalities which are found in Marfan’s and Ehlers-Danlos syndromes.
Although aneurysms may occur secondary to these, it is not as common as atherosclerosis, especially given the history of hypertension and diabetes mellitus given in this stem.
Q.21. A 51 year old man has cramping pain felt in his calves when he walks up the hill. The pain resolves within a few minutes of resting. This has been ongoing for the past 6 months. On examination, his popliteal and foot pulses are present but weak. There are no ulcers noticeable on his lower limbs. There is no weakness or numbness in his legs. His recent total cholesterol level shows a level of 5.0 mmol/L (normal is < 5 mmol/L). His blood pressure is 138/89 mmHg. He has a body mass index (BMI) of 24.9 kg/m2. He is a non-smoker. He has no known medical conditions. What is the most appropriate advice to give him for secondary prevention of cardiovascular disease?
Correct Answer : A
Guidelines recommends offering stains without the need for a formal risk assessment for all people with established cardiovascular disease (CVD) (which includes peripheral artery disease). For secondary prevention atorvastatin 80 mg would be the drug of choice. Cardiovascular disease risk factors such as high blood pressure need to be addressed, however, in this patient, his blood pressure is within the normal range.
He would not require any antihypertensive medication at this point. A healthy diet, increased physical activity, and weight, if overweight, should also be recommended.
These recommendations should be in combination with statin treatment.
It is important NOT to delay statin treatment whilst managing cardiovascular disease risk factors.
In any case, his BMI is 24.9 kg/m2 which is in a healthy range.
Other important advice for this patient in line with guidelines would be to commence antiplatelet therapy – clopidogrel 75 mg daily (aspirin 75 mg daily if clopidogrel not tolerated)
Choose a Question
×Choose a Question
×
Trial Access Limit Reached
You’ve reached the limit of free content. Subscribe to continue learning without restrictions.